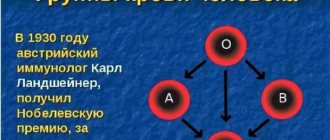
Blood group, like the Rh factor, are permanent indicators of the human body. And their basis is genetically laid from the moment of the beginning of intrauterine life. However, there are often reports that, under various circumstances, a person blood type changes. Why is this possible and is it dangerous for our health? Or is this process completely normal? Let's find out...
You can read about what blood groups exist in nature and what the Rh factor is in this article.
Changes in blood type over the course of life
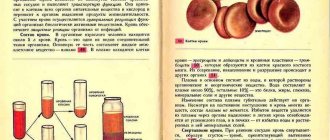
Situations where the blood type changes spontaneously and seemingly for no apparent reason are practically unknown to medicine. The bone marrow of a healthy person is programmed by DNA code to produce the same type of blood cells for life. At the same time, special protein antigens are located on each red blood cell, which make it possible to determine Rhesus status and classify blood into group 1, 2, 3 or 4.
Doctors unanimously say that in a healthy person it is impossible to change the blood type and Rh factor over the course of life.
When such cases appear, there is nothing left to do but attribute the result to diagnostic errors . If a change in blood group was detected during repeated laboratory tests, then one should look for good reasons for this.
Why does the Rh factor change?
The proteins responsible for determining the Rh factor “live” on the membrane of red blood cells. That is why, in the case of a strong increase in the number of red cells in the plasma, the analysis may show not only the wrong group, but also the wrong Rh factor, which actually exists. In addition, the results of laboratory tests may be distorted if there are proteins in the body that, in certain circumstances, demonstrate the same characteristics as the substances responsible for “positive” Rh.
In addition, in the history of modern medicine, there is one case of a change in the Rh factor, which has not yet found a scientific explanation. Nine-year-old girl Demi Lee Brennan underwent a liver transplant, after which her blood turned from the first “negative” to the first “positive”. But world medicine knows no more such cases [4].
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Changes in blood type during pregnancy
Most often, reports of changes in blood grouping come from pregnant women who are registered at the antenatal clinic and periodically donate blood for analysis. Indeed, blood type can change during pregnancy . However, it is very important to note that this is a false shift .
It is due to the fact that the expectant mother’s body increases the production of red blood cells. At the same time, due to accelerated hematopoiesis, it is possible to form blood cells that have a small amount of group antigens on their surface or are completely absent. At this point, a blood group test may show a false result.
This is extremely important. After all, if a pregnant woman needs a blood transfusion, it must be carried out according to the “old” blood group (which was determined before pregnancy). Otherwise, a hemagglutination reaction may occur, i.e. red blood cells stick together and precipitate. This situation is life-threatening for both the mother and the fetus.
Forms of hemolytic pathology:
| Forms | Description |
| Anemic | When a baby has a low level of hemoglobin and an increased level of unconjugated bilirubin. The condition does not entail any serious consequences and is easily normalized. |
| Jaundice | Occurs due to severe bilirubin intoxication. |
| Edema | The most dangerous form of HDN, leading to the death of the fetus in the womb. If the child manages to survive, then a number of pathologies are detected, including damage to the brain and central nervous system. |
The state of red blood cell hemolysis is characterized by the destruction of the red blood cell membrane and the release of hemoglobin into the plasma fluid. Released hemoglobin in large quantities has a poisonous effect on the body.
Therefore, simultaneously with poisoning and overload of the fetal body with bilirubin and other substances, such a pathology also entails anemia.
The liver does not have time to neutralize free bilirubin on a large scale. And this substance in a neurotoxic form wanders throughout the body of the embryo, disrupting oxidative processes in organs and tissues. This leads to irreversible, destructive consequences, including the death of the child. For this reason, the danger of blood substance group conflict during pregnancy should not be underestimated.
Changing blood group in pathological conditions
Potentially, the blood type and Rh factor can also change in various genetic and infectious diseases that lead to hematopoietic disorders and direct damage to red blood cells:
- Blood diseases (thalassemia);
- Bone marrow tumors (leukemia, hemoblastosis, hematosarcoma);
- Viral infections (HIV and AIDS, viral hepatitis);
- Bacterial infections (plague, yellow fever, typhus);
- Parasitic infections (malaria);
- Poisoning with chemicals (nitrates, nitrites, aniline dyes, acids, ethers, gasoline, ethyl alcohol).
The red blood cells of each person have individual sensitivity to the listed damaging factors. Therefore, in such diseases, changing the blood group or Rh factor is possible, but not mandatory . However, such changes are temporary. After recovery, the hematopoietic system should produce full-fledged blood cells that a person had before his illness.
What else could cause change?
Blood type can only be determined through laboratory analysis. To do this, the sample is mixed with sera containing different types of antibodies and it is observed in which cases the red blood cells stick together. But sometimes during such analysis you can get the wrong result. One of the reasons, although not the only one, is the laboratory assistant’s mistake. But there are cases when the analysis was carried out correctly, but still shows completely different data than was previously obtained. In such cases, they do not speak of a change of group, but of a distortion of the results of the analysis. And this can happen for a number of objective reasons.
Infection
Against the background of some infectious diseases, the body produces specific enzymes that, entering the blood, cause the splitting off of part of antigen A, due to which it acquires the characteristics of antigen B. This process does not affect the composition of the plasma in any way, but if an analysis is done at this time, it is the likelihood of getting a distorted result. If the study is repeated after recovery, the reaction will indicate the correct group [1].
Diseases affecting blood composition
Some diseases are accompanied by increased production of red blood cells. In the presence of too many red blood cells, the antibodies reach a concentration insufficient for the chemical reaction that defines the group. As a result, the studies also show the wrong result.
A change also occurs in patients with myeloid leukemia, an oncological disease, during which the number of degenerated white blood cells in the plasma rapidly increases, and the concentration of antigens decreases [2].
Effect of bacteria
Bacteria can also affect your blood type. While studying the intestinal microbiota, scientists discovered a bacterium that is capable of changing groups A and B to 0, cutting off the corresponding antigens [3]. But such changes are also temporary - they persist as long as the bacterium is present in the body, then the group becomes the same as before.
Pregnancy
It is during pregnancy that many women discover that they have a “change in blood type.” The reason is also the number of red blood cells. During pregnancy, red cells are produced by the bone marrow more intensively than during other periods of life. As a result, the concentration of antibodies also changes, causing distortion of test results.
Irreversible change in blood type
This becomes possible with a complete bone marrow transplant. Patients diagnosed with malignant bone marrow tumors need to have it replaced. As a result of this treatment procedure, a person receives a donor organ that produces new blood cells.
It should be noted that bone marrow donors are selected very carefully. The transplanted bone marrow must match the recipient's bone marrow as closely as possible. Therefore, doctors most often choose donors with the same blood type and Rh factor as the recipient.
Can BG change with transfusion?
Transfusion does not affect the BG in any way, however, there are certain exceptions to this rule:
- When identifying blood to a certain group, the health worker made a mistake.
- The patient suffers from a disease of the hematopoietic system (aplastic anemia), after treatment of which, his red blood cells acquire new antigenic properties that were previously suppressed by the disease.
- If the patient has been transfused with a large volume of donor blood: until the “new” red blood cells die, the patient may be diagnosed with another GC for several days.
- The patient underwent a donor bone marrow transplant, before which all his blood progenitor cells were destroyed using chemicals. As a result, the “new” bone marrow can produce cells with a different structure and change the BG. This probability is minimal, but it exists.
Idiopathic change of blood group and Rh factor
“All my life there was one group, and now suddenly it has changed for some reason” - is this possible?
In medicine, all diseases and pathological conditions, the cause of which is not fully studied and understood, are usually called “idiopathic”. Changing your blood type is no exception. Therefore, all cases when no one can name the reason for the change that occurred can be classified as an idiopathic change in blood group.
A change in blood type occurs without any clinical manifestations. Calm and quiet. Therefore, we can assume that such changes do not harm human health.
How do you get an incorrect test result?
BG is checked immediately after birth. A newborn child must undergo such an analysis. The standard group verification process is simple:
- Capillary blood is collected,
- The obtained material is transported to the laboratory,
- At the third stage, the group itself is checked using reagents,
- They issue a conclusion.
Even at these 4 stages, laboratory technicians are capable of making mistakes that could cost the life of the diagnosed patient in the future. In addition, the life of another person depends on the incorrectly indicated result if this patient becomes a donor.
Read also: What is FSH, a table with age norms for women at different periods of life, the ratio of FSH to LH
- Most often, medical staff make a mistake when test tubes with blood are involuntarily confused. It costs nothing to swap them. Not all laboratory technicians approach the blood sampling procedure correctly and responsibly.
- No one has canceled the dishonest attitude of medical staff towards the process of processing and disinfection of test tubes.
- Collected materials are transported in containers so they can be mixed. Mixing of samples occurs, again, due to an unfair attitude towards work.
At this stage, the possibility of obtaining an erroneous result remains. But a greater number of medical errors occur when directly studying the analysis. This happens for the following reasons:
- Incorrect addition of serum directly to the sample,
- Use of expired and low-quality reagents,
- Failure to comply with hygiene standards in the room where diagnostics are carried out,
- Inconsistency in temperature, air humidity or lighting,
- Use of outdated equipment,
- Human factor, inattention, fatigue.
There is no way to protect yourself from such “diagnosis,” especially if the analysis is carried out in a public medical institution. It is better to check the group in several laboratories. It is because of negligent medical staff that most people wonder whether the RF or GK can change.
"Pros" and "cons" of our blood
The Rh factor is a qualitative assessment of a blood characteristic parameter, depending on the presence or absence of D antigen in the human body. This indicator is innate (!).
The presence of D-antigen protein molecules is a sign of positive Rhesus (Rh+). Their absence is negative (RH-).
The second case is less common. Its owners are only about 15% of the world's population. The remaining 85% of the population has a plus sign.
There is no intermediate option. There are only two of them: either “positive” or “negative”.