What is hydrocephalus?
The term hydrocephalus is formed from two Greek words: “hydro” - water and “cephalus” - head (“dropsy of the brain”). In hydrocephalus, there is a significant buildup of cerebrospinal fluid (CSF) inside cavities of the brain called ventricles. An increase in the volume of cerebrospinal fluid (CSF) occurs when the balance between the production of cerebrospinal fluid and its absorption and further removal from the body is disturbed. This may be the result of a deficiency in the circulatory system or excessive production of cerebrospinal fluid. Hydrocephalus can be congenital or acquired. The concept of congenital hydrocephalus means that it appears from the moment of birth. The disease can be provoked by various factors: traumatic brain injury, brain tumor, necrosis, meningitis, etc. The frequency of this disease is high throughout the world. According to the literature, hydrocephalus affects 5-15 children out of every thousand newborns. Treatment consists of diverting CSF outside the cerebrospinal fluid system into body cavities where it can be absorbed (absorbed). An effective operation allows a child to live and develop normally, study in a regular school, and an adult to return to a full, active life. However, patients and their loved ones must be able to recognize the signs and symptoms of postoperative complications so that medical care can be provided in a timely manner.
Causes of hydrocephalus
Hydrocephalus develops due to the accumulation of cerebrospinal fluid in the cerebrospinal fluid system of the brain in the event of the production of an excess amount of cerebrospinal fluid, impaired absorption or disturbance of the circulation of cerebrospinal fluid. In case of exposure to damaging factors on the fetal brain during intrauterine development, congenital hydrocephalus occurs. Acquired hydrocephalus develops under the influence of various pathological mechanisms after the birth of a child.
The following causes of congenital hydrocephalus are known:
- intrauterine infections (hydrocephalus, toxoplasmosis, cytomegaly, syphilis);
- birth injury;
- defects in the development of the cerebrospinal fluid system (atresia of the foramina of Magendie and Luschka, stenosis of the Sylvian aqueduct, structural defects of the subarachnoid space, Dandy-Walker syndrome);
- developmental anomalies of the skull and spine (congenital basilar impression, Chiari malformation).
Acquired hydrocephalus occurs as a result of inflammatory processes of the brain and its membranes, traumatic brain injuries, acute and chronic vascular disorders. Hydrocephalus in adults often develops against the background of a colloid cyst of the third ventricle and intracerebral tumors (germinomas, astrocytomas, ganglioneuromas) growing into the ventricles of the brain or compressing the cerebrospinal fluid tract, disrupting the normal circulation of cerebrospinal fluid and its outflow from the cranial cavity.
Make an appointment
Anatomy and physiology
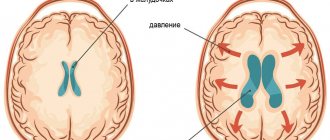
In order to better know and understand the disease, we will give you some information about the anatomy of the skull, the structure of the brain, as well as the process of formation and absorption of cerebrospinal fluid (Fig. 1). The brain occupies most of the cranial cavity. It is penetrated by a large number of blood vessels and is surrounded by cerebrospinal fluid as a buffer. The fluid is located in 4 cavities (ventricles) located inside the brain. The ventricles have delicate structures known as villous plexuses (choroid plexuses). These structures produce a significant amount of CSF - about 500 ml per day. The fluid circulates continuously and contains a large number of substances essential for nutrition and ensuring the normal functioning of the nervous system.
CSF also provides a protective cushion for the brain. CSF circulates in the ventricular system and is removed through 3 holes in the 4th ventricle and then enters the subarachnoid space surrounding the brain and spinal cord.
CSF constantly circulates in the brain and spinal cord, constantly being in the process of a) formation, b) circulation and c) absorption. In a healthy body these processes are balanced. Hydrocephalus develops if CSF is not cleared from the ventricular system through the cerebrospinal fluid tract. Less commonly, hydrocephalus is caused by excess production of CSF, such as with villous plexus papilloma.
Hydrocephalus in children: just the facts
Hydrocephalus is a disease that occurs due to excessive production and excessive accumulation of cerebrospinal fluid in the intrathecal spaces and/or ventricles of the brain (in the subarachnoid or subdural space), leading to thinning (atrophy) of the medulla and divergence of the skull bones [1–4].
ICD-10 provides the following codes for various types of hydrocephalus: G91 (G91.0 - communicating hydrocephalus, G91.1 - obstructive hydrocephalus, G91.2 - normal pressure hydrocephalus, G91.3 - post-traumatic hydrocephalus unspecified, G91.8 - other types hydrocephalus, G91.9 - hydrocephalus unspecified).
Classification of hydrocephalus
There are several options for classifying hydrocephalus. First of all, a distinction is made between congenital and acquired hydrocephalus.
Congenital hydrocephalus is present at the time of birth of the child and is the result of inflammatory diseases of the central nervous system (CNS), malformations of the brain, as well as intracranial (birth) trauma, hemorrhages in the brain.
Acquired hydrocephalus develops after birth due to etiologically and pathogenetically diverse pathologies (neuroinfections, tumor processes, vascular diseases, traumatic brain injuries, etc.).
The disease can be active or passive. In the first case, there is an increase in intracranial pressure in the presence of dilatation of the ventricles and subarachnoid spaces. With passive hydrocephalus, it is assumed that the described changes are observed in the absence of intracranial hypertension.
There are open and closed forms of hydrocephalus. Open (communicating) hydrocephalus is diagnosed in the absence of disturbances in the connection of the ventricular system of the brain with the subarachnoid space, and closed (occlusive or non-communicating) - when this communication is disrupted.
External and internal forms of hydrocephalus are determined by the localization of the accumulation of cerebrospinal fluid (CSF); External hydrocephalus is an accumulation of CSF in the intrathecal spaces of the brain, internal hydrocephalus is an accumulation of CSF in the ventricles of the brain.
Pathogenetic classification of hydrocephalus: 1) hypersecretory forms (excessive formation of CSF); 2) aresorptive forms (impaired CSF absorption processes); 3) occlusive forms (the presence of an obstacle to the movement of CSF from the source of its formation to the areas of its resorption).
Depending on the existing level of occlusion of the cerebrospinal fluid pathways, five variants of hydrocephalus are considered: 1) occlusion of one or both foramina of Monroe; 2) blockade of the cavity of the third ventricle; 3) stenosis or occlusion of the Sylvian aqueduct; 4) occlusion or non-opening of the openings of the fourth ventricle; 5) violation of the patency of the subarachnoid spaces.
Depending on the achieved level of control over intracranial hypertension, it is customary to distinguish between compensated, subcompensated or decompensated hydrocephalus.
A separate variant of the disease is normal pressure hydrocephalus (“symptomatic”). With it, an increase in intracranial pressure is initially observed (a consequence of excessive accumulation of CSF in the ventricles of the brain) - with or without ventriculomegaly, which gradually decreases, but remains moderately elevated (150–200 mmH2O). There are two types of normal pressure hydrocephalus - idiopathic (cause unknown) and secondary (consequence of subarachnoid hemorrhage, trauma, tumor and/or infection of the central nervous system, complication of neurosurgical intervention, etc.) [1–4].
S. Oi (2010) proposed a “multi-category classification of hydrocephalus”, reflecting modern ideas about this disease (Table) [5, 6].
Etiology and pathogenesis of hydrocephalus
The most important etiological factor of hydrocephalus is intra- and perinatal pathology of the central nervous system. Pregnancy pathology and oxygen starvation of cerebral tissue are considered as etiological causes of congenital hydrocephalus; intrapartum factors leading to hypoxic-ischemic and/or traumatic brain damage; gestational immaturity of brain structures most susceptible to the described damage.
The development of hydrocephalus is caused by inflammatory diseases of the brain and its membranes, as well as intrauterine and neuroinfections, congenital malformations of the central nervous system, vascular pathology, tumors of the brain and spinal cord, traumatic injuries (including intracranial birth injuries), genetic factors, etc.
Cases of hydrocephalus associated with cerebral dysgenesis, brucellosis, mumps and other infections, diffuse villous hyperplasia of the choroid plexus, vascular anomalies, intracranial hemorrhages, etc. have been described.
Post-traumatic hydrocephalus (progressive excess accumulation of CSF in the cerebrospinal fluid spaces and brain matter due to traumatic brain injury) is caused by impaired circulation and resorption of CSF [1–4, 7].
According to C. Schrander-Stumple and JP Fryns (1998), hereditary X-linked (congenital) hydrocephalus occurs in 4% of all registered cases of the disease (according to other data in 5–15% of observations), up to 40% of cases of hydrocephalus are etiogenetically caused [8 ]. Hydrocephalus occurs in Dandy–Walker syndrome, Arnold–Chiari syndrome, etc. At least 43 mutations/loci associated with hereditary forms of hydrocephalus (in humans and laboratory animals) have been described; Under experimental conditions, 9 genes associated with this cerebral pathology were found, while in humans there is only one [1–4].
The progression of hydrocephalus is accompanied by structural and morphological changes in the brain of varying severity: 1) thinning of the cortex and white matter (up to its complete elimination); 2) atrophy of the choroid plexus; 3) atrophy/subatrophy of the basal ganglia, brainstem, cerebellum; 4) severe disorders of capillary blood flow; 5) thickening and/or fusion of the meninges; 6) excessive growth (hypertrophy) of glial tissue. In severe cases, the formation of hydroanencephaly is possible, when there is only ependyma and a thin layer of the pia mater.
The most intensively functioning and highly vascularized periventricular region suffers the most from hypoxia. The consequence of atrophy of the periventricular white matter of the brain is passive expansion of the ventricular system with the formation of ventriculomegaly.
With post-traumatic hydrocephalus, pathological processes in the brain are morphologically characterized by dilation of the ventricular system, periventricular edema and obliteration of the subarachnoid fissures. Obliteration of the CSF flow paths is determined by the following pathogenetic factors: subarachnoid hemorrhage, intracranial hematomas, focal and/or diffuse brain damage, cicatricial adhesions and atrophic processes (including after extensive craniotomy and resection trepanations), meningoencephalitis and ventriculitis. The time frame for the development of post-traumatic hydrocephalus (normotensive, hypertensive or occlusive) usually varies from 1 month to 1 year [1–4, 7].
Clinical syndromology of hydrocephalus
The main symptoms of hydrocephalus (congenital and acquired) are determined by two groups of factors: 1) the causes of the disease; 2) directly hydrocephalic syndrome.
The first group mainly includes focal manifestations (usually in the form of spastic paresis of the ascending type in the lower and/or upper extremities). The severity of group 2 symptoms depends on the form, stage and degree of progression of hydrocephalus. In the congenital form of the disease, signs of hydrocephalus may be present both at birth and appear later - by the age of 3–6 months.
More often, the first sign of the disease is a disproportionately rapid increase in head circumference. To assess it in children, special tables (centile) are used.
In children of the first year of life, there may be a predominance of the “cerebral” parts of the skull over the “facial” (as a result - a forced position with the head thrown back), increased venous pattern and congestion of the saphenous veins of the head, tension of the greater and other fontanelles, divergence of the skull bones, Graefe’s symptom . These symptoms are accompanied by a lag in psychomotor development (of varying severity), and less often in physical development. Optic nipple atrophy is a severe complication of untreated or treatment-resistant progressive hydrocephalus.
Cephalgic syndrome is more typical of acquired hydrocephalus in children over 1 year of age (when the fontanelles and cranial sutures are already closed).
Clinical manifestations of post-traumatic hydrocephalus are characterized by neurological and mental disorders caused by primary brain injury. In part, they are a reflection not so much of hydrocephalus itself, but rather a consequence of a traumatic brain injury (TBI) or premorbid pathology.
A. P. Konovalov et al. (1999) distinguish three variants of post-traumatic hydrocephalus: 1) against the background of resolved or mild residual symptoms of severe TBI, with dominance in the clinic of any specific symptom complex; 2) against the background of slowly resolving severe symptoms of severe TBI with the addition of intellectual-mnestic and ataxic syndromes; 3) against the background of a vegetative state (which prevents exit from it). Hypertensive and occlusive post-traumatic hydrocephalus (excluding normotensive hydrocephalus) is characterized by headache, vomiting, and dizziness. All patients exhibit psychopathological symptoms (intellectual-mnestic disorders, euphoria or lethargy, aspontaneity, akinetic mutism, etc.); as well as gait disturbances and ataxia (with a characteristic “sticking of the feet to the floor”), dysfunction of the pelvic organs.
With normal pressure hydrocephalus, there are usually no classic symptoms characteristic of congenital or acquired hydrocephalus, but since ventriculomegaly has a negative effect on adjacent areas of cortical tissue, the disease has its own characteristics (classic triad: gait disturbances, urinary incontinence, decreased intelligence of varying degrees of severity) [ 1–4].
Diagnostics and examination methods
Establishing a diagnosis of hydrocephalus (in addition to physical data) is based on neuroimaging data (neurosonography - with an open fontanel, computed tomography and magnetic resonance imaging of the brain - CT and MRI), which are considered in conjunction with the symptoms of the disease described above. These neuroimaging methods have replaced the previously used skull radiography. It is resorted to only in rare cases; Survey radiography of the skull allows one to indirectly judge secondary changes in the bones of the skull (in the absence of CT and MRI).
It is especially important to monitor the adequate functioning of shunts installed during neurosurgical intervention. At the slightest suspicion of shunt failure, the patient should be referred to a neurosurgeon.
Isotope cisternography with the introduction of a radioactive isotope (during a lumbar puncture) and subsequent observation of the removal of CSF from the brain makes it possible to establish the diagnosis of normal pressure hydrocephalus.
Diaphanoscopy (transillumination of the skull) has now been practically abandoned. Lumbar puncture is a traditional research method that allows you to assess blood pressure and analyze the CSF. An increase in echo pulsation up to 70–80% during an ultrasound examination of the brain is not a diagnostic sign of hydrocephalus.
The study of auditory evoked potentials often reveals their disturbances, which indicates a special sensitivity of the brain stem to intracranial hypertension.
An ophthalmological examination of the fundus allows one to identify changes characteristic of hydrocephalus (congestion in the fundus, atrophic processes, signs of inflammation, as well as hemorrhage, changes in the tone and caliber of blood vessels, etc.), which makes it possible to assess the course of the pathological process.
If a congenital infection (intrauterine infection) is suspected, serological and virological studies are justified.
Abroad, a method of non-invasive monitoring of intracranial pressure through the large fontanel in children of the first year of life, based on the principle of applanation, is used. The measurement is made using a special device (fontanometer), and the study itself is called “phonogram” or “fontanometry” [1–4, 7].
Differential diagnosis
Hydrocephalus is differentiated from the following main pathological conditions: subdural intracranial hemorrhage, megalencephaly (primary), hydroanencephaly, meningitis, brain tumors, familial (constitutional) macrocephaly, vitamin D-deficient rickets, rickets of premature infants, etc.
Less common are other types of pathology from which it is necessary to differentiate hydrocephalus: achondroplasia, Soto syndrome (cerebral gigantism), numerous so-called “neurocutaneous” syndromes, a group of leukodystrophies (Alexander’s disease, Canavan’s disease, globoid and methochromatic forms of leukodystrophies), gangliosidosis, mucopolysaccharidosis (Tay’s disease –Sachs and Sandhoff), urine disease with the smell of maple syrup, etc. [1–4, 7].
Treatment
Therapeutic measures for progressive hydrocephalus are divided into surgical and therapeutic (drug and non-drug).
If there are signs of an ongoing inflammatory process in the central nervous system, children are prescribed appropriate therapy (antibacterial agents, specific drugs, as well as glucocorticosteroids and human intravenous immunoglobulins - according to indications).
Progressive forms of hydrocephalus (occlusive), as a more serious variant of the pathology, require timely neurosurgical intervention (shunt surgery). The purpose of surgery is to create an adequate outflow of CSF using special shunts (drainage systems made of synthetic materials). There are shunts that divert CSF from the ventricles of the brain to various loci of the body (ventriculoperitoneal, lumboperitoneal, ventriculoatrial). Thus, some shunts transport excess accumulation of cerebrospinal fluid into the peritoneal cavity, others - into the right ventricle of the heart. Ventriculoperitoneal shunting is the main method of neurosurgical treatment of hydrocephalus in the Russian Federation and abroad.
There is a method of surgical treatment called “endoscopic third ventriculostomy” (perforation of the lower part of the third ventricle of the brain to eliminate the blockage of CSF flow and increase its outflow); another name for the method is “endoscopic ventriculocisternostomy of the bottom of the third ventricle.” The purpose of the described operation is to create pathways for the outflow of CSF from the third ventricle into the cisterns of the brain, through which the resorption of cerebrospinal fluid occurs.
Other types of endoscopic treatment of hydrocephalus in various clinical situations are aqueductoplasty, ventriculocystocysternostomy, septostomy, endoscopic removal of an intraventricular tumor, as well as endoscopic installation of a shunt system.
Among the neurosurgical procedures in infants, ventricular puncture (removal of CSF from the ventricles of the brain through the fontanelle) can be used. This external drainage procedure is used extremely rarely, as it can be accompanied by a large number of complications (infection, etc.).
There are isolated reports of the use of intradural spinal endoscopy in the treatment of hydrocephalus and associated conditions in children.
In the acute occurrence of intracranial hypertension, drugs with a diuretic effect are used. These include: furosemide (intramuscular) - sometimes in combination with a solution of magnesium sulfate, glycerol (per os), mannitol (intravenous drip).
If long-term treatment of hydrocephalus is necessary, acetazolamide (Diacarb) is first prescribed, a diuretic from the group of carbonic anhydrase inhibitors (an enzyme that catalyzes the reversible reaction of carbon dioxide hydration and subsequent dissociation of carbonic acid). The action of acetazolamide is associated with the suppression of carbonic anhydrase in the ventricular plexuses of the brain and with a decrease in CSF production (hypolyquor effect). The side effects of acetazolamide (acidosis and shortness of breath) are systematically corrected by the administration of sodium bicarbonate (0.5 g 3 times a day).
Patients with hydrocephalus under the age of 3 years need to be prescribed vitamin D and calcium supplements. In addition to calcium, supplementation of potassium and magnesium preparations (Asparkam, Panangin) is absolutely necessary during acetazolamide therapy.
Symptomatic treatment for hydrocephalus is determined by individual indications and usually includes: massage, physical therapy, various types of physiotherapy, biofeedback method, as well as stimulating therapy (nootropic, metabolic, vascular drugs, etc.), etc. Anticonvulsants for children with hydrocephalus prescribed if there are appropriate indications (symptomatic epilepsy, etc.).
Neurodietological measures should be aimed at maintaining nutritional status, adequate fluid intake, supplementation of vitamins and minerals, and, if necessary, nutritional support (clinical nutrition: enteral and/or parenteral) [2–4].
Prevention
Since in a significant number of cases hydrocephalus can be diagnosed during fetal development, sonographic examination of the fetus is recommended (starting from the 17th week of gestation). In some cases, MRI examination is indicated, although P. Peruzzi et al. (2010) indicate that it does not have pronounced diagnostic advantages compared to ultrasound methods [9].
In order to prevent hydrocephalus in children, timely detection and treatment of intrauterine infections in their mothers is necessary. It is necessary to fully implement the prevention of childhood injuries and neuroinfections. To prevent myelomeningocele, preventive administration of folic acid supplements is indicated [1–4, 7].
Forecast
Hydrocephalus is a cerebral pathology associated with significant neurological deficits, potential disability and decreased quality of life. There is a risk of irreversible changes in the nervous system and a decrease in intelligence (even mental retardation).
With congenital and acquired hydrocephalus, the prognosis is determined by the early onset and adequacy of treatment (pharmacological or neurosurgical).
A serious complication of hydrocephalus can be epilepsy, induced both by hydrocephalus itself (structural and morphological changes in brain structures) and by the installation of a drainage shunt [1–4, 7].
According to M. Mataro et al. (2001), the average IQ values in patients with hydrocephalus are reduced in a number of verbal and nonverbal functions. Among patients who received adequate therapy, normal levels of intellectual function are observed in 40–65% of cases [10].
Literature
- Kliegman RM, Stanton BF, St Geme III JW et al., eds. Nelson textbook of pediatrics. 20 th ed. Philadelphia. Elsevier. 2016. 3474.
- Shamansurov Sh. Sh., Studenikin V. M. Congenital and acquired hydrocephalus. Ch. 11. In the book: Neurology of early childhood. Tashkent: O'Qituvchi, 2010. 156–164.
- Studenikin V. M., Shamansurov Sh. Sh. Congenital hydrocephalus. Ch. 9. In the book: Neonatal neurology. M.: Medforum, 2014. 120–135.
- Studenikin V.M., Shelkovsky V.I., Kuzenkova L.M. Hydrocephalus and hydrocephalic syndrome in children // Doctor.ru. 2006; 5:2–5.
- Oi S. A proposal on “Multi-categorical Hydrocephalus Classification”: McHc. Critical review in 72,576 patterns of hydrocephalus // J. Hydrocephalus. 2010; 2 (2): 1–21.
- Oi S. Hydrocephalus research update: controversies in definition and classification of hydrocephalus // Neurol. Med. Chir. (Tokyo). 2010; 50:859–869.
- Kandasamy J., Jenkinson MD, Mallucci CL Contemporary management and recent advances in pediatric hydrocephalus // BMJ. 2011; 343:d4191.
- Schrander-Stumple C., Fryns JP Congenital hydrocephalus. Nosology and guidelines for clinical approach and genetic counseling // Eur. J. Pediatr. 1998; 157(5):355–362.
- Peruzzi P., Corbitt RJ, Raffel C. Magnetic resonance imaging versus ultrasonography for the in utero evaluation of central nervous system anomalies // J. Neurosurg. Pediatr. 2010; 6 (4): 340–345.
- Mataro M., Junque C., Poca MA et al. Neuropsychological findings in congenital and acquired childhood hydrocephalus // Neuropsychol. Rev. 2001; 11 (4): 169–178.
V. M. Studenikin, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Economics
LLC NPSMC "Dream Clinic", Moscow
Contact Information
Hydrocephalus in children: just the facts / V. M. Studenikin
For citation: Attending physician No. 4/2018; Issue page numbers: 66-69
Tags: cephalalgia, brain, cerebrospinal fluid, intracranial hypertension
Diagnostics
In newborn children, the bones of the skull have not yet fused and hydrocephalus is determined visually. The head enlarges, the bones of the skull diverge, the fontanelle is tense and bulging; the skin is thin and shiny; The veins in the hairline area look full and swollen. Also symptoms are: vomiting, apathy, excitability, downward displacement of the eyes (“setting sun symptom”), etc. However, when the cranial sutures are not fused, the signs and symptoms of increased intracranial pressure seem subtle.
In older children and adults, the bones of the skull are fused and, when the ventricles expand, compression of the brain tissue occurs. Symptoms of increased intracranial pressure appear: headaches, nausea, vomiting, blurred vision, lack of coordination, psychopathological personality changes, lack of concentration and lethargy. These symptoms require additional instrumental diagnosis.
Symptoms of hydrocephalus in an adult
The accumulation of an excess amount of cerebrospinal fluid in a limited space of the cranium leads to an increase in intracranial pressure, which causes the most typical signs of hydrocephalus: intense headache that cannot be relieved by analgesics, nausea and vomiting, a feeling of pressure on the eyeballs.
These symptoms of hydrocephalus in an adult patient can occur acutely or increase gradually, having a transient nature at the onset of the disease. Replacement hydrocephalus often occurs without signs of increased intracranial pressure. Neurologists at the Yusupov Hospital detect it only after additional examination of the patient. Hydrocephalus of the brain in an adult in the photo has characteristic signs: an increase in the volume of the head and frontal bone.
In most cases, hydrocephalus in adults is accompanied by neurological symptoms. It is caused both by compression of brain structures by expanded cerebrospinal fluid spaces and by the underlying disease, which is the cause of the development of hydrocephalus. With hydrocephalus, vestibular disorders are observed: gait instability, dizziness, noise in the ears and head, nystagmus. Visual function is impaired: there is a significant decrease in visual acuity and loss of certain areas of the visual field. During ophthalmoscopy, ophthalmologists identify congested optic discs. With prolonged hydrocephalus, atrophy of the optic nerves develops.
Hydrocephalus in adults can occur with disturbances in the motor and sensory spheres:
- paresis and paralysis;
- decrease or complete loss of all types of sensitivity;
- increased tendon reflexes and muscle tone;
- formation of spastic contractures of the limbs.
Occlusive hydrocephalus, caused by impaired circulation of cerebrospinal fluid in the posterior cranial fossa, is characterized by symptoms of cerebellar ataxia: changes in handwriting, large-scale disproportionate movements, impaired gait and coordination.
Patients suffering from hydrocephalus develop mental disorders over time, manifested by disorders of the emotional-volitional sphere: neurasthenia, emotional instability, causeless euphoria with a rapid transition to a state of apathy. With a sharp increase in liquor pressure, patients begin to behave aggressively.
Types of diagnostic tests
- Ultrasound is a simple, inexpensive test that helps evaluate the extent to which the ventricles of the brain are dilated. Currently, it is the simplest and safest method for diagnosing hydrocephalus.
- Computed tomography (CT) - This is a technique of drawing with a thin beam the contours of the skull, brain, ventricles and subarachnoid space. It is carried out to determine the size and shape of the ventricles and identify abnormalities such as tumors, cysts or other pathologies.
- Magnetic resonance (nuclear magnetic resonance NMR) is a non-surgical diagnostic method that uses radio signals and a magnet. MRI data determines the shape and severity of hydrocephalus. These studies are indispensable for clarifying the causes of dropsy.
- Cisternography (radiography of the cisterns at the base of the skull) is a test that requires the injection of a radioactive substance into the CSF. It is used to clarify the type of hydrocephalus: communicating or obstructive, as well as to determine the direction of CSF flow.
- Pneumoencephalography is now used much less frequently than in the past. In some cases, it is necessary to pump air with a needle into the spinal cord.
- Angiography (X-ray of blood vessels) is a special technique for injecting a contrast agent into the arteries that cross the brain. After some time, anomalies are detected at the level of blood vessels and the presence or absence of pathological disorders.
- A neuropsychological examination consists of a series of questions and answers to identify the presence of abnormalities in the functioning of the brain.
The main types of hydrocephalus
At the initial consultation, the neurosurgeon will listen to the patient’s complaints, but will be able to make an accurate diagnosis only as a result of a comprehensive diagnosis. Special studies make it possible to determine what stage of the disease we are talking about - advanced or mild hydrocephalus.
There are quite a large number of varieties of dropsy:
- by origin, acquired and congenital diseases are distinguished;
- according to the characteristics of the course, hydrocephalus can be closed (occlusive), open (non-occlusive) and mixed;
- by location - internal and external hydrocephalus;
- according to clinical signs - acute, subacute, chronic degrees of hydrocephalus.
The dynamics of pathology development is also important. The most dangerous is considered progressive hydrocephalus, in which the number of symptoms constantly increases. The mild type is considered a regressive disease. With stable hydrocephalus, significant changes in the human body, as a rule, do not occur.
Treatment
Currently, occlusive (obstructive) hydrocephalus is treated surgically. Surgical intervention consists of draining excess cerebrospinal fluid outside the cerebrospinal fluid system: into the abdominal (abdominal) cavity or into the atrium. Sometimes CSF may be drained into the pleural cavity. In these cavities, cerebrospinal fluid is absorbed and excreted along with waste products of the body.
To drain the CSF, the surgeon implants a drainage system (shunt). The system material is silicone and polypropylene. Both of these materials are well tolerated by the body. All elements of the system are implanted under the skin; there are no external areas.
Diagnosis and treatment methods for dropsy
Diagnosis of hydrocephalus is carried out in several ways. For example, using multislice computed tomography. As a result, the location of the pathology and its nature are determined - closed or open. The second common research method is MRI (magnetic resonance imaging), which provides accurate data on the condition of the brain vessels, the presence of structural changes and inflammatory processes.
In the early stages of identifying hydrocephalus, conservative treatment is prescribed - for example, medication. If the results are unfavorable, surgery is indicated:
- shunting for hydrocephalus involves draining excess fluid through a tube;
- external ventricular drainage - organization of a special drainage that is inserted into the cavity with cerebrospinal fluid;
- surgical removal of a septum, tumor, or blood clot that obstructs the movement of fluid.
Contraindications to surgery to eliminate symmetrical or asymmetrical hydrocephalus are severe cardiac pathologies, inflammatory processes in the nervous tissue, and serious problems with the blood vessels or respiratory system.
Neurosurgeons of the city clinical hospital named after. A.K. Eramishantsev will help cope with problems such as replacement, normotensive, triventricular, vicarious hydrocephalus. Sign up for a consultation to get more accurate answers to your questions. With timely intervention, the rehabilitation period after surgery occurs with minimal discomfort, and within a few days after surgery, adult patients can return to work, and children can return to school and a full-fledged active lifestyle.
Shunt System Components
The system consists of two catheters and one one-way valve. The ventricular catheter is located in the ventricle of the brain, and the peripheral (peritoneal or cardiac) catheter is placed in the abdominal cavity or in the right atrium, respectively. Both catheters are connected to a valve that regulates the unidirectional flow of cerebrospinal fluid. The valves are designed to operate in different pressure ranges (high, medium, low and very low). The neurosurgeon, having determined the patient’s intracranial pressure, selects the appropriate valve, depending on the severity of the disease, the patient’s age and clinical nuances.
Almost all valve models have a reservoir that your doctor can use to “bleed” the system to determine if it is working properly. From the reservoir, by inserting a thin needle through the skin, you can take samples of cerebrospinal fluid for laboratory tests or administer medications. Patients and their loved ones are not recommended to test the drainage system by “bleeding” the reservoir. This action can be dangerous unless your doctor has given you specific instructions about it. In patients suffering from non-communicating (obstructive) hydrocephalus, cerebrospinal fluid should be drained from the cerebral ventricle using a ventricular catheter. In patients with communicating hydrocephalus, a CSF drainage system is implanted from the lumbar space of the spine into the abdominal cavity - the lumboperitoneal system.
Types of hydrocephalus in adults
There are open (communicating), closed (occlusive) and replacement hydrocephalus. Open hydrocephalus of the brain in adults involves free communication of spaces through which cerebrospinal fluid circulates. It develops when there is an imbalance in production and reabsorption of cerebrospinal fluid. There are hyperproductive, aresorptive and mixed forms of hydrocephalus.
Replacement hydrocephalus can be a consequence of physiological aging of the body or develop in pathological conditions of the central nervous system, accompanied by atrophic changes (Alzheimer's disease, Creutzfeldt-Jakob disease). This form of the disease does not refer to true hydrocephalus, caused by impaired cerebrospinal fluid dynamics, but occurs as a result of the filling of “free” spaces inside the skull with cerebrospinal fluid.
In accordance with the location of the expanded cerebrospinal fluid spaces in relation to the brain tissue, the following types of hydrocephalus in adults are distinguished: internal (intraventricular), external (subarachnoid) and mixed. Depending on the level of intracranial hydrocephalus, hypertensive and normotensive hydrocephalus are distinguished. In functional and clinical aspects, progressive (increasing), stabilized (not changing over time) and regressive (decreasing) hydrocephalus are distinguished. Progressive hydrocephalus can be decompensated or subcompensated.
In acute hydrocephalus, no more than three days pass from the moment of the first symptoms of the disease to severe decompensation. Subacute progressive hydrocephalus develops within one month from the onset of the disease, and chronic hydrocephalus develops within a period of 3 weeks to 6 months.
Surgery and hospitalization
Implantation of the shunt system is carried out by a neurosurgeon under sterile operating room conditions. In preparation for surgery, the hair is shaved to achieve maximum cleanliness. The operation is performed under general anesthesia, usually not for a very long time. The neurosurgeon drills a small hole in the skull bone, then makes a small incision in the dura mater that protects the brain and inserts a ventricular catheter into the lateral ventricle. To implant the rest of the bypass system, another incision is made and a tunnel is created subcutaneously to implant a peritoneal or cardiac catheter. The end of the catheter is carefully inserted either into the abdominal cavity or into the jugular vein leading to the ventricle of the heart. Catheters are connected to the valve using connectors on the valve itself. All parts of the shunt are thus connected into a single drainage system. At the end of the operation, small sterile dressings are applied to each incision.
Immediately after the operation, the patient is taken to the postoperative department. The patient is here from 1 hour to 1 day under close observation, then he is transferred to the ward. Most patients are discharged 7-10 days after clinical rehabilitation.
Discussion
The concept of CHIC is inextricably linked with such pathological conditions as CDV and slit ventricle syndrome (SVS). Understanding the nature of these disorders is key in choosing adequate treatment for this group of patients.
It is necessary to distinguish between simply anatomical reduction in the size of the ventricles, which does not require treatment, with the thyroid gland itself, which has characteristic clinical manifestations. On neuroimaging, narrow or slit-like ventricles are found in 20-53% of children with shunts, while clinically thyroid gland is observed in 1-37% of cases [4, 8-15]. The syndrome develops predominantly in children operated on during the 1st year of life [16]. The average age of manifestation of thyroid gland is 6-7 years [9, 13], although an earlier development of this condition cannot be ruled out [6]. Explaining the causes of the pathology causes a lot of disagreement, and the choice of tactics for thyroid gland remains a subject of debate to this day [1, 17—22]. However, it is quite obvious that all attempts to elucidate the mechanism of development of PTS against the background of CHIC inevitably lead us to the problem of CCD.
CCD refers to a condition where the volume of the growing brain exceeds the available intracranial space. In this case, normal physiological fluctuations in intracranial contents (the volume of intracranial blood and cerebrospinal fluid) lead to an increase in ICP with characteristic clinical manifestations. Various terms are used to describe this pathology in the literature: cephalocranial disproportion [23-26], post-shunt craniosynostosis [4], cranial hyperostosis [27], secondary craniosynostosis [28, 29], shunt-induced craniostenosis [17, 30], secondary microcrania [24] and others.
A. Sandler et al. [31] distinguishes two categories of CDCs:
1) primary CDD - caused by a primary pathological process leading to diffuse thickening of the bones of the arch or premature ossification and closure of the sutures. A striking example of such CCD is primary craniostenosis;
2) secondary CDD is an iatrogenic phenomenon that is initiated by implantation of a shunt system in early childhood.
The incidence of secondary CCD is unknown, since no similar studies have been conducted. Severe, disabling headaches occur in 42% of adolescents with shunts [32]. In a study of 3100 patients undergoing LSO, craniostenosis was detected in 1.6% of patients [1]. In our group of 59 children, 27 (46%) were diagnosed with premature suture closure, while signs of CD were noted in only 3 (5%) of them. It is possible that the approximate incidence of CCD can be indirectly estimated from the incidence of slit ventricle syndrome. It is conceivable that a significant proportion of patients with this syndrome suffer from CCD and their narrow, slit-like ventricles may be a manifestation of a crowded skull.
In CCD, the brain's ability to compensate for physiological fluctuations in intracranial volume is compromised for a number of reasons [33]. First, the discrepancy between normal brain volume and small cranial volume leads to increased extraparenchymal resistance. Secondly, the reduced volume of the ventricles and subarachnoid spaces, which normally participate in compensating for increased ICP, significantly reduces the potential for damping ICP fluctuations [34]. Thirdly, impaired venous outflow during CDD leads to increased pressure in the superior sagittal sinus, which impairs the absorption of cerebrospinal fluid [14]. In addition, venous congestion leads to changes in the turgor of brain tissue, increasing its rigidity and reducing compliance [11, 14].
Clinical manifestations
Typically, such patients are operated on for hydrocephalus at an early age (before 1 year) and, as a rule, they have a history of repeated revisions and multiple visits for chronic severe headaches, despite a functioning shunt. If drug treatment has an effect, it is most often insignificant or short-lived. The severity of the headache limits daily activities, including school or work activities [35, 36]. In contrast to the “low pressure” headaches that occur in a hyperdrainage state, in CCD, lying down does not reduce the severity of pain. Other manifestations of increased ICP may include diplopia, ataxia, dizziness, and disturbances of consciousness. Cases of acute deterioration leading to death have also been described [26].
Diagnostics
In a number of patients, upon examination, a characteristic deformation of the skull is revealed: microcephaly, scaphocephaly, plagiocephaly. X-rays reveal thickening of the bones of the arch, pronounced “finger impressions”, erosion of the internal plate from the pressure of adjacent grooves, thickening or compaction of the diploe, overlapping of bones in the suture area and their synostosis. Neuroimaging demonstrates normal or slit-like ventricles that do not always dilate even during an exacerbation. This is due not only to a decrease in brain compliance, but also to the absence of intraventricular obstruction [22]. On K.T. and MRI reveals a narrowing of the convexital subarachnoid spaces, as well as overfilling of the cranial cavity, especially in the posterior cranial fossa. In this case, both ascending and descending dislocation of the cerebellum can develop [24, 37]. An increase in ICP does not always lead to changes in the fundus [22]. With invasive ICP monitoring in such patients, A. Sandler et al. [31] found a correlation between headaches and the appearance of plateau waves of increased ICP.
Treatment
In case of radiographically confirmed secondary craniosynostosis and the presence of signs of CD (clinical manifestations of intracranial hypertension, narrowing of the subarachnoid spaces and cerebral ventricles), surgical intervention aimed at decompression of intracranial structures is indicated. Additional criteria may include thickening of the bones of the calvarium, pronounced “finger impressions,” and acquired Chiari malformation.
In 1974, F. Epstein et al. [20] published the results of subtemporal craniectomy performed on 2 children with narrow ventricles who had previously received shunt systems. Essentially, this method creates an artificial surgical fontanel, providing additional space for the brain, and also making it possible to palpate the increased pressure. Such decompression can be performed on one or both sides [22]. However, the authors themselves noted the low effectiveness of such interventions and unacceptable cosmetic consequences: due to the protrusion of the temporal flaps, the head took on the shape of a cloverleaf [22]. Another method used by F. Epstein et al. [11] in 2 children with shunts, there was skull fragmentation - “a radical expansion of the skull... by fragmentation of the skull from the coronal suture to the transverse sinus posteriorly and to the squamosal sutures laterally.”
Open reconstructive interventions aimed at increasing the volume of the skull have become widespread [1, 4, 6, 17, 38]. Particularly noteworthy is the fact that in case of secondary dislocation of the cerebellum, supratentorial reconstruction of the skull is pathophysiologically more justified than decompression of the posterior cranial fossa [24]. When performing reconstruction, it is advisable to replace the valve of the shunt system with a valve with a higher pressure or a programmable valve, or to add an anti-siphon device to the system [1].
Another effective method for correcting secondary craniosynostosis and CD is the use of distraction devices. Distraction osteogenesis can be defined as bone growth surgically induced by applying distending forces at the osteotomy site [39]. The simultaneous use of invasive ICP monitoring sensors and gradual distraction of the skull bones makes it possible to individualize the technique in relation to each patient, performing distraction to the required amount, at which ICP parameters are normalized [31].
Participation in care
Children with implanted shunts should be monitored by a neurosurgeon throughout their lives. Most patients suffering from hydrocephalus, after implantation of a shunt system, can lead a normal life, but constant monitoring by loved ones in collaboration with a neurosurgeon is necessary.
The neurosurgeon monitors each patient to prevent drainage failure. The first time after implantation or re-operation - regularly, with a gradual transition to examinations once a year.
Relatives are advised to be able to recognize early signs of complications. Quick and accurate assessment of health problems is very important. Flu symptoms may mask symptoms of a blocked shunt. Quickly identifying them will allow you to plan a repeat operation and avoid an emergency.
Patients and their loved ones should pay close attention to signs and symptoms of complications. The main causes are: blockage, infection and excessive drainage.
Blockage
The main type of complication is blockage of the system. Blockages can occur at any level of drainage. The holes in the ventricular catheter may become clogged with brain tissue or villous plexus tissue. It can also be blocked due to excessive contraction of the ventricular cavity due to too intense drainage of fluid from the ventricular cavity (constricted ventricle syndrome). Intestinal loops or necrotic tissue may adhere to the peritoneal catheter. Shunts inserted into a ventricle of the heart can become blocked by blood clots, pieces of brain matter, or tumor cells.
The shunt system may also be disconnected by disconnection of various elements of the shunt or by changes in the position of the catheter caused by the growth of the child. X-rays are necessary to check the integrity of the shunt.
Partial blockage of the system parts provokes the appearance of symptoms of increased intracranial pressure. Episodic headaches, nausea, apathy and decreased sensory functions may occur. Decreased performance at school or at work is the most common phenomenon in these conditions.
In case of complete blockage, symptoms develop more quickly (headaches, nausea, vomiting, blurred vision, loss of coordination and confusion). The patient falls into a stupor or coma. In such cases, urgent hospitalization is necessary for observation and appropriate treatment.
The surgeon performs a series of tests to locate and determine the extent of drainage blockage. Sometimes it is necessary to remove and replace part or all of the system.
Infection
Infection is the second type of complication. It poses a significant risk for any surgical procedure, most often when implanting a foreign body.
It manifests itself in the form of redness or suppuration along the edges of the suture or along the path of the drainage system under the skin. The surgeon fixes his attention on these signs. If left untreated, the wound may erode or open, and in more serious cases, the infection may cause chills and fever. Typically, the drain needs to be removed. Sometimes antibiotic therapy can be administered without removing the system.
Since the shunt is a foreign body, the patient may experience an allergic or inflammatory reaction. Inflammation at one of the drainage sites should be immediately shown to a neurosurgeon.
Excessive drainage
Excessive drainage of cerebrospinal fluid occurs when the valve is incorrectly selected according to the pressure parameter. If the valve opening pressure is too low, it can cause excessive drainage, causing the cerebral ventricle to compress and deforming the brain tissue. The patient experiences headaches that are most severe when standing.
In addition, nausea, vomiting, drowsiness and nervous system disorders, in particular double vision, appear. School-age children experience a decline in mental abilities.
More information about shunt systems for the treatment of hydrocephalus
The result of the operation largely depends on the quality of the shunt system. In recent years, in many hospitals, neurosurgeons have been using shunt systems produced by the largest American company Medtronic. The company's engineers, together with leading US neurosurgeons, have developed a range of valves of various models and sizes (including valves for newborns).
One of the latest achievements in the production of liquor drainage devices is the Delta valve. This is a unique valve, has no analogues from other manufacturers. It was created to avoid such a common complication as excessive CSF drainage. If all other valves pass as much fluid as they are designed for pressure, then the Delta valve allows as much fluid as is needed to remain in the ventricle to maintain intracranial pressure within physiological limits. When implanting the Delta valve, the patient is maintained at normal pressure, regardless of the rate of cerebrospinal fluid production and, most importantly, regardless of the patient’s body position (lying/standing).
The technological features of the materials from which the system valves are made prevent deformation and sticking during pumping; the dome of the valve reservoir is designed to withstand repeated punctures with a thin needle (the holes self-tighten). Catheters are made of high-quality latex-free silicone, so they do not stick together or form loops, which significantly reduces the risk of system blockage.
The valves are equipped with connectors for connection to catheters; their design facilitates connection and reduces the possibility of disconnection and disconnection of the system.
A radiopaque mark is applied along the length of the catheters, this allows you to see the shunt on an x-ray. The same substance is applied to the valve with a dot code indicating the pressure of the valve. There are no metal parts in the shunt system. This is very important when conducting CT and NMR studies, because metal will produce artifacts, and a magnet in NMR may shift the location of the system (if it had metal parts).
All systems are sterile and supplied in double sterile packaging. To reduce the risk of infection, Medtronic has developed a unique BioGlide hydrogel. It is applied to the inner and outer surfaces of catheters, as well as the outer surface of the valve, and does not peel off. Before implantation, the neurosurgeon can treat the system parts with antibiotics, and the hydrogel will hold them for 3 days for postoperative antibiotic therapy inside the patient’s body. This way, the risk of infection is minimized.
Treatment of hydrocephalus
Neurologists at the Yusupov Hospital take a differentiated approach to treating patients with hydrocephalus. In case of a regressed form of the disease, drug therapy is not used. To reduce cerebrospinal fluid pressure, patients are prescribed diuretics: Diacarb, mannitol, Lasix. Nootropics, venotonics and angioprotectors improve the functional activity of the brain.
For progressive hydrocephalus, neurosurgeons at partner clinics of the Yusupov Hospital perform shunt operations. If there is an obstacle to the outflow of cerebrospinal fluid, the space-occupying lesion is removed or the adhesions are cut. If a hematoma is present, it is removed surgically.
An innovative method of treating hydrocephalus is endoscopic surgery:
- endoscopic ventriculocisternostomy of the bottom of the third ventricle;
- endoscopic installation of a shunt system;
- septostomy;
- aqueductoplasty;
- ventriculocystocysternostomy;
- endoscopic removal of intraventricular brain tumor.
Endoscopic operations have a number of advantages compared to bypass interventions: they restore the physiological flow of cerebrospinal fluid, are less traumatic, and improve the patient’s quality of life.
Treatment with endoscopic methods
Endoscopic treatment of hydrocephalus, or dropsy of the brain, is a priority in neurosurgery, since this disease is common among both children and adults. Hydrocephalus of the brain occurs due to impaired absorption of cerebrospinal fluid into the venous system.
Endoscopic surgery
Endoscopic interventions for hydrocephalus of the brain are used to reduce intracranial pressure. Surgeries for dropsy are most effective in comparison with drug therapies, which help slow the progression of the disease, but do not eliminate it. Endoscopic surgery for hydrocephalus, the cost of treatment of which is determined by the severity of the disease, is divided into several types:
- Septostomy;
- Ventriculocisternostomy of the floor of the third ventricle;
- Ventriculocisternostomy;
- Installation of the shunt system endoscopically;
- Removal of intraventricular tumors endoscopically;
- Aqueductoplasty.
The most widely used is endoscopic ventriculocisternostomy of the bottom of the third ventricle. The main task of the surgeon with this technique is to create pathways for the outflow of cerebrospinal fluid from the ventricles into the cisterns of the brain, through which the cerebrospinal fluid is absorbed into the vascular walls, as in a healthy person.
Advantages of endoscopic operations
Endoscopic surgery can only be effective if it is performed by a good specialist. One wrong move by the surgeon during brain surgery can lead to irreparable, severe consequences. When shunts are installed, they are often blocked by blood clots, tumor cells, etc. During endoscopy, no foreign objects remain in the body, and accordingly, the development of such complications is excluded.
In severe cases, patients are given brain drains. Such an event is very dangerous, since the infection can easily penetrate the brain through the drainage. With endoscopic intervention this complication does not occur.
Bypass surgery
Many people who have been diagnosed with the disease wonder where to treat hydrocephalus: in a public medical institution or a modern clinic. Yusupov Hospital is equipped with the latest equipment. Doctors regularly improve their skills and master new treatment methods. The clinic staff ensures a comfortable stay for patients.
Shunt surgery for hydrocephalus in adults, the price of which varies depending on the characteristics of the disease, is performed safely and efficiently at the Yusupov Hospital. Installation of a shunt system ensures the removal of cerebrospinal fluid. The procedure lasts about 90 minutes and is performed under general anesthesia for patients of any age.
Bypass surgery is a safe intervention, but there are certain risks when using it, which the neurologist informs the patient about. For example, a reaction to anesthesia or bleeding may develop. Shunt surgery allows the patient to restore normal brain function.
Emotional support
The physical side of hydrocephalus is only part of the problem of this disease. The patient and his relatives need to take into account his emotional factors.
Although surgery should resolve your hydrocephalus to some extent, you may feel fearful, depressed, irritable, or doubtful. If the patient is a child, it should be taken into account that he has the same feelings as an adult. If your child is feeling out of shape or uncomfortable because they need to visit the doctor frequently or have repeated tests, it is best to reassure them with simple explanations. If he knows what awaits him, he will be more willing to cooperate with you. Children, like adults, as a rule, do not like unpleasant surprises. A calm atmosphere among loving loved ones is the best environment for children. It is advisable to explain the phenomenon of hydrocephalus in words that the child can understand.
It is very important to know how the child feels and be able to explain to him what he is experiencing. The needles hurt. It is natural to cry and want to get rid of them. Being admitted to hospital is a new challenge for your child. You must tell him the truth in order to gain and secure his trust. Sincerity is the best way to maintain your child's trust.
Children over ten years of age are generally able to comprehend more complex concepts. They may associate signs and symptoms with their illness. Restrictions associated with the disease are easier for them to bear. Tell your doctor about your feelings and give him the right to guide you. Some people share their feelings with close friends, others need professional help. The health professionals treating you or your child are interested in your well-being and their goal is to do what is best for you and your loved ones.
Patients and the patient's parents should communicate with their doctor quite frequently. It is important to actively participate in this communication so that your doctor can better understand your needs and the needs of your loved ones.