Blood donation (from the Latin donare - “to give”) and (or) its components is the voluntary donation of blood and (or) its components by donors, as well as activities aimed at organizing and ensuring the safety of the collection of blood and its components. Blood taken from a donor (donor blood) is used for research and educational purposes; in the production of blood components, medicines and medical devices. The clinical use of donor blood and (or) its components is associated with transfusion (transfusion) to the recipient for therapeutic purposes and the creation of reserves of donor blood and (or) its components.
Artificial blood substitutes have side effects, are toxic, expensive and are not able to completely replace all components and reproduce all the functions of blood in the body, therefore donor blood is practically irreplaceable for transfusions to victims of burns and injuries, during complex operations and during difficult childbirths. Blood is also vital for patients with hemophilia, anemia and cancer patients during chemotherapy. Every third inhabitant of the Earth needs donor blood at least once in his life.
Requirements for the donor, his rights and obligations
Citizens of the Republic of Belarus, as well as foreign citizens and stateless persons permanently residing in the Republic of Belarus, aged from eighteen to sixty years, who have full legal capacity, have undergone a medical examination, do not suffer from diseases and are not in conditions where in which donating blood and its components is contraindicated.
A prerequisite for performing the donor function is the prior written consent of the donor to take his blood and its components.
What cardiovascular pathologies do not allow donation?
In addition to hypertension, there are diseases of the cardiovascular system that prevent the possibility of being a donor.
In case of these pathologies, collection at a blood transfusion center or station is prohibited:
- atherosclerotic vascular lesions;
- heart defects;
- tendency to thrombosis;
- cardiosclerosis;
- IBS.
Along with hypertension, there are other diseases of the cardiovascular system in which donation is contraindicated
A gentle or limited sports regimen is recommended for patients. Donating blood is an above-average physical activity and often leads to an exacerbation of the underlying pathology and causes death. Before collecting the material, you need to be examined by a therapist and find out if there are any such pathologies.
Conditions for donating blood
Before the blood donation procedure, the donor must register, fill out a short questionnaire and undergo a medical examination: donate blood from a finger prick to test the hemoglobin level, and then undergo an examination by a transfusiologist. All this happens directly at the donor point and does not take much time. When donating whole blood, no later than six months after each donation (at which part of the blood is taken for analysis), the donor must come to the donor point to donate blood for a second test. In case of no-show, the collected donor blood is destroyed. Periodically, the donor needs to have a fluorography of the chest organs, an ECG with interpretation, a urine test and a clinical blood test, receive a certificate from an infectious disease specialist about the absence of contact with patients with hepatitis and other infectious diseases at the place of residence over the past 12 months, and a certificate from a therapist about previous diseases. Women must also undergo a gynecological examination.
Contraindications to donation
Depending on previous diseases, operations, procedures, a person may not be allowed to donate blood temporarily (temporary contraindication) or permanently (absolute contraindication). A temporary contraindication (temporary withdrawal from donation) implies that a certain time must pass after a procedure, surgery, or recovery before a person can donate blood. An absolute contraindication (permanent refusal to donate) implies that a person will not be allowed to donate blood, regardless of how much time has passed after his recovery.
Examples of diseases leading to permanent exclusion from donation: viral hepatitis, AIDS, carriage of HIV infection, congenital or acquired syphilis, generalized psoriasis, eczema, complete absence of hearing and speech, complete blindness, drug addiction, alcoholism, malignant neoplasms; Surgical interventions for resection or transplantation of any organs, transplantation of any tissues also lead to an absolute contraindication. For example, tattooing or ear piercing, vaccinations (for a period of ten days to one year), some infectious diseases, including acute respiratory infections (ARVI), surgical interventions, including abortions, pregnancy and lactation.
An increase in ALT activity of less than two times leads to a withdrawal from donation for three months. In this case, some donor points require the donor to provide a certificate from an infectious disease specialist confirming the absence of diseases and contacts with infectious patients, as well as negative results of the “Infection Markers” test, which is used to determine the presence of Australian antigen (surface antigen of the hepatitis B virus) and antibodies to the blood in the blood. hepatitis C virus. A referral for a test can be obtained from an infectious disease specialist at the clinic at your place of residence, where you can also donate blood for testing.
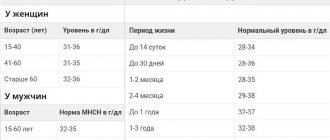
A decrease in hemoglobin content in the blood by more than ten g/l from the norm after the next blood donation leads to a six-month withdrawal from donation.
Detailed description of the study
Hypertension (hypertension) is a chronic increase in systolic blood pressure of more than 140 mm Hg. Art. or diastolic blood pressure more than 90 mm Hg. The disease occurs without external causes and primary damage to other organs, such as the kidneys, which is why it was previously called “essential” hypertension
The World Health Organization estimates that 54% of strokes and 47% of cases of coronary heart disease are a direct consequence of high blood pressure, making hypertension an important risk factor for cardiovascular morbidity and mortality.
Blood pressure in the body is regulated by many mechanisms, including: vascular resistance to blood flow, the effect of hormones on the arteries, signals from the nervous system, and the rate of fluid filtration in the kidneys. Changes in the action of these mechanisms lead to disruption of pressure regulation. The predominant cause of hypertension is thought to be increased vascular resistance, often in combination with increased arterial stiffness.
The presence of hypertension implies a genetic predisposition. Genes have been identified whose changes (mutations) increase the risk of hypertension. They are associated with changes in the regulation of arterial wall resistance and other mechanisms, but the contribution of environmental factors is also important.
It should be taken into account that external factors such as excess salt intake, obesity, smoking and alcohol abuse are important in the occurrence of hypertension along with genetic predisposition. They ultimately determine how severe the increase in blood pressure will be.
Most people with hypertension do not show any signs of increased blood pressure, even if the levels reach dangerously high levels. Some report headaches, shortness of breath, or nosebleeds, but these symptoms are not specific to hypertension and may be related to underlying conditions.
In view of this, people whose close relatives suffer from hypertension and have suffered a heart attack or stroke need regular monitoring of blood pressure levels. Screening for genetic predisposition to hypertension can help identify causes of high blood pressure and assess the risk of hypertension among those with close relatives with the disease.
The study aims to identify mutations in genes associated with an increased risk of hypertension, such as:
- Angiotensinogen (AGT). Polymorphism: Met235Thr (M235T; Met268Thr; M268T);
- Angiotensinogen AGT: 521 C>T(Thr174Met);
- Adducin 1 alpha ADD1: G1378T;
- Angiotensin II receptor type 1 AGTR1: A1166C;
- Angiotensin II receptor type 2 AGTR2: 1675 G>A;
- CYP11B2 - Cytochrome P450 gene, family 11 B;
- G protein polypeptide 3 GNB3: C825T;
- Endothelial nitric oxide synthase type 3 NOS3: T-786C;
- Endothelial nitric oxide synthase type 3 NOS3: Glu298Asp (E298D).
Everything you need to know about donation
Who can donate blood and its components?
Citizens of the Republic of Belarus, as well as foreign citizens and stateless persons permanently residing in the Republic of Belarus, aged 18 to 60 years, who have full legal capacity and do not suffer from diseases and conditions in which donating blood and its components are contraindicated, are allowed to perform the donor function. .
In exceptional cases established by the Ministry of Health of the Republic of Belarus, the medical advisory commission of the organization of blood transfusion may decide to allow persons over the age of sixty to perform the donor function.
What is the procedure for enrolling as a donor?
When registering to donate blood, the donor must provide:
- passport of a citizen of the Republic of Belarus with residence permit or registration for at least 6 months at the specified address. Those living in the dormitory must provide a certificate from the commandant (passportist) indicating the specific room of residence (at least 6 months);
— a medical certificate about the state of health (form 1 health/u-10), previous diseases, injuries, operations (taken at the clinic at the place of residence) is provided every six months;
— fluorography data of the chest organs is provided once a year;
— a conclusion from a gynecologist (female), provided once every 6 months;
— general urine test at the request of the medical registrar no later than 10 days before donating blood;
— military ID (for initial application);
— photograph (for initial application).
How often can you donate blood and its components?
Men can donate whole blood no more than 5 times a year.
Women – no more than 4 times a year.
The interval between blood donations is at least 60 days, after the 5th donation - not
less than 90 days.
After donating plasma, at least 14 days must pass before the donor can donate plasma again.
What medical examination do I need to undergo to become a donor?
All necessary tests are usually done directly at the blood transfusion station. Determined: blood type and Rh factor; general blood test data (hemoglobin, leukocytes, erythrocytes, ESR, etc.); as well as markers of pathogens of blood-borne (blood-borne) infections: human immunodeficiency virus, hepatitis B and C viruses; the causative agent of syphilis.
In addition to the blood test, the potential donor undergoes a medical examination at the blood transfusion station, during which the doctor measures blood pressure, temperature, pulse, and asks about his health. Before the blood donation procedure, each potential donor fills out a special “donor questionnaire” in which he answers questions about his state of health and previous diseases.
The final decision on admission to blood donation is made by a transfusiologist, who also evaluates the psychoneurological status of the donor and can reject him if he is suspected of using drugs, alcohol, or leading an antisocial lifestyle.
How is donating blood different from donating plasma?
When donating plasma, the donor's blood is taken, part of the plasma is separated, and the red blood cells are returned to the donor. Plasma can be donated at intervals of at least 2 weeks, and whole blood can be donated no more than 3-5 times a year at intervals of 60 days.
After five regular blood donations, it is better to take a break for 3-4 months.
How long do you really need to wait after a risky situation (when you can become infected with HIV or viral hepatitis) for the tests to be informative?
At least 6 months. In no case should you hide existing risky situations from the doctor at the donor point. Hidden information can be dangerous for the recipient.
Can a smoker be a donor?
Smoking is not a contraindication to donation. Experts recommend refraining from smoking one hour before donating blood and not smoking for two hours after donating.
What types of blood donation are there?
The most common method is to donate whole blood. It is taken from a vein in the arm with an average of 450+/-50 ml at a time and lasts 7-10 minutes.
You can donate not whole blood, but its components, for example, plasma - the procedure is called plasmapheresis, or platelets - thrombocytapheresis.
During these procedures, only the component necessary for clinical use is selectively extracted from the donor's blood, and all other components are returned to the bloodstream.
Plasmapheresis procedures are performed much more often. There are two ways to carry them out: manual (manual) or also called “intermittent”, when a dose of blood is taken from a donor and immediately centrifuged, separating it into red blood cells and plasma. The red blood cells are returned to the donor, and the plasma is quarantined. With automatic plasmapheresis, the process occurs continuously using a special device. The whole procedure takes 30-40 minutes.
How to prepare for donating blood?
1 - 2 days before blood donation, exclude fatty, fried, spicy foods from the diet (butter and vegetable oil, cream, milk, sour cream, cottage cheese, lard, mayonnaise, nuts, seeds, eggs).
Blood supply is carried out after a light breakfast (not on an empty stomach! ), it is advisable not to eat fatty, fried and dairy products the previous evening; sweet tea, crackers, cookies, fruits are recommended.
You must refrain from:
— drinking alcohol 48 hours before donating blood,
- as well as from the use of aspirin, analgin and medications containing aspirin and analgesics 72 hours before the procedure,
- if possible, refrain from smoking an hour before the procedure,
- You also need to get enough sleep.
Donors in a state of alcoholic intoxication or hangover will not be accepted and no supporting documents will be issued.
How long should it take after drinking alcohol before donating blood?
It is strictly forbidden to drink alcohol 2-3 days before and on the day of blood donation.
What needs to be done to restore the body after donating blood?
On the day of blood donation, heavy physical and sports activities and heavy lifting are not recommended. For two days, it is recommended to eat well and regularly, drink at least 1-2 liters of liquid per day (alcohol is not recommended). Then lead your normal lifestyle.
To restore your blood composition faster, it is recommended to drink more fluids - juices, tea. Proper nutrition is necessary: the donor’s diet should always contain protein, which determines the level of hemoglobin in the blood. Products containing protein - meat, lentils, beans and all legumes, fish, etc.
Is it possible to become addicted to donation?
There is no habituation to donation: hematopoiesis in the body of a healthy person is a complex self-regulating process that is not affected by periodic blood donations.
How is the record of blood donated by a donor and, in general, the record of donors kept?
Records of blood donated by a donor and donor records are maintained in the medical institution where blood donation is carried out. Information about the donor is simultaneously entered into an electronic database. For now, electronic databases are maintained in each region independently and are not interconnected. In the future, they will all be united into a single information network of donors in Belarus.
When registering, each donor is also given a “Donor Questionnaire”, which he or she fills out independently or with the help of a medical registrar.
Registration forms are stored for 5 years, except for the “Donor Registration Card”, which must be stored for 75 years. When a donor is deregistered, a record is made of the reason for the donor’s deregistration in the “Medical Card of an Active Donor” and in the “Donor Registration Card” and the total amount of withdrawn blood or its components for the entire period of donation is summed up.
What is the single dose for donating blood?
The volume of blood donation should not exceed 13% of the circulating blood volume, which is 7 – 7.2% of the donor’s body weight. The dose of standard blood donation is 450±50 ml.
For modern medicine, it is very important that as many people as possible weighing more than 55 kg give blood in a full dose of 450 ml, and plasma 600 ml. Doctors have to transfuse blood components in large doses to one patient, and the fewer number of donors the blood is taken from, the more safe and effective its action as a therapeutic agent.
Is it harmful to donate blood? Is the human body adapted for this?
Donating blood is not harmful. The human body is evolutionarily adapted to bloodletting: this is a universal reaction mechanism in case of injury, and in women, in general, it is part of the functioning of the body.
Who needs donor blood?
Every third person on earth needs blood donors at least once in their life. There are several categories of people who need donor blood.
There are people who need blood products for life. These are, first of all, patients with hemophilia. If there are enough clotting factors, and the patient has received adequate supportive therapy since childhood, then he is no different from an ordinary person and leads the life of an ordinary person. And without blood clotting factors, the life of such patients is simply impossible.
Patients with cancer need donated blood. Modern treatment of malignant tumors involves killing tumor cells. Along with the tumor cells, normal hematopoiesis also stops for some time. It is during this period that the patient needs maintenance therapy with components of donor blood, in particular, platelets, for which there is no replacement, and is not even theoretically expected in the near future.
Donor blood is needed for patients with surgical pathology. These are people who need joint replacements, these are cardiac surgery patients. Surgical operations involve trauma to blood vessels and tissues, and the need to restore lost blood components.
Blood transfusions are often required for women during childbirth. A certain number of women in childbirth are always at risk of blood loss, which also needs to be properly compensated in order to save the life of the mother and child.
What sensations may arise when donating blood? I want to help, but I'm terribly afraid of all these procedures.
As for sensations, everything is very individual. There may be a slight sensation of pain when inserting the needle into the vein, but only for a couple of seconds. Sometimes during blood donation, more often in men, fainting occurs. Women, due to their physiology, are better adapted to small blood losses. Moreover, fainting speaks more of psychological fear. Many donors do not observe any changes in their well-being and do not cancel the reduction in their usual activity on the day of donating blood - they go to work, etc. And for many, there is euphoria from the consciousness of a good deed done.
What is plasmapheresis?
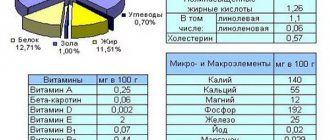
Plasmapheresis is the selective removal of plasma from the body. Plasma is the liquid part of blood. It contains a wide variety of substances: proteins (including coagulation factors), fats, carbohydrates, hormones, vitamins, salts, which are necessary for building body tissues and maintaining their vital functions, as well as organic substances that regulate metabolism. Plasma is widely used for medicinal purposes in surgery, obstetrics and gynecology, oncology and other areas of medical practice.
Donor plasmapheresis is a method of obtaining plasma from a donor with the return of one’s own blood cells (erythrocytes, platelets, leukocytes).
What should I do if I want to donate blood for a specific patient?
If you know the first and last name of the person for whom you want to donate blood, then it is enough to come to the medical institution where such a patient is located and go to the donor point, which is usually located at the hospital.
You can also contact the blood transfusion station that serves this medical institution and inform that you are going to donate blood for a specific patient, indicating his name and place of treatment. You must first coordinate blood donation with the doctors who are treating the patient for whom you want to donate blood.
What can and cannot be done after donating blood?
Immediately after donating blood, sit for 10-15 minutes. Refrain from smoking for an hour before and after blood donation, and refrain from drinking alcohol for 24 hours. Do not remove the bandage for 3-4 hours, try not to get it wet. Try not to undergo intense physical activity during the day. Try to eat plentifully and regularly for two days. Drink increased amounts of fluid for two days. Do not plan to give blood immediately before exams, competitions, a project, during a particularly intense period of work, etc.
Why is a donor registered in one region not allowed to donate in another region?
This is due to security issues. The ban on not taking blood from people arriving from other regions is caused by the hypothetical assumption that in one region the donor is listed as a person exempt from donation, and in another region there is no way to verify the opposite. With the introduction of a unified information base, which will contain a register of persons exempted from donation in all regions of the republic, this problem will be eliminated.
How does donating blood affect your health?
Donating blood on a regular basis is useful for the prevention of diseases of the cardiovascular system and, in addition, promotes self-renewal of the entire body. Scientists, in the course of examining a large number of men, found that those who regularly donate blood have heart attacks ten times less often. American researchers from the Kansas Medical Center confirmed that men who are regular donors are 30% less likely to suffer from heart attacks.
Moreover: donating blood and subsequent renewal most directly influence the improvement of a person’s emotional state. And in serious situations, for example, in an accident, the donor has a better chance of survival, since his body is more adapted to blood loss.
Will I be infected with anything?
No. Everything necessary for blood collection is disposable and is opened in front of the donor. It is possible to become infected with hepatitis and HIV infection during a manicure, in a hairdresser, in a tattoo parlor, during acupuncture, but not at a blood transfusion station.
Could I faint?
You can. But according to statistics, only every tenth donor experiences illness. Most often - men. It is psychologically more difficult for them. Fainting is rare. Basically everything gets done with dizziness. They pass quickly.
I have a tattoo...
A tattoo is not an absolute contraindication. This is reinsurance. In a tattoo parlor you can become infected with HIV and hepatitis. After getting a tattoo, you can donate blood only after 1 year. The number of tattoos does not matter. The same applies to acupuncture treatment.
What are the requirements for blood (plasma) donors?
— the donor must lead a healthy lifestyle;
- have proper, sufficient sleep and rest, do not come for donation after a night shift;
- do not hide from the doctor information about previous diseases, about casual sexual relations that can lead to infection with HIV, hepatitis, and sexually transmitted infections;
- do not drink alcohol (including beer) for three days before donating blood;
- do not come for blood donation if there are signs of an acute illness (runny nose, cough, headache, sore throat, etc.) the day before and on the day of blood donation, do not take fatty foods;
- exclude significant physical activity, psycho-emotional stress.
What guarantees and compensation are provided to donors of blood and its components?
After donating blood or its components, the donor receives monetary compensation and a “Certificate of guarantees and compensation to the donor”, according to which he is exempt from work, study, service on the day of the medical examination and donation of blood (plasma) while maintaining the average salary.
Maintaining average earnings is carried out by organizing blood transfusions in the manner determined by the Council of Ministers of the Republic of Belarus.
Full-time students upon provision of a certificate from the dean's office of the relevant educational institution.
Article 31 guarantees provided to a donor who donated blood and its components on a reimbursable basis. Article 311 guarantees provided to a donor who donated blood and its components free of charge.
Based on materials from the site https://donor-gomel.by/