Lisinopril: active ingredients
The name of the drug is identical to its active substance - lisinopril dihydrate. Separately, you can find the drug under other trade names. As a rule, its cost under other names is significantly higher.
The following can be used as auxiliary components by various manufacturers:
- corn starch or pregelatinized;
- calcium hydrogen phosphate;
- mannitol;
- magnesium stearate;
- colloidal silicon dioxide;
- microcrystalline cellulose;
- talc.
The drug is produced in the form of oblong white tablets. Its edges are rounded and there is a risk in the center. Each tablet contains 5 mg, 10 mg or 20 mg of active ingredient. The medicine is packaged in 10 tablets in a blister. The package contains 30 doses (3 blisters).
Lisinopril analogs
The original Lisinopril has an affordable price, but there are still many generics (analogs of the drug from different manufacturing countries) on the market.
Substitutes (synonyms) for Lisinopril in Russia
- Lisinopril-Ratiopharm;
- Diroton (Hungary);
- Diropress (Germany, Slovenia);
- Iruzid (Croatia);
- Ko-Diroton (Poland, Hungary);
- Lysigamma (Germany);
- Rileys-Sanovel (Türkiye);
- Scopril (Macedonia);
- Equator (Hungary, Russia).
Lisinopril is available in the form of tablets of 5, 10 and 20 mg.
There are also many medications on the market that combine Lisinopril with other groups of antihypertensive substances:
- with Amlodipine (Equator, Tenliza);
- with Hydrochlorothiazide (Co-Diroton, Lisinopril-H,HL, Lizoretik);
- with Indopamide (Diroton-Plus).
Such combinations were created to simplify the regimen and reduce the number of tablets, which increases the likelihood of systematic use of the drug.
How does Lisinopril work?
The drug acts on the renin-angiotensin system of the heart, interfering with dilatation of the left ventricle. At the same time, there is a decrease in the load on the myocardium. The substance reduces pressure in the capillaries of the lungs, as well as in peripheral vessels. When treated with Lisinopril, the tolerance of the cardiac myocardium to increased stress increases. In addition, the activity of renil in plasma increases.
After taking a single dose, the first positive effect occurs after 50-60 minutes. The manifestation of the therapeutic effect intensifies within 7 hours and persists throughout the day. Therapy lasting for several weeks achieves the maximum possible hypotensive effect.
Eating does not interfere with the absorption of the active substance, but at the same time does not contribute to it. Therefore, taking the medicine does not depend on the time of eating. Absorption of Lisinopril reaches 25%. The drug molecules bind weakly to blood proteins. Half-life occurs after 12 hours. Substances are excreted unchanged by the kidneys. Lisinopril does not form metabolites.
Lisinopril in the treatment of arterial hypertension in patients with pathology of the digestive system
The prevalence of arterial hypertension (AH) in Russia reaches 40% in men and 50% in women. In 83.3% of patients, hypertension is combined with diseases of the digestive system, including 30% with liver pathology.
To correct blood pressure (BP) in patients with hypertension, antihypertensive drugs of various pharmacological groups are used, among which the most frequently prescribed drugs are angiotensin-converting enzyme (ACE) inhibitors [7].
Over the past 30 years, ACE inhibitors have been called the “cornerstone of the treatment of cardiovascular diseases” (E. Braunwald, 1991) and the “gold standard of therapy” (J. Cohn, 1998) [10].
The results of numerous international studies have shown that these drugs are the most effective, reducing mortality from cardiovascular diseases, having organoprotective effects, and therefore are recommended as first-line antihypertensive drugs for long-term treatment of patients with hypertension.
Currently, the best known ten ACE inhibitors are captopril, enalapril, benazepril, fosinopril, lisinopril, moexipril, perindopril, quinapril, ramipril and trandolapril. Five of them (captopril, enalapril, lisinopril, ramipril, trandolapril) have been shown to reduce mortality in large studies [21, 23, 24, 28–32].
The Scandinavian study (STOP-2) compared the effectiveness of ACE inhibitors (lisinopril or enalapril 10 mg per day) with other antihypertensive drugs (beta-adrenergic blockers, hydrochlorothiazide in combination with amiloride or felodipine) in the treatment of 6614 patients with hypertension for 54 months [ 22].
This study showed that ACE inhibitors significantly reduced the risk of heart failure.
The ALLHAT study included 33,357 hypertensive patients followed for an average of 4.9 years [1, 17]. The first group of patients was prescribed chlorthalidone (up to 25 mg per day), the second - amlodipine (up to 10 mg per day), the third - lisinopril (up to 40 mg per day). During therapy with lisinopril, stroke (“end point”) occurred less frequently than when using a diuretic.
The TPOPHY study compared the effectiveness of monotherapy with hydrochlorothiazide and lisinopril in overweight hypertensive patients. Monotherapy with an ACE inhibitor ensured blood pressure control in 60%, and monotherapy with a diuretic in 43% of patients. In the group receiving lisinopril, in more than half, a dose of 10 mg/day was sufficient, and only one in four needed to be prescribed 40 mg/day. To achieve the target blood pressure level during diuretic therapy, almost every second person required the prescription of 50 mg/day of hydrochlorothiazide, which is associated with the likelihood of life-threatening arrhythmias.
In the GISSI-3 study, patients receiving lisinopril had a significantly reduced risk of death and cardiovascular disease [9].
Therapy with ACE inhibitors in patients with hypertension and diabetes mellitus significantly reduces the risk of target organ damage. In the EUCLID study in 530 patients with type 1 diabetes mellitus, lisinopril had a nephroprotective effect and reduced the risk of progression of retinopathy.
The multicenter, randomized, double-blind ATLAS trial showed that treatment with high doses (33.2 mg per day) of lisinopril was associated with a significant reduction in the risk of death or hospitalization by 12% [27].
The antihypertensive effect of ACE inhibitors is associated with:
- inhibition of the renin-aldosterone-angiotensin system in tissues and the vascular wall;
- inhibition of the conversion of inactive angiotensin I into the active vasoconstrictor angiotensin II and a decrease in aldosterone secretion;
- increased plasma renin activity;
- accumulation of bradykinin due to inhibition of kininase II;
- dilatation of renal vessels with increased natriuresis;
- increased synthesis of prostaglandins PGI2 and PGE2 [18, 20].
The release of PGI2 and PGE2 has vasodilatory, diuretic and natriuretic effects. Treatment with ACE inhibitors also reduces the formation of other vasoconstrictor and antinatriuretic substances, such as norepinephrine, arginine vasopressin, and endothelin-1 [12].
Hemodynamic effects when using ACE inhibitors are manifested:
- a decrease in total vascular resistance due to an indirect vasodilating effect, which leads to a decrease in blood pressure by 15–25%;
- relaxation of volume vessels with a decrease in filling pressure of the left ventricle;
- increased minute blood volume;
- an increase in renal blood flow due to dilatation of efferent arterioles in the glomeruli [11].
Classification of ACE inhibitors. Despite the common mechanism of action, ACE inhibitors differ in chemical structure, the presence of additional functional groups in the molecule, the nature of the prodrug, activity and pharmacokinetic profile, which is very important to consider when treating patients with various pathologies of the digestive organs [3].
The most popular chemical classification, according to which drugs are divided into four main classes depending on which chemical group in their molecule binds to the zinc ion in the active centers of the angiotensin I-converting enzyme:
- preparations containing a sulfhydryl group;
- drugs containing a carboxyl group;
- preparations containing a phosphinyl group;
- drugs containing the hydroxamic group [15].
Analysis of literature data shows that according to the duration of the antihypertensive effect, ACE inhibitors can be divided into two groups:
- medium duration - captopril;
- long-acting - enalapril, lisinopril, quinapril, which in most cases provide round-the-clock control over blood pressure levels when taken once a day.
Taking into account data on physicochemical properties and pharmacokinetic characteristics, ACE inhibitors are divided into three classes:
1. Lipophilic ACE inhibitors (captopril), which themselves have pharmacological activity, but undergo further transformations in the liver to form pharmacologically active disulfides, which are eliminated by renal excretion.
2. Lipophilic prodrugs (pharmacologically inactive) become active diacid metabolites after metabolic transformation in the liver (enalapril to enalaprilat), which are then transformed into inactive compounds [13]. In patients with liver pathology, both of these processes are impaired, and with a decrease in blood flow in the liver, there is a delay in the conversion of the prodrug to its active form during the first passage through it.
Accordingly, in liver diseases, drugs that require transformation to acquire activity have a weaker effect [6, 14].
Prodrugs are more lipophilic than their pharmacologically active metabolites, which allows them to ensure rapid and complete absorption when taken orally.
ACE inhibitors of this class should be divided into three subgroups depending on the predominant route of elimination of their active diacid metabolites:
- subclass A - drugs with predominantly renal elimination;
- subclass B - drugs with two main elimination routes;
- subclass C - drugs with predominantly hepatic elimination.
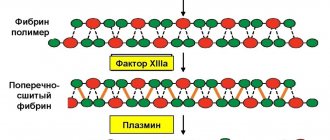
3. Hydrophilic drugs (lisinopril), which are not metabolized in the patient’s body. They circulate in the blood in a form unbound to plasma proteins and are eliminated unchanged through the kidneys. Their concentration in the blood plasma is determined by the dose taken orally, as well as the rate of absorption and the rate of excretion through the kidneys [16, 19, 26].
Only four ACE inhibitors (captopril, libenzapril, lisinopril and ceronapril) directly have biological activity. All other ACE inhibitors themselves are inactive substances or pro-drugs, i.e., they exhibit their effect after biotransformation in the liver and the formation of active metabolites [25].
The degree of blocking of the tissue renin-angiotensin system by various ACE inhibitors varies. Drugs that are characterized by less lipophilicity cause less accumulation of bradykinin in tissues, which is associated with the appearance of a side effect - dry cough.
Lisinopril is a well-studied ACE inhibitor, the benefit of which has been proven in the treatment of patients with hypertension.
Lisinopril is an active pharmacological compound.
Lisinopril was the third ACE inhibitor (after captopril and enalapril) of the drugs in this group that entered clinical practice.
Lisinopril has a prolonged antihypertensive effect. The onset of the antihypertensive effect is 1–3 hours after oral administration, the peak of action is after 6 hours, the duration of action is 24 hours with a stable effect after 2–4 weeks of treatment [4, 5].
The antihypertensive effect lasts more than a day. In case of abrupt cessation of therapy with lisinopril, there is no sudden increase in blood pressure, as well as a significant increase in blood pressure values before the start of treatment.
Lisinopril causes dilatation of arterioles and veins, which leads to a decrease in blood pressure by approximately 15% due to a decrease in total peripheral vascular resistance. Lisinopril does not cause reflex tachycardia due to stimulation of the vagus nerve and a decrease in the sensitivity of carotid sinus baroreceptors due to improved compliance and dilatation of the carotid artery.
Pharmacokinetics
After oral administration, the bioavailability of lisinopril is 25–29%. The functional state of the liver does not affect bioavailability. Eating does not change the absorption of the drug from the gastrointestinal tract. In the human body it is not metabolized and is excreted unchanged in the urine. In blood plasma, lisinopril does not bind to proteins. The half-life is 12.6 hours. The drug undergoes glomerular filtration, is secreted and reabsorbed in the tubules. The maximum concentration is achieved 6 hours after taking a single dose, and the steady-state level of concentration with regular use is achieved after 2-3 days.
For hypertension, the initial dose is 10 mg/day for a single dose, followed by a possible gradual increase to 40 mg/day.
Thus, when treating patients with hypertension with pathology of the digestive organs, the doctor has the opportunity to choose a drug from various classes of ACE inhibitors, depending on their pharmacokinetic characteristics.
In our work, we assessed the effectiveness of an ACE inhibitor (lisinopril) in the treatment of patients with hypertension with various pathologies of the digestive organs.
Purpose of the study
To evaluate the pharmacodynamics of lisinopril in various diseases of the digestive system in patients with hypertension.
Materials and research methods
The study included 60 patients with hypertension in combination with steatosis (group 1), liver cirrhosis (group 2), duodenal ulcer (group 3), 20 people in each group, respectively.
Titration of lisinopril dosages was carried out weekly under the control of 24-hour blood pressure monitoring (ABPM). Based on complaints, medical history and examination (blood tests, esophagogastroduodenoscopy, ultrasound examination of the abdominal organs), the presence of pathology in the liver and upper digestive tract was established. Patients with duodenal ulcer with normal liver function constituted the comparison group (Table 1).
To assess the effectiveness of lisinopril, ABPM was carried out using the ABRM-02 monitor using the oscillometric method of measuring blood pressure in a free motor mode. Registration was carried out on the “non-working” arm in the absence of blood pressure asymmetry. If blood pressure asymmetry is more than 5 mm Hg. Art. the study was conducted on the arm with higher scores. Blood pressure measurements were carried out for 24 hours every 15 minutes from 6.00 to 22.00 hours and every 30 minutes from 22.00 to 6.00 hours.
In order to clarify the daily blood pressure profile and assess the hypotensive effect of lisinopril, average blood pressure values were determined based on ABPM data. Normally, during the daytime, blood pressure should not exceed 140 and 90 mmHg. Art., at night - 120 and 80 mm Hg. Art. As an indicator of pressure load, we assessed the time index (TI) - the percentage of time during which blood pressure exceeds the critical level for certain time periods (in accordance with the recommendations of the American Society of Hypertension, a VI of more than 30% indicates the presence of elevated blood pressure) [3].
Statistica 5.0 program was used for statistical data processing. For each indicator, the mean value and standard deviation from the mean value were calculated. The statistical significance of changes in indicators was determined using Fisher's test. Differences were considered statistically significant at p < 0.05.
Results and its discussion
According to ABPM data, a persistent increase in blood pressure was initially detected in all examined patients; no significant differences were found between the groups.
The effectiveness of therapy was assessed after 1, 2, 3 and 4 weeks according to the VI ABPM level: good - with VI less than 30%, unsatisfactory - with VI more than 30%.
If lisinopril was insufficiently effective, the dose was gradually increased to 20 mg (Tables 2, 3).
As can be seen from table. 2 and 3, during therapy with lisinopril at a dose of 10 mg/day, a decrease in average daily blood pressure and blood pressure values was noted in all three groups. When treated with lisinopril, a good antihypertensive effect was obtained in 50% of patients with liver cirrhosis. In 60% of patients with duodenal ulcer, a good effect was achieved when taking 10 mg/day, in 30% of patients - 20 mg/day.
Insufficient effectiveness of lisinopril therapy was observed in 15% of cases in patients with liver cirrhosis and in 10% in patients with duodenal ulcer, even when the dose of the drug was doubled.
Conclusion
The results of this study indicate that the effectiveness of lisinopril monotherapy did not depend on the severity of liver changes in patients with hypertension.
In this regard, the use of antihypertensive drugs that are not metabolized in the liver, which can provide adequate blood pressure control for 24 hours in hypertensive patients with gastrointestinal pathology, becomes especially relevant [2, 8].
Thus, lisinopril is a highly effective antihypertensive drug in the treatment of patients with various pathologies of the digestive system.
Literature
- Belenkov Yu. N., Mareev V. Yu., Ageev F. T. Angiotensin-converting enzyme inhibitors in the treatment of cardiovascular diseases (quinapril and endothelial dysfunction). M., 2001. 86 p.
- Drapkina O. M., Mayevskaya M. V., Korneeva O. N., Tutnov D. A., Ivashkin V. T. Clinical study of the effectiveness and safety of dapril (lisinopril) in liver pathology and concomitant arterial hypertension // Russian Medical News . 2004, No. 2, p. 39–42.
- Kobalava Zh. D. Kotovskaya Yu. V., Khirmanov V. N. Blood pressure in research practice. Ed. V. S. Moiseeva, R. S. Karpova. M.: Reafarm, 2004. 384 p.
- Komissarenko I. A., Lazebnik L. B., Mikheeva O. M. Features of the metabolism of antihypertensive drugs in patients with pathology of the digestive organs // Cardiovascular therapy and prevention. Appendix 1. 2009. 8 (6). P. 239.
- Komissarenko I. A., Mikheeva O. M., Drozdov V. N., Petrakov A. V., Silvestrova S. Yu. The use of angiotensin-converting enzyme inhibitors in patients with arterial hypertension against the background of liver pathology // Consilium medicum. 2007. T. 9. No. 11. P. 72–75.
- Kushakovsky M. S. Hypertension. St. Petersburg: Sotis, 1995. pp. 243–253.
- Lazebnik L. B., Drozdov V. N. Diseases of the digestive organs in the elderly. Anacharsis, 2003, pp. 37–39.
- Lazebnik L. B., Mikheeva O. M., Komissarenko I. A., Drozdov V. N., Petrakov A. V., Silvestrova S. Yu. Features of treatment of patients with hypertension with ACE inhibitors for pathology of the digestive organs // Experimental and Clinical gastroenterology, 2007. No. 4. pp. 47–55.
- Mazur N. A. Efficacy of non-lipophilic angiotensin-converting enzyme inhibitors in the treatment of cardiovascular diseases // Russian Journal of Cardiology. 2003. No. 4 (42). pp. 76–79.
- Mareev V. Yu. Application of ACE inhibitors in the treatment of cardiovascular diseases in the 21st century. Why is it beneficial to choose fosinopril? Heart diseases. Guide for doctors. Ed. R. G. Oganova, I. G. Fomina. M.: Litterra, 2006. pp. 3–8.
- Metelitsa V.I. Handbook of clinical pharmacology of cardiovascular drugs. St. Petersburg - M.: Binom. 2nd ed. 2002. 925 p.
- Preobrazhensky D.V., Sidorenko B.A. Treatment of arterial hypertension. M., 1999. pp. 126–136.
- Savenkov M.P., Ivanov S.N., Botsoeva M.A., Mikhailusova M.P. Correction of high blood pressure in the morning with the help of ACE inhibitors // Gedeon Richter in the CIS. 2001. No. 4 (8). pp. 27–30.
- Savenkov M.P., Ivanov S.N., Solomonova L.A., Savenkova A.M. Morning begins with dawn and increased blood pressure // Russian Medical Journal. 2006. T. 14, No. 10. P. 734–736.
- Storozhakov G.I. ACE inhibitors: place in the treatment and prevention of cardiovascular diseases // Consilium medicum. Extra edition. 2002, January, p. 3–4.
- Tkhostova E. B. Clinical effectiveness of lisinopril in patients with cardiovascular diseases // Gedeon Richter in the CIS. 2001. No. 4 (8). pp. 23–25.
- ALLHAT Authors. Major Outcomes in High-Risk Hypertensive Patients Randomized to Angiotensin-Converting Enzyme inhibitor or Calcium channel blocker VS Diuretic. JAMA, December 18, 2002, 288, 23, 2981–2996.
- Campbell DJ, Kladis A., Duncan AM Effects of converting enzyme inhibitors on angiotensin and bradykinin peptides // Hypertens. 1994, 23: 439–449.
- Choodoff L. Lisinopril: a new ACE inhibitor for the treatment of hypertension and congestive heart failure // Mt. Sinai. J. Med. 1990. Vol. 57. P. 169–171.
- Furberg CD, Pitt B. Are all angiotensin-converting enzyme inhibitors interchangeable? // Am Coll Cardiol. 2001, 37, 1456–1460.
- Gruppo Italiano per to Studio della Sopravvivenza nell'Infarto Miocardico (GISSI-3). Effects of lisinopril and transdermal glyceryl trinitrate singly and together on six-week mortality and ventricular function after acute myocardial infarction // Lancet. 1994; 343:1115–1122.
- Hansson L., Lindholm LH, Ekbom T. et al. Randomized trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 Study // Lancet. 1999, 354, 1751–1756.
- ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group (ISIS-4). A randomized factorial trial assessing early oral captopril, oral mononitrate and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction // Lancet. 1995; 345:669–685.
- Kober L. et al. for the Trandolapril Cardiac Evaluation (TRACE) Study Group // N Engl J Med. 1995: 333: 1670–1676.
- Lancaster SG, Todd PA Lisinopril: a preliminary review of its pharmacodynamic and pharmacokinetic properties and therapeutic use in hypertension and congestive heart failure // Drugs. 1988, 35: 646–669.
- Opie HL Angiotensin-converting enzyme inhibitors. Wiley-Liss-Authors Publishing. New York, 1992.
- Packer M., Poole-Wilson PA, Armstrong PW et al. Comparative effects of low and high doses of angiotensin-converting enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS Study Group // Circulation. 1999; 100(23):2312–2318.
- Pfeffer MA et al. On behalf of the SAVE Investigators. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction: results of the Survival And Ventricular Enlargement trial // N Engl J Med. 1992; 327:669–677.
- The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure // Lancet. 1993; 342:821–828.
- The CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS) // N Engl J Med/1987; 316:1429–1435.
- The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients // N Engl J Med. 2000; 342:145–153.
- The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart future // N Engl J Med. 1991; 325; 293–302.
L. B. Lazebnik, Doctor of Medical Sciences, Professor O. M. Mikheeva, Doctor of Medical Sciences, Professor I. A. Komissarenko, Doctor of Medical Sciences, Professor
State Budgetary Educational Institution of Higher Professional Education MGMSU Ministry of Health and Social Development of Russia, Central Research Institute of Gastroenterology of the City Health Department, Moscow
Contact information for authors for correspondence
What is lisinopril prescribed for?
The name of the drug suggests that it belongs to the so-called group of “by-catch”, the action of which is primarily aimed at lowering blood pressure in the fight against hypertension. However, a doctor may prescribe treatment with Lisinopril in other cases:
- for chronic heart failure;
- in acute myocardial infarction not accompanied by arterial hypotension;
- to combat nephropathy of diabetic etiology, both type 1 and type 2.
- with arterial hypertension.
Self-administration of the drug is unacceptable. The dose, frequency of doses and duration of treatment are determined only by the doctor.
conclusions
Lisinopril is a long-acting ACE inhibitor that is highly effective. The drug is considered the “gold standard” in the treatment of hypertension and circulatory failure (together with diuretics, statins, angiotensin-II antagonists and Ca2+ channel blockers). The combined use of Lisinopril and Indapamide reduces the likelihood of recurrent episodes of ischemic stroke by 29% and intracranial hemorrhage by 50%.
It is worth remembering that the antihypertensive effect reaches a plateau no earlier than 10-14 days from the start of treatment.
Before using the drug, you must carefully read the instructions! Lisinopril should not be taken without a doctor’s prescription, and you should not replace it with an analogue yourself.
Contraindications to the use of Lisinopril
Contraindications to the use of Lisinopril are pregnancy and breastfeeding. If the expectant mother suffers from hypertension, her condition is monitored in a hospital setting. High blood pressure in such cases is corrected with safe doses of diuretics.
If replacing the drug during breastfeeding is not possible, you should definitely transfer the child to artificial feeding or feeding with donor milk.
Other contraindications are:
- excess potassium in the blood;
- renal dysfunction;
- gout;
- renal artery stenosis;
- elderly age;
- cerebrovascular insufficiency;
- hypotension;
- childhood;
- tissue obstruction that interferes with normal outflow;
- availability of a donor kidney.
Lisinopril: instructions for use
The drug is taken once a day. It is important to observe the time interval between medication doses. Superimposing the effect of one dose on another threatens severe hypotension, up to loss of consciousness.
If the first tablet was taken at lunch, then the second tablet should not be taken in the morning hours of the next day. It is important to keep taking your medication at lunchtime.
A single dose is prescribed by the attending physician based on the following studies:
- blood pressure conditions;
- heart function;
- vascular health;
- risk factors.
If an increase in the single dose is not required, as a rule, a single dose of 2.5 mg of Lisinopril is sufficient to normalize the patient's condition. Dose adjustments can be made no earlier than after 4 weeks of continuous use of the drug, since it is after this time that the maximum possible therapeutic effect is achieved.
If increasing the dose does not give the required result, a similar drug from a different pharmacological group is prescribed, the action of which in a different way will help normalize blood pressure.
If treatment of an insulin-dependent patient is required, Lisinopril is taken under the strict supervision of a specialist in a hospital setting.