pharmachologic effect
Manufacturer: ALSI-pharma, Pranapharm, VERTEKS, Ozone, Russia
Release form: tablets
Active ingredient: Lisinopril
Synonyms: Diroton, Irumed, Lisinoton, Liziprex, Lysigamma, Daprel
The drug belongs to the second generation ACE inhibitors, since it causes a decrease in blood pressure by blocking the formation of the vasoconstrictor factor - angiotensin II.
Selection of analogues
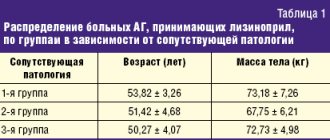
If the patient is not satisfied with the price, it is recommended to select an analogue with the same active ingredient, but at a lower cost. If there are contraindications, look for a product with another active ingredient that will not cause negative effects. The data is shown in the table.
| A drug | Active substance | Leader | Price |
| Diroton | Lisinopril dihydrate | Gedeon Richter | 180-450 |
| Losartan | Losartan potassium | Teva | 150 |
| Lorista | Losartan potassium | KRKA-RUS | 180-380 |
| Perindopril | Perindopril erbumine | PRANAFARM | 110-280 |
| Enalapril | Enalapril maleate | Valenta Pharmaceuticals | 12-80 |
| Enap | Enalapril maleate | KRKA | 70-90 |
| Prestarium | Pirindopril arginine | Les Laboratories Secrier | 450-550 |
To choose the right substitute, you need to undergo laboratory blood tests, ECG, and ultrasound of the heart. Based on the data obtained, the patient’s well-being and concomitant diseases are determined. Side effects and contraindications for each drug are taken into account. Select the most effective remedy that does not negatively affect the body. Otherwise it is not applicable.
Comparison with Perindopril
Perindopril is a medicine based on perindopril erbumine. It is an ACE inhibitor that quickly lowers blood pressure. The action occurs by suppressing the rate of transition of angiotensin 1 to angiotensin 2. Indications for use:
- arterial hypertension;
- heart failure;
- prevention of recurrent stroke;
- cardiac ischemia.
According to the mechanism of action and indications for use, Perindopril is similar to Lisinopril. Both substances are ACE inhibitors that lower blood pressure. They have a large number of side effects. Negative effects occur in relation to the gastrointestinal tract, cardiovascular, nervous, and immune systems.
Similar contraindications for use; both medications are prohibited for use in childhood, pregnancy and lactation.
Perindopril and Lisinopril are similar in their effect on the body, reducing blood pressure. If a person is not recommended to use ACE inhibitors, it is better to take Lozap. They indirectly affect the transition of angiotensin.
Comparison with Enalapril
Enalapril is a product based on enalapril maleate. It is one of the cheapest drugs that stops an attack of arterial hypertension. This is an ACE inhibitor that slows down the transition of angiotensin 1 to the second form. Indications for use:
- arterial hypertension;
- treatment and prevention of heart failure;
- prevention of coronary ischemia in the presence of a history of myocardial infarction and angina pectoris.
Compared to other medications, it causes far fewer side effects. Therefore, it is often prescribed to patients with intolerance to other groups of antihypertensive drugs. Possible negative reactions:
- headache, fatigue, depression, tinnitus;
- orthostatic hypotension, fainting;
- dyspeptic reactions, inflammation of the liver and pancreas;
- violation of the ratio of blood cells;
- decreased kidney function;
- cough, rash, Quincke's edema.
Despite the presence of many positive qualities, the drug is contraindicated for some patients. For example, with a history of systemic allergic reactions, diabetes mellitus, pregnancy, lactation, and adolescence.
Comparison between Losartan and Lorista
Losartan, Lorista are medications that have an identical active ingredient in the form of losartan potassium. They are similar to the action of Lozap. They have similar side effects, contraindications, and mechanisms of action. All 3 drugs do not affect ACE inhibition. Therefore, there are fewer contraindications.
Blood pressure decreases for a shorter period, then returns to its previous levels.
The medicine is produced in tablets that are taken daily to maintain the effect on the body. The greater the concentration of the active component in the systemic circulation, the stronger the antihypertensive effect. But gradually it can be eliminated if there is addiction. If the effectiveness decreases, it is necessary to undergo a re-examination to determine the best drug.
When choosing one of the drugs, they are guided by price. Losartan and Lozap have the smallest. Lorista has a high cost due to the manufacturer's markup.
If the patient's intravascular pressure gradually increases, switch from the active substance losartan to any ACE inhibitor. The effect on the body is much longer lasting. An experienced doctor will select a drug that has the least number of negative effects, taking into account the patient’s state of health and age.
Lisinopril analogs
Only a doctor can decide what can replace Lisinopril. Analogs and substitutes for Lisinopril are both synonyms and other ACE inhibitors, such as Fosicard, Hartil and Enalapril.
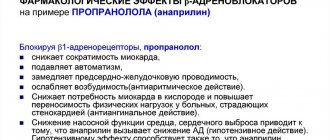
In addition, there are analogues of Lisinopril without the side effects characteristic of ACE inhibitors. These are adrenergic blockers Anaprilin, Concor and others, as well as sartans - angiotensin antagonists (Lozap, Valsacor, Telzap, Giposart).
Calcium channel blockers, for example, Amlodipine, also reduce blood pressure, and therefore can be considered analogues of the drug Lisinopril, either alone or in combination.
A comparison of the prices of some analogues is given in the table
| A drug | Active substance | Average price for average monthly dose, rub. | Country of origin |
| Lisinopril | Lisinopril | 100 | Russia |
| Diroton | Lisinopril | 300 | Hungary |
| Enalapril | Enalapril | 50 | Russia/India |
| Hartil | Ramipril | 350 | Hungary |
| Lozap | Losartan | 250 | Slovakia |
| Lorista | Losartan | 150 | Slovenia |
| Telzap | Telmisartan | 250 | Türkiye/Russia |
| Phosicard | Fosinopril | 250 | Iceland |
| Concor | Bisoprolol | 300 | Germany |
| Physiotens | Moxonidine | 300 | Germany |
| Perindopril | Perindopril | 200 | Russia |
| Noliprel | Perindopril arginine + Indapamide | 500 | France |
| Captopril | Captopril | 30 | Russia/India |
| Amlodipine | Amlodipine | 80 | Russia |
| Prestarium | Perindopril | 350 | France |
| Valsacor | Valsartan | 300 | Slovenia |
| Indapamide | Indapamide | 30 | Russia |
Hartil
Manufacturer: Egis, Hungary
Release form: tablets
Active ingredient: Ramipril
Synonyms: Amprilan, Tritace, Dilaprel, Vazolong
The analogue of Lisinopril in tablets Hartil is an ACE inhibitor, used for arterial hypertension, treats chronic heart failure, nephropathy and reduces the risk of stroke and myocardial infarction.
Telzap
Manufacturer: Sanofi, Turkey/Russia
Release form: film-coated tablets
Active ingredient: Telmisartan
Synonyms: Mikardis, Praytor, Tanidol, Telmista, Telmisartan-SZ, Telmisartan STADA
The Telzap analogue contains Telmisartan, which is an angiotensin receptor antagonist and also lowers blood pressure and is used for hypertension.
Concor
Manufacturer: Merck, Germany
Release form: film-coated tablets
Active ingredient: Bisoprolol
Synonyms: Biprol, Biol, Bisogamma, Coronal, Niperten
The Concor analogue is a beta-blocker - it lowers blood pressure and has an antianginal and antiarrhythmic effect and is used for hypertension, angina pectoris and arrhythmia.
Phosicard
Manufacturer: Actavis, Iceland
Release form: tablets
Active ingredient: Fosinopril
Synonyms: Monopril, Fosinap, Fosinopril-OBL
The analogue Fosicard is also an ACE inhibitor, has a hypotensive, vasodilating and cardioprotective effect in hypertension and chronic heart failure.
Physiotens
Manufacturer: Solway, Germany
Release form: film-coated tablets
Active ingredient: Moxonidine
Synonyms: Moxonidine-SZ, Moxarel, Moxogamma
The Physiotens analogue is an imidazoline receptor agonist, that is, a centrally acting antihypertensive agent, used only for hypertension, but unlike Lisinopril, it has minimal side effects.
Noliprel
Manufacturer: Servier, France
Release form: film-coated tablets
Active ingredient: Perindopril arginine + Indapamide
The Noliprel analogue is a combination drug consisting of two antihypertensive drugs, which, when used together, enhance the effect of each other.
Used for hypertension and to reduce the risk of vascular complications of diabetes.
Lisinopril Stada tablets 5 mg 30 pcs ➤ instructions for use
Orally, regardless of food intake, 1 time per day in the morning, preferably at the same time. The dose is selected individually.
To ensure the dosage regimen of the drug at a dose of 2.5 mg, it is recommended to use tablets of 2.5 mg or 1/2 tablet of 5 mg with a score.
For arterial hypertension (in patients not receiving other antihypertensive drugs):
the initial dose is 5-10 mg 1 time per day, depending on the patient’s condition. If there is no effect, the dose is increased every 2 weeks by 5 mg to an average therapeutic dose of 20-40 mg/day (a dose above 40 mg/day usually does not lead to a further decrease in blood pressure). The usual maintenance dose is 20 mg/day. The maximum daily dose is 40 mg.
The therapeutic effect usually develops within 2-4 weeks from the start of treatment, which should be taken into account when increasing the dose. If the therapeutic effect is insufficient, the drug can be used in combination with other antihypertensive drugs.
If the patient is receiving diuretic therapy, then these drugs should be stopped 2-3 days before starting lisinopril. If it is impossible to discontinue diuretics, the initial dose of lisinopril should not exceed 5 mg/day. In this case, after taking the first dose, medical supervision is recommended for several hours, taking into account the maximum hypotensive effect after 6 hours (a pronounced decrease in blood pressure may develop).
For renovascular hypertension or other conditions associated with increased activity of the renin-angiotensin-aldosterone system (RAAS) (hypovolemia, diet with limited salt intake, cardiac decompensation or severe hypotension):
the initial dose is 2.5-5 mg per day under strict medical supervision (monitoring blood pressure, kidney function, potassium levels in the blood serum). The maintenance dose, while continuing strict medical supervision, should be determined depending on the dynamics of blood pressure.
For renal failure
Due to the fact that lisinopril is excreted through the kidneys, the initial dose is determined depending on creatinine clearance. Further, in accordance with the therapeutic effect and tolerability, a maintenance dose should be established under conditions of frequent monitoring of renal function, potassium and sodium levels in the blood serum.
| Creatinine clearance, ml/min | Initial dose, mg/day |
| 31-80 | 5-10 |
| 10-30 | 2,5-5 |
| less than 10** | 2,5 |
*including patients on hemodialysis
For persistent arterial hypertension, long-term maintenance therapy of 10-15 mg/day is indicated.
For chronic heart failure
The initial dose is 2.5 mg 1 time per day, followed by an increase in dose by 2.5 mg after 1-2 weeks to a maintenance daily dose of 5-20 mg, depending on the dynamics of blood pressure. The maximum daily dose is 20 mg.
In elderly patients (over 65 years old)
a more pronounced and prolonged antihypertensive effect is often observed, which is associated with a decrease in the rate of elimination of lisinopril (it is recommended to start treatment with a dose of 2.5 mg per day).
Acute myocardial infarction (as part of combination therapy):
in early (in the first 24 hours) treatment of patients with stable hemodynamic parameters (systolic blood pressure at least 100 mm Hg) to maintain these parameters and prevent left ventricular dysfunction and heart failure - on the first day the dose is 5 mg, then 5 mg after 1 day, 10 mg after two days and then 10 mg 1 time per day as maintenance therapy. In patients with acute myocardial infarction, the drug should be used for at least 6 weeks.
Patients with low systolic blood pressure (120 mmHg or lower) at the beginning of treatment or during the first 3 days after acute myocardial infarction should receive the drug at a dose of no more than 2.5 mg per day.
In case of decreased blood pressure (systolic blood pressure is less than or equal to 100 mm Hg), the daily dose of 5 mg can be temporarily reduced to 2.5 mg if necessary. In case of prolonged pronounced decrease in blood pressure (systolic blood pressure below 90 mm Hg for more than 1 hour), the drug should be discontinued.
For diabetic nephropathy
10 mg of lisinopril is used once a day. The dose, if necessary, can be increased to 20 mg 1 time per day in order to achieve diastolic blood pressure values below 75 mm Hg. Art. in the sitting position for patients with type 1 diabetes mellitus and below 90 mmHg. Art. in the sitting position in patients with type 2 diabetes mellitus.
Lisinopril or Lozap – which is better?
Manufacturer: Zentiva, Slovakia
Release form: film-coated tablets
Active ingredient: Losartan
Synonyms: Lorista, Cozaar, Bloktran, Losarel, Vero-Losartan, Renicard
Lozap is part of the group of sartans - angiotensin receptor antagonists, due to which, after taking this analogue, angiotensin II ceases to act in the body and blood pressure does not increase.
The Lozap analogue is used not only to lower blood pressure, but also to prevent various cardiovascular diseases accompanied by high blood pressure.
According to reviews, those who take Lozap regularly, their blood pressure stops rising.
Lozap Plus also contains the diuretic component Hydrochlorothiazide, which enhances the hypotensive effect of Losartan and allows you to reduce the therapeutic dose.
Comparative characteristics of Lisinopril and Lozap
Both drugs have antihypertensive effects. They are effective and low cost. The following similarities are highlighted:
- in addition to the main indication in the form of arterial hypertension, they are prescribed for increased blood pressure due to complications of diabetes mellitus, heart failure;
- a large number of side effects that must be taken into account when prescribing and using the drug;
- use of substances for serious diseases of internal organs, in old age, but under the supervision of a doctor;
- possibility of overdose.
Since the active ingredients are different, the drugs differ from each other. Because of this difference, a doctor may prescribe one drug and refuse another. The following differences are distinguished:
- Lisinopril inhibits ACE, Lozap does not;
- substances differ in pharmacokinetics, Lozap has metabolites;
- Lisinopril can additionally be used for myocardial infarction;
- Lozap does not have the ability to block angiotensin receptors, so the decrease in blood pressure does not occur directly, but indirectly.
Both substances are useful for arterial hypertension. Lisinopril is most often recommended; it affects ACE. If the patient has contraindications to it, Lozap is prescribed. It is less likely to cause negative actions.
Lisinopril or Enalapril - which is better for blood pressure
Manufacturer: Izvarino, Organika, Ozone, Russia
Release form: film-coated tablets
Active ingredient: Enalapril
Synonyms: Enap, Renipril, Enam, Berlipril, Renitek, Enalapril-ACRI
The analogue Enalapril is included in the same therapeutic group - it is also an ACE inhibitor.
Basically, this is a Russian-made analogue, and Enalapril is the international non-proprietary name of some imported analogues, such as Renitek, Berlipril and other drugs.
According to doctors, Lisinopril is considered more effective than Enalapril, however, it all depends on the individual reactions of the body.
Lisinopril
Arterial hypotension
Most often, a pronounced decrease in blood pressure occurs with a decrease in blood volume caused by diuretic therapy, a decrease in the content of sodium chloride in food, dialysis, diarrhea or vomiting. In patients with CHF and with or without concurrent renal failure, a pronounced decrease in blood pressure is possible. When using the drug Lisinopril, some patients with CHF, but with normal or reduced blood pressure, may experience a marked decrease in blood pressure, which is usually not a reason to discontinue treatment.
In such patients, treatment with Lisinopril should be started under the strict supervision of a physician (with caution in selecting the dose of the drug and diuretics).
Before starting treatment with the drug, if possible, the sodium content should be normalized and/or the blood volume should be replenished, and the effect of the initial dose of Lisinopril on the patient should be carefully monitored.
Under strict medical supervision, Lisinopril should be used in patients with coronary heart disease, cerebrovascular insufficiency, in whom a sharp decrease in blood pressure can lead to myocardial infarction or stroke. Transient arterial hypotension is not a contraindication for further use of the drug. After blood pressure has been restored, it is possible to continue using the drug.
Renal dysfunction
In patients with impaired renal function (creatinine clearance less than 80 ml/min), the initial dose of lisinopril should be changed in accordance with the creatinine clearance (see section "Dosage and Administration"). Regular monitoring of potassium levels and creatinine concentrations in blood plasma is a mandatory treatment strategy for such patients. In patients with CHF, arterial hypotension can lead to deterioration of renal function. Cases of acute renal failure, usually reversible, have been reported in such patients. In case of acute myocardial infarction, drug therapy should not be started in patients with signs of renal impairment, i.e. with a plasma creatinine concentration of 177 µmol/l and/or proteinuria more than 500 mg/day. If renal function is impaired during the use of the drug (creatinine concentration exceeds 265 µmol/l or its value doubles before the start of therapy), it is necessary to consider discontinuing the drug.
Renal artery stenosis
In case of renal artery stenosis (especially with bilateral stenosis or in the presence of stenosis of the artery of a single kidney), as well as with peripheral circulatory failure due to a lack of sodium ions and/or fluid, the use of the drug Lisinopril can lead to impaired renal function, acute renal failure, which usually turns out to be irreversible even after discontinuation of the drug.
In acute myocardial infarction
The drug Lisinopril can be used simultaneously with standard therapy for acute myocardial infarction (thrombolytics, acetylsalicylic acid as an antiplatelet agent, beta-blockers).
The drug Lisinopril can be used simultaneously with a solution of nitroglycerin for intravenous administration or with nitroglycerin for administration using therapeutic transdermal systems, as well as nitroglycerin for sublingual use. The use of Lisinopril is not recommended in patients who have suffered acute myocardial infarction if systolic blood pressure does not exceed 100 mmHg. rt. Art. In case of persistent arterial hypotension (SBP less than 90 mm Hg for more than 1 hour), the drug must be discontinued.
Surgery/general anesthesia
During extensive surgical interventions, as well as when using other drugs that cause a decrease in blood pressure, lisinopril, by blocking the formation of angiotensin II, can cause a pronounced, unpredictable decrease in blood pressure. Before surgery (including dentistry), the surgeon/anesthesiologist should be informed about the use of an ACE inhibitor.
In elderly patients, the use of standard doses leads to higher concentrations of lisinopril in the blood, so special care is required when determining the dose.
Mitral stenosis/aortic stenosis/hypertrophic obstructive cardiomyopathy
Lisinopril, like other ACE inhibitors, should be administered with caution to patients with left ventricular outflow tract obstruction (aortic stenosis, hypertrophic obstructive cardiomyopathy), as well as to patients with mitral stenosis.
Anaphylactoid reactions during desensitization
There are isolated reports of the development of anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy, for example, with hymenoptera venom. ACE inhibitors should be used with caution in patients susceptible to allergic reactions undergoing desensitization procedures. The use of ACE inhibitors should be avoided in patients receiving bee venom immunotherapy. However, this reaction can be avoided by temporarily discontinuing the ACE inhibitor before starting the desensitization procedure.
Hypersensitivity/angioedema
Angioedema of the face, extremities, lips, tongue, epiglottis and/or larynx, which may occur during any period of treatment, has rarely been reported in patients taking an ACE inhibitor, including lisinopril. In this case, treatment with the drug should be stopped as soon as possible, and the patient should be monitored until symptoms completely regress. Angioedema with laryngeal edema can be fatal. Swelling of the tongue, epiglottis or larynx can cause airway obstruction, so appropriate therapy (0.3-0.5 ml of 1:1000 epinephrine (adrenaline) solution subcutaneously) and/or measures to ensure airway patency should be immediately carried out. In cases where the swelling is localized only on the face and lips, the condition most often goes away without treatment, but the use of antihistamines is possible.
The risk of developing angioedema is increased in patients who have a history of angioedema not associated with previous treatment with ACE inhibitors.
In rare cases, intestinal angioedema develops during therapy with ACE inhibitors. In this case, patients experience abdominal pain as an isolated symptom or in combination with nausea and vomiting, in some cases without previous angioedema of the face and with normal levels of Cl-esterase. The diagnosis is made using computed tomography of the abdominal cavity, ultrasound, or at the time of surgery. Symptoms disappear after stopping ACE inhibitors. In patients with abdominal pain taking ACE inhibitors, the possibility of developing angioedema of the intestine must be taken into account when making a differential diagnosis.
Concomitant use with mTOR inhibitors
(mammalian Target of Rapamycin - target of rapamycin in mammalian cells), for example, temsirolimus, sirolimus, everolimus, racecadotril (an enkephalinase inhibitor used to treat acute diarrhea), estramustine
In patients concomitantly receiving therapy with mTOR inhibitors, racecadotril, estramustine, the risk of developing angioedema (for example, swelling of the airways or tongue with or without impairment of respiratory function) may be increased (see section "Interaction with other drugs").
Anaphylactic reactions during low-density lipoprotein (LDL) apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during LDL apheresis using dextran sulfan. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued before each apheresis procedure.
Hemodialysis
Anaphylactoid reactions have also been observed in patients on hemodialysis using high-flow dialysis membranes (eg, AN69®) who are also taking ACE inhibitors. In such cases, the use of a different type of dialysis membrane or another antihypertensive agent should be considered.
Neutropenia/agranulocytosis/thrombocytopenia/anemia
During therapy with ACE inhibitors, neutropenia/agranulocytosis, thrombocytopenia and anemia may develop. With normal renal function and the absence of other complications, neutropenia rarely occurs. ACE inhibitors are used only in emergency cases in the presence of systemic vasculitis, immunosuppressive therapy, taking allopurinol or procainamide, as well as when combining all of these factors, especially against the background of previous renal failure. There is a risk of developing severe infectious diseases that are resistant to intensive antibiotic therapy. When carrying out therapy with Lisinopril in patients with the above factors, it is necessary to regularly monitor the number of leukocytes.
Lithium preparations
The combined use of Lisinopril and lithium preparations is not recommended (see section “Interaction with other drugs”).
Dry cough
Cough has been reported when using ACE inhibitors. The cough is dry and prolonged, which disappears after stopping treatment with an ACE inhibitor. In the differential diagnosis of cough, cough caused by the use of an ACE inhibitor must also be taken into account.
Ethnic differences
It should be taken into account that patients of the Negroid race have a higher risk of developing angioedema. Like other ACE inhibitors, lisinopril is less effective in lowering blood pressure in black patients. This effect may be associated with a pronounced predominance of low-renin status in black patients with arterial hypertension.
Double blockade of the RAAS
Cases of hypotension, syncope, stroke, hyperkalemia and renal dysfunction (including acute renal failure) have been reported in susceptible patients, especially when used concomitantly with drugs that affect this system. Therefore, double blockade of the RAAS by combining an ACE inhibitor with an ARA II or aliskiren is not recommended. Combination with aliskiren and drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or moderate or severe renal impairment (GFR <60 ml/min/1.73 m2 body surface area) (see sections "Contraindications" and "Interaction" with other drugs") and is not recommended in other patients.
Concomitant use of lisinopril and ARB II in patients with diabetic nephropathy is contraindicated and is not recommended in other patients.
Potassium-sparing diuretics, potassium supplements, potassium-containing table salt substitutes and food supplements
Concomitant use with ACE inhibitors is not recommended (see section “Interaction with other drugs”).
Patients with diabetes mellitus
When using the drug in patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, blood glucose concentrations should be regularly monitored during the first month of therapy.
Liver dysfunction
The use of ACE inhibitors can lead to the development of cholestatic jaundice with progression up to fulminant liver necrosis, so it is necessary to stop taking the drug if the activity of “liver” transaminases increases and symptoms of cholestasis appear.
Hyperkalemia
During therapy with ACE inhibitors, including lisinopril, hyperkalemia may develop. Risk factors for hyperkalemia include renal failure, old age, diabetes mellitus, certain concomitant conditions (for example, decreased blood volume, acute heart failure, metabolic acidosis), concomitant use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, amiloride), as well as potassium supplements or potassium-containing substitutes for table salt and the use of other drugs that increase the content of potassium in the blood plasma (for example, heparin). Hyperkalemia can cause serious heart rhythm problems, sometimes fatal. The simultaneous use of the above drugs should be carried out with caution.
Kidney transplant
There are no data on the use of lisinopril after kidney transplantation. Primary hyperaldosteronism
Patients with primary hyperaldosteronism are usually resistant to treatment with antihypertensive drugs that affect the RAAS. In this regard, Lisinopril is not recommended for use in such patients.
It is not recommended to drink alcohol (ethanol) during treatment with Lisinopril.
Lisinopril or Lorista – which is better?
Manufacturer: KRKA, Slovenia
Release form: film-coated tablets
Active ingredient: Losartan
Synonyms: Lozap, Cozaar, Bloktran, Losarel, Vero-Losartan, Renicard
The Lorist analogue is used in the same way as Lozap. Protects patients with diabetes from renal failure, is used for heart failure and to prevent high blood pressure.
Reviews from doctors about Lisinopril and Lorist are equally positive; each of these two drugs is popular among cardiologists.
Lisinopril or Perindopril
Manufacturer: Izvarino, Pranafarm, Promomed Rus, Russia
Release form: film-coated tablets
Active ingredient: Perindopril
Synonyms: Prestarium, Perineva, Coverex, Parnavel, Perindopril-Vertex, Perindopril-Teva
Perindopril is part of the group of AP inhibitors. Additionally, it reduces heart rate, reduces myocardial oxygen demand, restores vascular elasticity, and has a moderate diuretic effect. Therefore, the use of Perindopril is wider; in addition to hypertension, the drug is prescribed for angina pectoris and for the prevention of complications after strokes.
Accordingly, Perindopril can be considered more effective than Lisinopril.
Lisinopril: a universal drug in the arsenal of a cardiologist
It became possible to effectively influence the cardiovascular continuum with the introduction of diuretics and selective beta-blockers into clinical practice. The next stage was the emergence of angiotensin-converting enzyme inhibitors (ACEIs) and calcium antagonists (CAs), which contributed to further advances in the treatment of CVD. With good reason, the last quarter of the twentieth century can be called the “era of ACE inhibitors.” Today, five main classes of antihypertensive drugs - thiazide diuretics, ACE inhibitors, angiotensin receptor blockers (ARBs) and β-blockers (BABs) - are suitable for initiation and maintenance of antihypertensive treatment in monotherapy or in combination [2 ,3]. When choosing one or another antihypertensive drug, it is necessary to remember that it must not only adequately reduce blood pressure to the target level, control it throughout the day, improving the blood pressure profile, but also meet a number of other requirements: the drug must reduce the reabsorption of Na+ and water, and not increase dysfunction endothelium, do not activate the sympathetic nervous system, have organoprotective properties, and be metabolically neutral. These requirements are fully met by ACE inhibitors, of which there are today more than 30 original drugs and their generics. Their pharmacological action is due to their influence on the functional state of the renin–angiotensin–aldosterone system (RAAS). ACE inhibitors have a highly selective action: they suppress the conversion of angiotensin I to angiotensin II without directly interacting with other components of the RAAS. Summarizing the data on the properties and mechanism of action of ACE inhibitors, we can dwell on the main protective effects of this group of drugs: 1. Cardioprotective effects (restoring the balance between the need and supply of myocardium O2, reducing pre- and afterload of the left ventricle (LV), reducing volumes and weight, slowing LV remodeling, decreased sympathetic stimulation, antiarrhythmic effect). 2. Vasoprotective effects (potentially direct antiatherogenic effect, antiproliferative and antimigration effect on smooth muscle cells, monocytes, neutrophils; improved endothelial function, antiplatelet effect, increased endogenous fibrinolysis, improved arterial compliance and tone). Among the many representatives of the ACEI class, lisinopril deserves special attention. Lisinopril (Diroton®, produced by the pharmaceutical company) is an ACE inhibitor with an extremely wide spectrum of action and original properties, which allows it to be used in a wide variety of situations. In addition, a large evidence base has been accumulated on the effectiveness and safety of lisinopril based on the results of a number of clinical studies. Lzinopril (Diroton) is the only hydrophilic ACEI, practically does not bind to plasma proteins and is not distributed in adipose tissue. The chemical structure of lisinopril contains a carboxyl group, which binds the zinc-containing domain of ACE. Unlike most ACE inhibitors, lisinopril is not a prodrug. Absorbed into the gastrointestinal tract, it does not undergo further metabolic transformations and is excreted unchanged by the kidneys. Lisinopril clearance correlates with creatinine clearance, so as creatinine clearance decreases, lisinopril excretion also decreases. In patients with renal failure, the elimination of the drug is slowed down, and therefore dose adjustment is required. The drug has fairly variable bioavailability - from 26 to 60%. Food intake does not affect the bioavailability of the drug. Its action begins 1 hour after oral administration, the peak effect develops after 4–6 hours, and the duration of action reaches 24 hours, which provides a convenient administration regimen - once a day [4]. The severity of the inhibitory effect of lisinopril on ACE activity was studied in vitro on rabbit lungs. The affinity constant of ACE for lisinopril was comparable to that of enalaprilat and captopril, but the dissociation half-life of the drugs was 105, 27 and 9 minutes, respectively. These data indicate a greater affinity of lisinopril for ACE [5]. Unlike most other ACE inhibitors, lisinopril does not contain a sulfhydryl group, which is the cause of a number of side effects (neutropenia and proteinuria) [6]. Lisinopril is used to treat patients with hypertension, congestive heart failure, and after acute myocardial infarction (AMI) [7]. Moreover, it was recently approved in a number of countries (Great Britain, Spain, Belgium) for the treatment of diabetic nephropathy, and in Mexico, Portugal and New Zealand for the treatment of patients with diabetic retinopathy [8]. Efficacy of lisinopril in the treatment of hypertension In 2002, the results of the ALLHAT (Antihypertensive and Lipid–Lowering treatment to prevent Heart Attack Trial) study were published [9], which assessed mortality from coronary artery disease and the incidence of myocardial infarction in elderly patients. In the ALLHAT study, 15,255 patients received chlorthalidone at a dose of 12.5–25 mg, 9,048 patients received amlodipine at a dose of 2.5–10 mg, and 9,054 patients received lisinopril at a dose of 10–40 mg per day. If the target blood pressure level could not be achieved, then at the next stage a second drug was added (atenolol - 25-100 mg, reserpine - 0.05-0.2 mg once a day or clonidine - 0.1-0.3 mg twice a day day). If there was no effect, hydralazine was added at the third stage - 25-100 mg twice a day. None of the three drugs was shown to be superior in their ability to prevent the primary composite endpoint of myocardial infarction and cardiovascular mortality. The analysis of overall mortality also did not reveal any benefits of any drug. Lisinopril was slightly inferior to chlorthalidone in its ability to prevent strokes, hospitalization for angina, and worsening heart failure. However, lisinopril was significantly superior to amlodipine in preventing decompensated heart failure in whites; in black patients, the effectiveness of lisinopril and amlodipine did not differ significantly. A comparison of the effectiveness of two ACEIs, enalapril and lisinopril, was carried out using blood pressure monitoring to control the effectiveness of therapy. The target BP was set to 140/90 mm Hg, and the dose of both drugs was titrated to achieve this BP level. Hydrochlorothiazide was added if necessary. Both drugs significantly reduced blood pressure, but the effect of lisinopril was more pronounced. The average doses of drugs at the end of the study were 18 mg enalapril and 8 mg hydrochlorothiazide in one group, and 17 mg lisinopril and 6 mg hydrochlorothiazide in the second group. With the same administration regimen (once daily), lisinopril has a longer duration of action. The safety of the drugs was comparable [10]. A relatively small study (65 patients with DBP 95–115 mm Hg) compared the effectiveness and tolerability of lisinopril and the b-blocker nebivolol. Lisinopril was prescribed at a dose of 20 mg once daily, nebivolol - 5 mg once daily. Both drugs caused a significant decrease in blood pressure and were well tolerated by patients [11]. A Norwegian multicenter study examined the antihypertensive efficacy, tolerability, and impact of lisinopril (mean dose 18.8 mg) and nifedipine (mean dose 37.4 mg) on quality of life in 828 patients with mild to moderate hypertension. Lisinopril was more effective in lowering blood pressure and was better tolerated by patients. Both drugs had an equally good effect on the quality of life of patients [12]. A study comparing the effectiveness of lisinopril (20 mg) and the ARB telmisartan (80 mg) included 32 previously untreated patients with hypertension. The effectiveness of the drugs was the same both according to routine office blood pressure measurements and according to 24-hour blood pressure monitoring [13]. Lisinopril demonstrated comparable efficacy to the ARB valsartan. The large randomized trial PREVAIL (Ehe Blood Pressure Reduction and Tolerability of Valsartan in Comparison with Lisinopril study) included 1213 patients with grade 1–3 hypertension (SBP 160–220 mmHg and DBP 95–110 mmHg. ). Patients were randomized to receive valsartan 160 mg or lisinopril 20 mg per day. After four weeks, if there was insufficient effectiveness, hydrochlorothiazide was added to therapy. The total duration of treatment was 16 weeks. 1100 patients completed the full course of treatment; 51 patients in the valsartan group and 62 patients in the lisinopril group discontinued treatment due to side effects of therapy. The decrease in blood pressure was identical in both treatment groups – 31.2/15.9 mmHg. and 31.4/15.9 mmHg. respectively [14]. Lisinopril for obesity Two large studies - the NHS (non-smoking women) and the Seventh–Day Adventist Study (non-smoking, non-alcoholic vegetarian men) revealed a direct correlation between body mass index and cardiovascular mortality [15]. According to the Framingham study, every 4.5 kg of weight increases systolic blood pressure by 4.4 mmHg. in men and by 4.2 mm Hg. among women. The multicenter, double-blind, randomized, placebo-controlled study TROPHY conducted a comparative study of the effectiveness of 12-week treatment of 232 obese and hypertensive patients with lisinopril and hydrochlorothiazide (HCT). ABPM data showed that lisinopril and hydrochlorothiazide effectively reduced blood pressure throughout the day compared to placebo (p < 0.001). However, a decrease in DBP below 90 mm Hg. noted in 60% of patients treated with lisinopril and only in 43% of patients treated with hydrochlorothiazide (p<0.05). It is important that the majority of patients (57%) taking lisinopril remained on a dose of 10 mg throughout the treatment period, while the majority of patients receiving HCTZ (71%) required an increase in dose to 25–50 mg per day , which is associated with extremely adverse metabolic effects. Both drugs had no significant effect on insulin levels and lipid profiles, but plasma glucose levels at 12 weeks differed significantly (p<0.001) in the lisinopril (–0.21 mmol/L) and hydrochlorothiazide (+0.31 mmol/L) groups [16 ]. It must be recalled that lisinopril is the only hydrophilic ACE inhibitor with a duration of action of 24–30 hours that is not distributed in adipose tissue. These properties allow us to consider it a drug of choice in the treatment of obese patients with hypertension. Lisinopril and nephroprotection The nephroprotective effect of lisinopril has been demonstrated at various stages of diabetic nephropathy, regardless of the presence of hypertension. The multicenter 2-year placebo-controlled trial EUCLID (Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria) examined the early administration of lisinopril on the progression of diabetic nephropathy and retinopathy in 530 patients with type 2 diabetes (T2DM). ) without hypertension with normoalbuminuria (85% of patients) and microalbuminuria (15%). The level of microalbuminuria (MAU) in the lisinopril group at the end of observation was 18.8% lower than in the placebo group. The maximum effect was found in patients who already had nephropathy at the beginning of the study: in patients with initial normoalbuminuria, the decrease in urinary albumin excretion compared to placebo was 12.7% (1.0 mcg/min.), while in patients with initial normoalbuminuria MAU – 49.7% (34.2 mcg/min.). Thus, the EUCLID study demonstrated the ability of ACE inhibitors to slow down both the development and progression of the initial stage of diabetic nephropathy. At the same time, the greatest nephroprotective properties were manifested precisely at the MAU stage. The EUCLID trial also assessed the effect of lisinopril therapy on the development and progression of diabetic retinopathy (DR) [17]. In the lisinopril group, a 50% reduction in the risk of progression of DR was detected (OR=0.5) compared with placebo, while the maximum protective effect of ACE inhibitors on the development and progression of DR (OR=0.34) was observed in patients with compensation of carbohydrate metabolism - with HbA1c level less than 7%. In one of the largest studies using lisinopril in patients with type 2 diabetes, which included 3463 patients with initial and severe diabetic nephropathy (DN) and hypertension, the administration of lisinopril even for a short period (3 months) showed not only the high antihypertensive effectiveness of the drug, but also an improvement in nitrogen excretion function of the kidneys - in almost 50% of patients with initially elevated creatinine levels, this indicator stabilized. Studies also noted a positive effect of lisinopril on indicators of metabolic control (levels of glycated hemoglobin and blood lipids) and good tolerability of therapy - side effects developed in only 2.2% of patients [18]. Lisinopril and cardioprotection The 2-year ELVERA study (Effects of amlodipine and lisinopril on Left Ventricular mass) examined the effect of lisinopril and amlodipine on myocardial mass and left ventricular diastolic function in elderly patients with hypertension who did not receive antihypertensive therapy. The study included 166 patients with hypertension (DBP 95–115 mm Hg and SBP 160–220 mm Hg) aged 60 to 75 years: 81 patients received amlodipine at a dose of 2–10 mg per day, 85 patients received lisinopril at a dose of 10–20 mg per day. Myocardial mass index (MMI) decreased by 25.7 g/m2 in the amlodipine group and by 27 g/m2 in the lisinopril group. The SAMPLE study [19] included 206 patients with hypertension and LVH. During therapy with lisinopril at a dose of 20 mg/day. in combination with HCTZ (12.5–25 mg/day) and without it, an adequate reduction in blood pressure and a decrease in LV MMI by 15.8% were observed. The effectiveness of early use of lisinopril in acute myocardial infarction (AMI) has also been proven. The results of the GISSI-3 study showed that if treatment with lisinopril begins on the first day of AMI with stable hemodynamics, there is a significant reduction in overall mortality. Nitrates did not improve these indicators. Mortality rates and combined endpoints by month 6 were significantly lower (p=0.03) in the group of patients treated with lisinopril [20]. The SMILE-2 (Survival of Myocardial Infarction) study directly compared two ACE inhibitors for AMI: zofenopril at a dose of 30–60 mg and lisinopril at a dose of 5–10 mg per day. Both drugs were prescribed to patients who received thrombolytic therapy for AMI. ACE inhibitor therapy began no later than 12 hours after completion of thrombolysis and lasted 42 days. A total of 1024 patients were included in the study. There were no significant differences in the risk of cardiovascular complications in both treatment groups [20]. Lisinopril for CHF The randomized ATLAS study compared the effectiveness and tolerability of long-term therapy with low (2.5–5 mg) and high (32.5–35 mg) doses of lisinopril in 3164 patients with class II–IV CHF and an ejection fraction of no more than 30% . During observation, in the group of patients receiving high doses of lisinopril, there was a decrease in mortality from all causes by 8% and mortality from cardiovascular causes by 10%. In addition, therapy with high doses of lisinopril led to a significant reduction in the need for hospitalization due to decompensated CHF (by 24%) [22]. In addition, the ATLAS study established an extremely favorable economic effect when using high doses of the drug - the cost of treatment was $2 billion/year lower [23]. One of the most worthy representatives of lisinopril on the Russian market, completely satisfying the price-quality ratio, is lisinopril - Diroton. In Volgograd, under the guidance of prof. S.V. Nedogoda [24] conducted a 6-month open randomized study comparing the clinical and pharmacoeconomic effectiveness of lisinopril - Diroton (5 mg N 28) and Lizoril (10 mg N 30) in 40 patients with hypertension. It was proven that Diroton reduced both SBP and DBP to a slightly greater extent than Lizoril (p>0.05), but at the same time, the cost-effectiveness ratio of Diroton was 1.6 times better than that of Lizoril. Thus, lisinopril (Diroton) is an extremely effective and economical antihypertensive drug with organoprotective properties, which is convenient for doctors to work with in a wide variety of clinical situations. References 1. MRFIT research group. Multiple Risk Factor intervention Trial. Risk factor changes and mortality results. JAMA 1982;248:1465–77 2. The Task Force for the management of arterial hypertension of the European Society of Hypertension and of the European Society of Cardiology. 2007 Guidelines for the management of arterial hypertension. J Hypertens 2007; 25:1105–1187. 3. VNOK. Prevention, diagnosis and treatment of arterial hypertension. Russian recommendations (second revision). Cardiovascular Therapy and Prevention 2004. Appendix 4. 4. Semple PF et al. Onset of action of captopril, enalapril, enalaprilic acid and lisinopril in normal man // Cardiovascular Drugs and Therapy. – 1987– Vol. 1. – P. 45–50. 5. Bull HG Inhibition of rabbit lung ACE by lisinopril, enalapril and captopril. // J. of Biological Chem. –1985–Vol.260 – P.2952–2962. 6. Chodoff L. Lisinopril: a new ACE inhibitor for the treatment of hypertension and congestive heart failure // Mt. Sinai. J. Med. – 1990. – Vol. 57. – P. 169–171. 7. Lisinopril. Mosby's GenRx – The complete reference for generic and brand drugs. 9th edn., Mosby, Inc., St. Louis, Missouri, 1999. 8. AstraZeneca. 'Zestril' prescribing information. . Available from: https://www.zestrilinfo.com/info/info.htm. 9. Davis BR, Culter JA, Gordon DJ Antihypertensive and lipid–lowering treatment to prevent heart attack trial. Am. J. Hypertens. – 1996. –Vol.9. –P.342–60. 10. Diamant M, Vincent HH Lisinopril versus enalapril: evaluation of through: peak ratio by ambulatory blood pressure monitoring. J Hum Hypertens. – 1999/ – Jun;13(6):405–12. 11. Rosei EA, Rizzoni D, Comini S et al. Evaluation of the efficacy and tolerability of nebivolol versus lisinopril in the treatment of essential arterial hypertension: a randomized, multicentre, double-blind study. Blood Press Suppl. – 2003, May;1:30–5 12. Os I, Bratland B, Dahlof B at al. Lisinopril or nifedipine in essential hypertension? A Norwegian multicenter study on efficacy, tolerability and quality of life in 828 patients. J Hypertens. – 1992, Feb;10(2). 13. Stergiou GS, Efstathiou SP, Roussias LG et. Al. Blood pressure– and pulse pressure–lowering effects, through:peak ratio and smoothness index of telmisartan compared with lisinopril. J Cardiovasc Pharmacol. – 2003, Oct;42(4):491–6. 14. Malacco E, Santonastaso M, Vari NA et al. Comparison of valsartan 160 mg with lisinopril 20 mg, given as monotherapy or in combination with a diuretic, for the treatment of hypertension: the Blood Pressure Reduction and Tolerability of Valsartan in Comparison with Lisinopril (PREVAIL) study. Clin Ther. – 2004. – Jun;26(6):855–65. 15. Lindsted K. Study Seventh–Day Adventist. Int J Obesity, 1991. 16. Reisin E et al. Lisinopril versus HCTZ in obese hypertensive patients: a multicenter placebo–controlled trial. Treatment in obese Patients with Hypertension (TROPHY) Study Group. Hypert 1997: Jul 30: 140–145 17. Euclid Study Group. Effect of Lisinopril On ProgReSSion of Retinopathy in Normotensive Peopler with Type 1 Diabetes. Lancet 1998; 351: 28–31. 18. Parting hh. Effects of Ace Inhibitors On Renal Function InCipient and Overtic Nephropathy. // J Diabetes Complications. 1996; 10 (3): 133–135. 19. Mancia G., Zanchetti A. et al. Study on Monitoring of Blood Pressure and Lisinopril EvalUation. Circulation, 1997; 95 (6); 1464–70. 20. Latini R., Nicolosi G., Maggioni Ap. et al. The Beneficial Effect of Lisinopril on Left Ventricular Remodeling After a First Myocardial IS Modulated by Age. The Gissi -3 Echo Database (abstract) no. 775–11. .1 Am Coll Cardiol 1996; 27 (2) SUPPL. A: 281 A 21. Ambrossioni E., Borgii S., Magnani V. et al. The Effect of the Angiotensin - Convertmg - Enzmie Inhibitor Zofenopril On Mortaly and Morbidity Anterior MyCardial Infarction. New Engi J Med. 1995; 332: 2: 80–85. 22. Packer M., Poole - Wilson P., Armstrong P. et al. Comparative Effects of Low - Dose Versus High - Dose Lisinopril on Survival and Major Events in Chronic Heart Failure: The Assessement OF TREATMENTH LISINOPRI ). Europ. Heart J., 1998; 19 (SUPPL.): 142 (abstract). 23. Packer m et al. Comparative Effects of Low and High Doses of the Acei Lisinopril, On Morbidity and Mortaly in Chronic Heart Failure. Circulation 1999; 100: 1–7. 24. Ostroumova O.D., Nedogoda S.V., Mamaev V.I., Shorikova E.G., pharmacoeconomic aspects of the effectiveness of angiotensic enzyme inhibitors in arterial hypertension and heart failure, rmzh volume 11, No. 5, p. 262– 267
Lisinopril or Captopril – which is better?
Manufacturer: Pharmakor, Ozone, Biosynthesis, Pranapharm, Russia
Release form: tablets
Active ingredient: Captopril
Synonyms: Capoten, Angiopril, Captopril Sandoz, Captopril-AKOS
Captopril belongs to the very first generation of ACE inhibitors. The drug is quickly absorbed into the bloodstream, the effect occurs within 30 minutes after administration, therefore it is often used as an ambulance for hypertensive crises.
Captopril can be considered the cheapest Russian analogue of Lisinopril.
Clinical and pharmacological properties of lisinopril
A feature of the chemical structure of lisinopril is the presence of a carboxyl group, which binds to the zinc-containing domain of the angiotensin-converting enzyme (ACE). Unlike most other ACE inhibitors, lisinopril is not a prodrug. Absorbed into the gastrointestinal tract, it does not undergo further metabolic transformations and is excreted unchanged by the kidneys. The bioavailability of the drug is quite variable - on average 30%. Lisinopril is not lipophilic and practically does not bind to plasma proteins.
An important feature of lisinopril is its long-lasting action. The effect appears within an hour after oral administration, the peak of action develops after 4–6 hours, and the duration reaches 24 hours, which provides a convenient administration regimen - once a day.
The drug has been shown to be safe and does not require dose adjustment when creatinine clearance is more than 30 ml/min. When creatinine clearance is less than 30 ml/min, it is necessary to start therapy with low doses (2.5–5 mg/day) and monitor potassium and creatinine levels in the blood.
In the treatment of arterial hypertension (AH), the initial dose of the drug is 5–10 mg/day, later it is increased to 40 mg/day. It was found that when the dose was increased to 80 mg/day, there was no additional reduction in blood pressure. To enhance the hypotensive effect, combination therapy with thiazide diuretics is indicated.
For heart failure, treatment with lisinopril is recommended to begin with a dose of 2.5–5 mg/day, followed by titration to 40 mg/day when systolic blood pressure (SBP) is above 100 mm Hg. Art.
In acute myocardial infarction, early administration of lisinopril (in the first 24–48 hours) to hemodynamically stable patients is possible. The initial dose is 5–10 mg.
In patients with diabetic nephropathy, the initial dose of the drug is 10 mg/day with further adjustment to 20 mg/day.
The most common side effect of lisinopril is a dry cough. A large post-marketing study of 10,289 patients showed that, in addition to dry cough, the most common adverse reactions were dizziness (2.3%), headache (2.1%), weakness (1.7%) and nausea (1.0%). ) [1]. The frequency of these adverse events is not high and does not exceed that when using placebo.
A large population-based observational study found that lisinopril did not significantly affect blood creatinine levels. Among 18,977 patients receiving lisinopril for 6 months, an increase in creatinine to 2.5 mg/dL or higher was observed in only 31 patients. A significant increase in creatinine levels was usually associated with severe heart failure, dehydration, or the presence of concomitant diseases [2].
In recent years, a number of generics of lisinopril have appeared on the market, comparable in pharmacokinetics to the original drug. One of them is Lysigamma (Wörwag Pharma, Germany). The drug is available in dosages of 5, 10 and 20 mg, which ensures ease of administration to patients with various pathologies, and is registered for use in all four main indications.
Lisinopril for hypertension
Lisinopril has been used for many years to treat hypertension, and to date, a lot of data have accumulated confirming its good effectiveness.
When treating hypertension, a single dose per day significantly increases patient adherence to therapy. The effectiveness of this dosing regimen has been proven using 24-hour blood pressure monitoring. The drug in a dose of 20 mg was prescribed to the first group of patients at 8.00, the second - at 16.00 and the third - at 22.00. The degree of blood pressure reduction and the duration of the hypotensive effect were similar in all three treatment groups. When the drug was prescribed at 10 p.m., the morning rise in blood pressure, associated with the highest risk of cardiovascular complications, was prevented to the greatest extent. Apparently, this drug prescription regimen is preferable [3].
A number of studies have shown that lisinopril is comparable in antihypertensive effectiveness to other ACE inhibitors. Thus, when directly comparing the effectiveness of combinations of enalapril and lisinopril with the diuretic hydrochlorothiazide (HCTZ) by monitoring blood pressure, it turned out that 18 mg of enalapril + 8 mg of HCTZ and 17 mg of lisinopril + 6 mg of HCTZ have equivalent hypotensive activity [4]. A randomized study in 181 patients with hypertension revealed that the hypotensive activity of lisinopril at a dose of 10 mg/day and zofenopril at a dose of 30 mg/day was the same [5]. Thus, in the treatment of arterial hypertension, target doses of ACE inhibitors may be 50 mg 3 times a day for captopril, 20 mg per day for enalapril, 40 mg per day for lisinopril and fosinopril [6].
The antihypertensive effectiveness of lisinopril is also comparable to the effectiveness of drugs from other groups. Thus, it turned out that the degree of hypotensive effect of lisinopril at a dose of 20 mg/day does not differ from the beta-blocker nebivolol at a dose of 5 mg/day [7].
Lisinopril is not inferior in effectiveness to calcium antagonists. A Danish pooled study compared the effectiveness and tolerability of lisinopril 10–20 mg/day and felodipine 5–10 mg/day in patients with stage I–II hypertension. Lisinopril was better tolerated by patients, and the incidence of side effects with its use was lower [8].
A Norwegian multicenter study assessed the antihypertensive efficacy, tolerability, and impact of lisinopril and nifedipine on the quality of life of 828 patients with stage I–II hypertension. The average dose of lisinopril at the end of the study was 18.8 mg/day, nifedipine - 37.4 mg/day. Lisinopril was more effective in reducing systolic blood pressure (SBP) and diastolic blood pressure (DBP), and was less likely to cause side effects. Both drugs had the same effect on the quality of life of patients [9].
The TROPHY study compared the antihypertensive efficacy of lisinopril and HCTZ using 24-hour blood pressure monitoring. The study included 124 patients with hypertension and obesity. Lisinopril was prescribed at a dose of 10–40 mg/day, HCTZ – 12.5–50 mg/day. The duration of treatment was 12 weeks. Both drugs significantly reduced blood pressure, and the degree of reduction in SBP was the same, and DBP decreased more in the lisinopril group. In men, lisinopril was generally more effective than HCTZ; in women, the effectiveness of both drugs was equal. In patients of the Negroid race, a diuretic was more effective, in Caucasians - an ACE inhibitor. When dividing patients into groups according to the type of circadian rhythm of blood pressure, it turned out that non-dippers (patients with a degree of nocturnal decrease in blood pressure
Several studies have compared the effectiveness of lisinopril and angiotensin receptor blockers (ARBs). Telmisartan 80 mg/day and lisinopril 20 mg/day had the same effect [11]. The effectiveness of lisinopril and losartan also turned out to be comparable [12]. In patients with severe hypertension, the combination of 8 mg of candesartan and 12.5 mg of HCTZ per day was equivalent in effectiveness to the combination of 10 mg of lisinopril and 12.5 mg of HCTZ [13].
The large study PREVAIL (The Blood Pressure Reduction and Tolerance of Valsartan in Comparison with Lisinopril study) included 1213 patients with stage I–III hypertension. (SBP – 160–220 mm Hg, DBP – 95–110 mm Hg). Patients were randomized to receive valsartan 160 mg/day or lisinopril 20 mg/day. If necessary, HCTZ was added to therapy. The total duration of treatment was 16 weeks. The decrease in blood pressure was identical in both treatment groups – 31.2/15.9 mm Hg. Art. and 31.4/15.9 mm Hg. Art. respectively [14].
Combination therapy with valsartan and amlodipine was comparable in effectiveness to the combination of lisinopril + HCTZ. The double-blind randomized study included 130 patients with stage II hypertension. Patients received valsartan 160 mg/day and amlodipine 5–10 mg/day or lisinopril 10–20 mg/day and HCTZ 12.5 mg/day. It turned out that both combinations are equivalent in reducing blood pressure and are equally well tolerated [15].
Effect on the condition of target organs
One of the important requirements for modern antihypertensive drugs is their protective effect against damage to the main target organs in hypertension, primarily the development of left ventricular (LV) myocardial hypertrophy and nephropathy. In addition, the effect of antihypertensive therapy on the elasticity of the arteries and the function of the vascular endothelium is significant - factors directly related to the activity of atherosclerotic lesions and the risk of developing cardiovascular complications. Sufficient evidence has accumulated regarding the protective effect of lisinopril on target organs. Lisinopril prevents the development of left ventricular myocardial hypertrophy and causes a decrease in its mass during long-term treatment. In the SAMPLE study (Study on Ambulatory Monitoring of Blood Pressure and Lisinopril Evaluation), patients received lisinopril at a dose of 20 mg/day for a year, if necessary in combination with HCTZ at a dose of 12.5–25 mg/day. Lisinopril not only significantly reduced blood pressure (according to office measurements and 24-hour monitoring), but also caused a reverse development of LV myocardial hypertrophy [16].
In the ELVERA study (Effects of amlodipine and lisinopril on Left Ventricular mass), in 85 patients receiving lisinopril at a dose of 10–20 mg/day for 2 years, the myocardial mass index decreased by 25.7 g/m2 [17].
Left atrial volume is a risk factor for a number of serious complications, the most common of which is atrial fibrillation. It has been shown that therapy with lisinopril helps to reduce the volume of the left atrium and reduce the fraction of mitral regurgitation even in patients with organic damage to the heart valves [18].
In another study of similar design, 69 patients with hypertension who had not previously received antihypertensive treatment took amlodipine at a dose of 5–10 mg/day or lisinopril at a dose of 5–20 mg/day for 12 months. Both groups showed the same regression of intima-media thickness of the carotid arteries. At the same time, the lumen of the common carotid arteries at the end of treatment turned out to be significantly larger in the lisinopril group, which, apparently, may be associated with favorable structural changes in the wall of the carotid arteries during treatment with ACE inhibitors [19].
Improvement in endothelial regulation of vascular tone during lisinopril therapy has been shown in small studies in smokers and patients with dyslipidemia [20, 21].
ALLHAT Study
The largest clinical trial of lisinopril in patients with hypertension was the ALLHAT trial, the results of which have been discussed in detail previously [22, 23].
In this study, 15,255 patients received the diuretic chlorthalidone at a dose of 12.5–25 mg/day, 9048 patients received amlodipine at a dose of 2.5–10 mg/day, and 9054 patients received lisinopril at a dose of 10–40 mg/day. According to the ability to prevent the onset of the so-called. primary composite endpoint (myocardial infarction + death from cardiovascular causes) and reducing overall mortality, no benefits were identified for any of the drugs used. Lisinopril was slightly inferior to chlorthalidone in its ability to prevent strokes, hospitalization for angina, and worsening heart failure. This may have been due to its slightly weaker hypotensive effect compared to chlorthalidone. The differences were especially pronounced in people of the Negroid race, who are characterized by low sensitivity to ACE inhibitors. At the same time, treatment of hypertension with lisinopril in Caucasian patients was more successful. Thus, it had significant superiority over amlodipine in the prevention of decompensated heart failure in whites. In patients of the Negroid race, lisinopril and amlodipine did not differ significantly in effectiveness.
The most interesting results of the study include data on a reduced risk of developing new cases of diabetes mellitus (DM) in patients receiving lisinopril compared with those taking chlorthalidone [24]. The incidence of new cases of diabetes diagnosed 2 years after the start of treatment was almost 2 times higher in the chlorthalidone group than in the lisinopril group. The same trend continued after 4 years. Patients taking lisinopril had lower blood glucose levels. These differences became significant after 2 years of the study and remained statistically significant until its end.
Most often, this effect is associated with blockade of the renin-angiotensin system, but the mechanism of the effect of ACE inhibitors and BAR on the prevention of the development of insulin resistance is not completely clear.
The ALLHAT study conducted a genetic substudy, GenHAT, to determine whether genetic markers influence the effectiveness of antihypertensive therapy. The first results of the GenHAT study have already been published. The main genes presumably determining the effectiveness of lisinopril were the angiotensin-converting enzyme (ACE) gene and its polymorphic marker type I/D. It was previously shown that carriers of the D allele have a higher level of expression of the ACE gene and higher activity of the renin-angiotensin system. Carriage of the D allele is believed to predispose to the development of cardiovascular complications. In the GenHat study, no association of this allele with the effectiveness of lisinopril therapy was found [24].
Other indications for lisinopril
Diabetes and diabetic nephropathy
In patients with diabetes, therapy with ACE inhibitors helps not only to slow down the progression of target organ damage, primarily nephropathy, but also to increase tissue sensitivity to insulin. Evidence has been obtained of the effectiveness of lisinopril in this group of patients.
The multicenter study EUCLID (Randomized placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria) studied the effect of lisinopril on the progression of diabetic nephropathy and retinopathy in patients with type 2 diabetes without hypertension. Therapy continued for 2 years. At the end of the study, the level of microalbuminuria in the lisinopril group was 18.8% lower than in the placebo group. The maximum effect was observed in patients who already had nephropathy at the beginning of the study. In patients receiving lisinopril, the level of glycosylated hemoglobin was significantly lower (6.9 compared to 7.3%). Progression of retinopathy was observed in 13.2% of patients in the lisinopril group and in 24.3% in the placebo group [25].
The purpose of the CALM study (The candesartan and lisinopril microalbuminuria study) was to compare the effectiveness of monotherapy with candesartan, lisinopril and combination therapy with these two drugs in 199 patients with hypertension, microalbuminuria and T2DM. The main criteria for inclusion in the study were DBP 90–110 mmHg. Art. and creatinine/albumin ratio 2.5–25 mg/mmol after 2 weeks of placebo. The main parameters by which the effectiveness of therapy was assessed were blood pressure level and the degree of microalbuminuria. Patients received lisinopril 20 mg/day or candesartan 16 mg/day for 12 weeks. At the end of this period, the reduction in blood pressure was similar in both groups. When lisinopril was prescribed, there was a tendency toward a greater reduction in urinary albumin excretion. Next, a third of patients continued monotherapy with lisinopril, a third continued monotherapy with candesartan, and another third received combination therapy with these drugs for 12 weeks. In terms of its effect on blood pressure levels, combination therapy was more effective than monotherapy with any of the drugs. The regression of microalbuminuria in the combination therapy group was also the most significant - by 50%. However, in this case, combination therapy was significantly more effective only compared to candesartan (p = 0.04). When compared with lisinopril monotherapy, no significant differences in the effect on microalbuminuria were found [26].
The results of these and other similar studies allow us to recommend lisinopril for use in patients with diabetic nephropathy.
Acute myocardial infarction
Lisinopril was one of the first ACE inhibitors to be proven effective in acute myocardial infarction (MI). The GISSI-3 study (Gruppo Italiano per lo Studio della Sopravvivenzanell'Infarto miocardico) was devoted to studying the effectiveness of lisinopril, nitrates and their combination in patients with acute MI. The study included 19,394 patients. Therapy with nitrates or lisinopril began no later than 24 hours from the onset of MI symptoms. The dose of lisinopril was 5 mg/day. It turned out that only in the group of patients receiving lisinopril, by the 6th week of therapy there was a significant reduction in mortality - by 7.7%, and in the primary combined end point (death + left ventricular systolic dysfunction) - by 11%. Differences in the risk of adverse outcomes persisted 6 months after MI. In addition to the fact that in the lisinopril group the risk of developing severe LV dysfunction decreased, its remodeling decreased [27]. The effect of lisinopril on the prognosis of MI was especially significant among patients with diabetes [28]. It is important to emphasize that the administration of lisinopril is indicated for hemodynamically stable patients. In the group of patients who had SBP below 120 mmHg at the time of randomization. Art., the incidence of severe hypotension and the risk of adverse outcomes with lisinopril were higher than in the placebo group [29].
The SMILE-2 (Survival of Myocardial Infarction) study directly compared the effectiveness of two ACE inhibitors in acute myocardial infarction: zofenopril at a dose of 30–60 mg and lisinopril at a dose of 5–10 mg per day. Both drugs were prescribed to patients receiving thrombolytic therapy. Treatment with ACE inhibitors began no later than 12 hours after completion of thrombolysis and lasted 42 days. A total of 1024 patients were included in the study. There were no significant differences in the risk of cardiovascular complications in both treatment groups [30].
Chronic heart failure
The ATLAS (Assessment of Treatment with Lisinopril And Survival) study compared the effectiveness of high (32.5–35 mg/day) and low (2.5–5 mg/day) doses of lisinopril in the treatment of heart failure. A total of 3164 patients with FC II–IV CHF (NYHA) who had an ejection fraction of less than 30% participated in the study. The greatest reduction in the risk of new hospitalizations due to worsening heart failure was 24% in the group of patients receiving high doses of the drug [31, 32]. In addition, in this group there was a tendency to reduce overall mortality - by 8%, not significant - and mortality from cardiovascular causes - by 10%, not significant, and the risk of overall mortality and all cases of hospitalization significantly decreased - by 12%, p = 0.002. The effect of high doses of lisinopril was the best in patients with high FC of heart failure. The use of high doses of lisinopril was also more preferable from a pharmacoeconomic point of view [33].
Thus, lisinopril is one of the most well-known and well-studied drugs in the group of ACE inhibitors. A large evidence base serves as the basis for the widespread use of lisinopril in cardiological practice.
Lisinopril or Amlodipine
Manufacturer: Berezovsky pharmaceutical plant, Rozlex, ALSI-pharma, Russia
Release form: film-coated tablets
Active ingredient: Amlodipine
Synonyms: Norvasc, Tenox, Normodipin, Amlotop, Kalchek, Amlorus, Cordi Cor
The analogue Amlodipine reduces blood pressure by another mechanism: the drug is a calcium channel blocker, that is, it reduces the tone of the smooth muscles of the vascular walls.
In addition to the hypotensive effect, Amlodipine increases the supply of oxygen to the myocardium, therefore it is also successfully used as an antianginal agent for angina pectoris.
Lisinopril or Prestarium - which is better?
Manufacturer: Servier, France
Release form: film-coated tablets dispersible in the oral cavity
Active ingredient: Perindopril
Synonyms: Prestarium, Perineva, Coverex, Parnavel, Perindopril-Vertex, Perindopril-Teva
Prestarium is an ACE inhibitor and additionally reduces heart rate, reduces myocardial oxygen demand, restores vascular elasticity, and has a moderate diuretic effect.
Prescribed for coronary heart disease and for the prevention of complications after strokes.
Characteristics of Lozap
Lozap is an antihypertensive drug based on losartan potassium. Available in coated tablets consisting of excipients. Due to the active component, the following pharmacological actions are formed:
- relaxation, elimination of vascular spasm;
- decrease in angiotensin, aldrosterone;
- no effect on ACE.
Absorption occurs through the intestines. Bioavailability is low. There is no penetration through the blood-brain barrier. Metabolism occurs in the circulatory system. Excretion occurs through the kidneys. Indications for use:
- arterial hypertension:
- heart failure;
- diabetic nephropathy.
The medicine is contraindicated in case of individual intolerance, severe liver damage, and minors. It should not be drunk during pregnancy or lactation; the active substance penetrates the placental barrier. It is not recommended to combine ACE inhibitors and Lozap.
Side effects
Despite its high effectiveness, the product has many side effects. Allergic reactions develop more often at the local and systemic level. But there are other negative consequences:
- reduction of blood sprouts;
- headache, migraine, depression;
- tinnitus, increased heart rate, arrhythmia, excessive hypotension;
- cough, shortness of breath;
- dyspeptic reactions, nausea, inflammation of the pancreas and liver;
- inflammation of muscles, joints;
- kidney inflammation, kidney failure;
- impotence;
- weakness, swelling, malaise
There are diseases and conditions for which the drug is compatible, but is used with caution. These include heart failure, arrhythmia, low-grade cardiomyopathy, liver or kidney failure. The product can also be used after 75 years. For all these conditions, it is recommended to periodically undergo examinations, take laboratory tests of blood and urine.
Enap or Lisinopril – which is better?
Manufacturer: KRKA, Slovenia
Release form: film-coated tablets
Active ingredient: Enalapril
Synonyms: Renipril, Enam, Berlipril, Renitek, Enalapril-ACRI
The Enap analogue is a first generation ACE inhibitor. Reduces blood pressure and is used for hypertension and other cardiovascular diseases.
Enap N contains a diuretic component that enhances the effect of the main active ingredient.
Characteristics of Lisinopril
Lisinopril is an antihypertensive drug based on the active substance of the same name. Manufactured by Vertex. The composition includes auxiliary components that are taken into account by doctors when selecting the dosage of the drug for allergy sufferers or patients. Due to the active component, the following pharmacodynamic properties are formed:
- decrease in angiotensin, aldosterone, bradykinin, increase in prostaglandins, due to which blood pressure decreases;
- reducing the load on blood vessels;
- dilatation of arteries, to a lesser extent veins;
- reduction of the myocardium of a hypertrophied heart;
- increasing life expectancy by eliminating the negative effect on the cardiovascular system.
The drug is absorbed in the intestines, bioavailability is low. A small amount of the substance penetrates the blood-brain barrier. Metabolism practically does not occur. Excretion is carried out by the kidneys. The medicine is indicated for use in the following diseases:
- arterial hypertension;
- heart failure, history of myocardial infarction;
- diabetic nephropathy.
The product is not used in cases of hypersensitivity or systemic allergic reactions. It is not recommended for use during pregnancy or lactation in women, as the substance penetrates the placenta. There have not been enough clinical trials on minors, so the drug is not prescribed for them.
Side effects
The drug affects many organs and systems. More often, negative reactions develop due to irrational use or self-medication. The following side effects are possible:
- excessive hypotension, cardiac arrhythmia, myocardial infarction;
- numbness of the limbs, confusion, fatigue;
- decrease in the number of blood cells;
- cough, bronchospasm;
- dyspeptic reactions, changes in taste, inflammation of the pancreas and liver, jaundice;
- local, systemic allergy;
- inflammation of joints, muscles, blood vessels.
There are categories of patients for whom the drug can be used, but with caution. These include patients with a hypertrophied heart, hyperaldosteronism, chronic heart failure, diabetes mellitus, and autoimmune diseases. During therapy, it is recommended to take repeated laboratory tests of blood and urine. If you feel worse, the medicine should be discontinued immediately.
Indapamide or Lisinopril - which is better?
Manufacturer: ALSI-pharma, Ozon, Biokhimik, Russia
Release form: film-coated tablets
Active ingredient: Indapamide
Synonyms: Indap, Arifon, Arifon Retard, Ravel SR, Indapamide Retard
The analogue Indapamide is a diuretic, due to its diuretic effect and lowers blood pressure.
Indapamide is an analogue of Lisinopril without the side effects characteristic of ACE inhibitors.
Before replacing Lisinopril for blood pressure, you should definitely consult a doctor who will help you find a replacement for Lisinopril, taking into account the whole picture of the patient’s disease.
Efficiency of selection of analogues
The effect of the analogue depends on the health status of the man or woman. A preliminary examination using laboratory and instrumental tests is required. The following indicators in the body are taken into account:
- degree of arterial hypertension;
- presence of extraneous cardiovascular disorders;
- age, presence or absence of pregnancy, lactation;
- condition of internal organs (liver, kidneys, gastrointestinal tract, pancreas).
Medicines that do not inhibit ACE are considered more gentle. However, they have less effect on the body. If arterial hypertension is moderate to severe, it is recommended to choose drugs based on losartan or other substances with an effect on ACE.
If a person independently selects a replacement, a strong effect on the cardiovascular system with complications is possible.
Unforeseen consequences may occur, leading to myocardial hypertrophy, increased load on the left ventricle, and hypotension. Even if a cardiologist helped change the medicine, it is recommended to take laboratory blood tests, undergo an ECG, and an ultrasound of the heart every 6 months. This will prevent the lack of therapeutic effect and adverse reactions.