Varicose veins of the esophagus: features of pathology
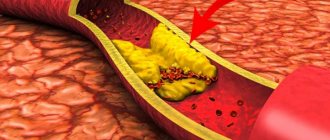
Varicose veins of the esophagus are a rather dangerous pathology. It represents a deformation of blood vessels. As a result of the development of the disease, the lumen of the veins increases, their walls stand out and nodes form. Deformed vessels become very tortuous and quite loose. The mucous membrane, which is located above the vessels, is subject to damage and inflammation.
The disease is also dangerous due to the absence of symptoms at an early stage of development. In the initial stages, varicose veins do not show any signs. For this reason, a person has no idea that pathological processes are occurring in his body. Meanwhile, varicose veins are very dangerous!
With the development of varicose veins, the patient complains of:
- belching and heartburn,
- from time to time difficulties when swallowing food (gradually discomfort becomes a constant companion),
- increased heart rate,
- discomfort and heaviness in the chest area.
Esophagitis is often associated with varicose veins of the esophagus. This process is inflammatory.
Bleeding becomes a dangerous complication of this pathology. The result is weakness and shortness of breath. General health deteriorates. The patient may suffer from weight loss.
Request a call back Get a free consultation
Current classification
There are several proposed classifications of the disease. Signs are detected during esophagogastroscopic examination. The most acceptable division of esophageal varicose veins according to the degree of change in the veins is considered.
- 1st degree - the maximum diameter of the vessels is 5 mm, they are elongated, localized in the lower part of the esophagus;
- 2nd degree - the tortuosity of the veins is determined, the diameter is increased to 1 cm, reaching the middle third of the organ;
- 3rd degree - draws attention to the thinning and tension of the walls of venous vessels, diameter over 10 mm, they are side by side, on the surface there are characteristic red markers from the smallest capillaries.
The initial stage is characterized by the absence of vein tortuosity
According to another classification (Vytenasoma and Tamulevichute), it is proposed to take into account 4 stages of the disease:
- 1 - vein diameter is allowed 2–3 mm, they are bluish in color and straight in shape;
- 2 - veins become tortuous, nodular, and increase in diameter to more than 3 mm;
- 3 - varicose nodes are clearly visible, significant tortuosity, protrusion appears into the lumen of the esophagus;
- 4 - the nodes grow to a grape-shaped shape, significantly narrow the lumen of the esophagus, and a thin network of small capillaries is visible on the outer surface.
In addition, the diagnosis takes into account:
- congenital form occurring against the background of pathologies of unknown origin;
- acquired - caused by various diseases.
How is the disease diagnosed?
Esophageal varicose veins are diagnosed by:
- Studying anamnesis.
- Medical examination. During it, you can note such signs of varicose veins as swelling, changes in the color of the skin and mucous membranes.
- Laboratory research. To study varicose pathology, the patient undergoes general and biochemical blood tests. Specialists count the number of platelets, examine liver enzymes, serum iron, protein, and lipid spectrum.
- Instrumental research. If varicose veins of the esophagus are suspected, ultrasound, esophagoscopy and x-ray diagnostics are performed. These studies are aimed at studying a specific area of the esophagus. The remaining organs of the peritoneum are also studied.
Prognosis for liver cirrhosis
Vascular disease of the gastrointestinal tract is characterized by high mortality. In cirrhosis it reaches 50%. Mortality does not depend on the nature of the bleeding, but on the severity of organ damage.
In 80% of cases, hemorrhage occurs on its own, so the likelihood of recovery is in those patients who have good liver condition. But 75% of patients are susceptible to relapse within the first two years.
To improve the condition of varicose veins, it is necessary to regularly undergo drug support and endoscopic treatment.
Although VRVP cannot be treated, the patient can live for decades if he maintains his condition with timely examinations, adjusts his diet and sleep and rest patterns. Be healthy!
How is esophageal varicose veins treated?
The main goal of therapy for esophageal varices is to prevent bleeding. In some cases, specialists have to eliminate the consequences of bleeding that has already been suffered.
Vein enlargement is treated by prescribing:
- Vitamins, antacids and astringents.
- Hemostatic agents.
- Drugs that constrict blood vessels.
In some cases, special colloidal solutions are introduced. Transfusions of plasma, blood and red blood cells are also carried out.
Surgeries on the esophagus are resorted to when drug therapy does not give the desired result.
All interventions are divided into 2 groups:
- Endoscopic.
- Surgical.
Endoscopic interventions on the esophagus are carried out by:
- Electrocoagulation. With this intervention, damaged vein tissue is effectively removed under the influence of electric current.
- Doping of the esophageal veins. This technique boils down to careful ligation of the veins of the esophagus. To carry out the intervention, specialists use small rings. 1, 2 or 3 rings are placed on each vein. Alloying is also possible using nylon loops.
- Bandaging. This technique is used to fix dilated veins. Thanks to this, you can quickly stop bleeding that has already begun due to vasodilation.
- Insertion of a probe that compresses the veins. Vein probes are made of rubber. They apply pressure to the bleeding vessel.
- Application of a special adhesive film or a substance such as thrombin to the affected areas of the veins.
Surgical operations to prevent bleeding as a result of dilation of the veins of the esophagus are carried out by:
- Sclerosis. A special solution is injected into the dilated veins. The solution is supplied by injection. They are injected into the lumen of the veins of the esophagus. The technique is quite effective. There is one significant drawback. The procedure must be carried out constantly and regularly. Typically, sclerotherapy is repeated every 5 days. Then the procedure is carried out once a month. Subsequently, sclerotherapy is carried out once every 3 months. At least 4-5 procedures must be performed per year. Only in this case can the method be sufficiently effective.
- Portosystemic stent shunting. This technique for eliminating varicose pathologies involves introducing a special stent into the middle part of the liver. It connects the functionality of the hepatic and portal veins.
- Anostomosis. The objects of intervention are the splenic vein and the left kidney.
- Vessel lining.
- Removal of esophageal veins that cannot be restored.
All operations on the veins of the esophagus are quite dangerous. In addition, varicose pathologies cannot be completely eliminated with their help. Relapses often occur, and operations provoke the risk of a number of complications.
That is why varicose pathologies are now being fought using another method. It is innovative and allows you to forget about the problem!
Embolization for dilated veins is popular for good reason!
Request a call back Get a free consultation
CLINICAL DIAGNOSIS OF PORTAL HYPERTENSION
With physical examination, it is easiest to detect ascites, redness, spider-like angiomas on the skin, erythema pubis, testicular atrophy, gynecomastia, Dupuytren's contracture and muscle atrophy. Portosystemic encephalopathy may also manifest itself - in some cases, asterixis (blurring or “purrying” tremor of the hands) and lethargy, in the lungs - restlessness, sleep disturbance. Most patients with PG also exhibit splenomegaly, although the size of the spleen correlates poorly with portal venous pressure and its increase may be associated with other illnesses. A hyperdynamic state can be indicated by a high (jumping) pulse, warm, well-perfused endings in conjunction with arterial hypotension.
Signs of portosystemic collaterals are dilated veins on the anterior surface of the abdomen (umbilical-epigastric shunts), the “jellyfish head” becomes a sinuous colateral vein near the navel. Internal hemorrhoids are not a specific finding, but may also manifest collateralization. The weakness of the visible collateral vessels on the back does not indicate portal hypertension, but obstruction in the level of the inferior venous vein. A rare cause may be compression of the lower empty vein by regenerative nodes in liver cirrhosis.
Ascites is easy to detect when there is a lot of swelling in the stomach - in such cases the life is tight, and swelling of the spine can be detected. However, minor ascites can be diagnosed instrumentally, for example, with the help of ultrasonography. Paracentesis helps to establish the etiology of ascites: the portal (non-peritoneal) etiology indicates a serum ascitic albumin gradient (SAAG) of over 1.1 g/dL (11 g/L). However, this method cannot distinguish between hepatic and suprahepatic PH, for example, in cases of persistent heart failure. Recent studies indicate a decrease in SAAG following the placement of transjugular portosystemic shunts (TIPS).
Laboratory testing of gas is not specific for the detection of PG. Indicates an increase in prothrombin hour and thrombocytopenia. In patients with cirrhosis of the liver, these indicators are considered predictors of the presence of varicose veins (see below). Hypoalbuminemia indicates the importance of liver function and, indirectly, PG. Similarly, hyponatremia and low sodium concentrations in the tissue may contribute to water and sodium retention in portal hypertensive syndrome.
Key features of the intervention!
The advantages of vein embolization include:
- High speed of intervention. The operation takes 30-60 minutes. Complex procedures may take longer.
- No significant discomfort. Pain and any discomfort during vein embolization are relieved with special modern medications.
- Speed of recovery after intervention. The patient will have to stay in the clinic for only 1-2 days. Note! In some cases, the length of hospitalization after vein embolization increases. In any case, the patient can return to normal life in the near future.
What recommendations do doctors give to patients?
- Strengthening the drinking regime. In the first 7 days after surgery, you need to drink plenty of clean water.
- Elimination of water procedures for 3-5 days. After this, you can take both a shower and a bath.
- Physical peace. It is usually prescribed for 2-3 weeks. Patients are prohibited from lifting heavy objects or playing sports. Bed rest is not prescribed for this period. Slow walks are even beneficial.
What lifestyle should I lead after embolization of esophageal vessels?
Patients should:
- Follow a specially prescribed diet that includes a large number of foods that help reduce total cholesterol levels.
- Avoid heavy exertion.
- Take various medications. They will be prescribed by your attending physician.
- Eat food often enough, but in as small portions as possible. The daily dose is best divided into 5-6 doses. Eating food is undesirable 2-3 hours before bedtime.
- Give preference to boiled dishes. Food can also be steamed. This way it retains a lot of useful substances, is easily digestible and does not become a source of additional harmful cholesterol.
It is forbidden to eat too hot or cold food. This can damage the esophagus and its veins.
PORTAL GASTROPATHY
Portal hypertensive gastropathy is inherited from portal hypertension with capillary dilatation and rupture of internal mucosal arterial shunts. This indicates the importance of maintaining the liver, which may occur in patients with hepatic portal block. With morphological examination, dilatation of vessels of both the mucous and submucosal balls is indicated. Hemorrhage in the mucous membrane is associated with thrombocytopenia, which develops with liver cirrhosis. With portal gastropathy, the sensitivity of the mucous membrane to various ear-causing agents increases: aspirin, alcohol, etc. Regression of portal gastropathy after transhepatic portosystemic shunting and reduction - after sclerotherapy or ligation of varicose veins is indicated.
The New Italian Endoscopic Club (1997) recommends that the diagnosis of portal gastropathy be based on four signs: mosaic appearance of the mucous membrane, appearance of red spots (mild stage), cherry-red spots, black-brown spots (important). step). The body of the slut is struck in front of us.
It is important to note that portal gastropathy can occur in patients with arterial hypertension without PG, and also in patients without other illnesses, its manifestations can progress, and also disappear. Bleeding, referred to as portal gastropathy, is rarely massive and more often leads to chronic bleeding.
The main advantages of the vein embolization method used in the center of Professor Kapranov
Endovascular embolization in our center is a low-traumatic procedure. It is fundamentally different from standard surgical interventions in the absence of large incisions in the vein and tissue. In addition, embolization does not require the patient to be put under general anesthesia. This reduces numerous risks and makes intervention possible in the presence of general contraindications to standard surgery.
The advantages of carrying out the intervention at the center of Professor Kapranov also include:
- Experience of professionals. All doctors performed a lot of interventions to restore the functionality of the esophagus. They are ready to help you too.
- Comfortable conditions of stay in any clinic. Embolization of the esophageal vessels will not cause pain or severe discomfort.
- Reducing the likelihood of relapse. The technique used to block the vessel allows you to quickly and reliably stop the blood flow of the vein (vessel) of the esophagus.
- No discomfort when restoring the functionality of the esophagus. During vein embolization, the patient does not experience pain. All unpleasant sensations are eliminated with the help of special medications.
- Short recovery period after intervention for varicose veins of the esophagus. For minor vascular interventions, the patient may be discharged on the day of the procedure. In this case, special care, complex treatment, and regular dressings are not required.
- Minimal number of contraindications and complications. The success of an operation for embolization of esophageal vessels largely depends on the professionalism of the doctor. That is why it is important to choose a surgeon wisely.
- Opportunities for organ preservation. Esophageal embolization, for example, avoids a number of serious problems.
External factors
In addition to pathological causes, there are a number of extraneous causes that can affect the appearance and development of the disease, these include:
In addition to pathological causes, there are a number of extraneous causes
- alcohol abuse;
- medications that negatively affect the condition of the liver;
- some diseases transmitted by inheritance;
- viral diseases affecting the liver (hepatitis).
Important! Pregnant women should pay increased attention to their health, since any viral infections suffered during this period can be transmitted to the fetus, increasing its risk of developing esophageal varices.