October 12, 2021
2033
The federal chain of pharmacies "Omnifarm" offers a wide range of metabolic drugs. Modern drugs to improve metabolism can be ordered in Moscow and other regions. You can get the necessary medications at the nearest pharmacy, taking into account the geolocation of our network. It includes 20 pharmacies offering convenient services and a help system operating throughout Russia.
On the site you can find the necessary drugs to improve metabolism, designed to speed up metabolism. You can search by name, main component or manufacturer. For all medicines, upon request of the buyer, a certificate is provided along with the receipt.
Types of metabolic disorders, what medications are needed
Among the main factors causing metabolic disorders in the body are insufficient physical activity, unbalanced nutrition, and hormonal predisposition. Various acute and chronic diseases also affect human metabolism. Metabolics are drugs that correct metabolism and vital energy in the body, helping to speed up metabolism.
Types of violations in the digestibility and processing of elements occur in the main categories:
- protein metabolism;
- carbohydrate;
- fat metabolism;
- vitamins and minerals;
- water-mineral;
- acid-base;
- hormonal balance.
Proper metabolism and comprehensive weight loss are ensured by various fat-burning, tonic, and immunostimulating agents. The medications your doctor prescribes to improve your metabolism will differ in each of these cases. They are designed to regulate metabolic processes occurring in the body.
- Restore functionality at the cellular level and eliminate metabolic failures.
- The processes of processing useful components supplied with food are brought to a normal state.
- Restore complex biochemical reactions occurring in the human body.
- They establish the production of the necessary energy for normal life.
There is no one cure for all metabolic disorders in the body. In medical practice, different types of drugs are used to normalize the breakdown and processing of fats, the absorption of proteins, carbohydrates, minerals, vitamins, and the correct balance of hormones.
Modern view on the role of metabolic therapy in the treatment of diseases of the cardiovascular system
Lecture transcript
All-Russian Internet Congress of Specialists in Internal Diseases
00:00
Vladimir Trofimovich Ivashkin, Academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
– We have the next message. Professor Alexander Anatolyevich Simakov.
"Modern view on the role of metabolic therapy in the treatment of diseases of the cardiovascular system."
Please, Alexander Anatolyevich.
(Slide show).
Alexander Anatolyevich Simakov, professor, doctor of medical sciences:
– Thank you Vladimir Trofimovich.
(Slide show).
I want to start by saying that we all work in clinics and we all have our own patients. And most importantly, we all have our own students and graduate students with whom we work, from whom we grow our shift. When a patient comes to our clinic, a young doctor always turns to his mentor, usually with two questions: what do clinical recommendations say about this disease in this case, and how best to treat the patient.
The first question reflects the application of randomized clinical trials to real-world practice. And the second implies a specific patient with individual physical, mental, social and some other characteristics of the patient. And also, most importantly, the subjective opinion of experts. Although medicine purports to be a mixture of these concepts, they are in fact diametrically opposed to each other.
(Slide show).
I would even call it (you know, Vladimir Trofimovich, Oksana Mikhailovna) not so much “The Role of Metabolic Therapy”, but rather “What is medicine in general” from the position of relationships. This is science, art or certain rules, recommendations.
01:22
(Slide show).
Most clinical guidelines allow us to optimize treatment and standardize outcomes. The clinical opinion of the doctor should not be underestimated at all. A subjective study of the protocol and (inaudible, 01:40) of the doctor can sometimes provide better knowledge of the protocol.
There is, I want to say, such an example of BARI. It is not very well known, this study, in Russia. This study looked at the mortality rate of diabetic patients who underwent percutaneous angioplasty CABG after 7 years of treatment. It has been included in various recommendations. At the same time, mortality in percutaneous angioplasty was higher than in CABG, although in the BARI registry of this study it was just lower. This situation occurred with clinical trials.
In addition, this adherence to treatment is a reflection of the relationship between the patient and the doctor, the effect and the placebo, and the preference of the patient himself. By the way, this is very well illustrated by alternative medicine. For example, homeopathic, where these ingredients act as the main factors.
(Slide show).
What I want to do again is at the beginning. It is clinical research that is the basis for many doctors and many researchers as a way to treat patients. If a drug is not included for one reason or another, for example, in recommendations or in RCTs, doctors do not prescribe it. It is the recommendations, standards, and protocols that are the basis for not prescribing this drug.
But it is well known that healthcare systems and clinical practice differ significantly from country to country. All of this affects the outcomes of randomized trials (ECST studies). From a safety point of view: in randomized studies only experienced specialists should be taken into account (work), but in real practice this does not always happen, unfortunately.
(Slide show).
Another problem is patient selection. The CASE study (almost a classic): almost 17 thousand patients - of which only 780 patients were included. This is less than 5%. As a consequence of strict inclusion/exclusion, most patients are left out of clinical trials - the results obtained are not applicable to them.
According to the National Institutes of Health, the average exclusion rate in RCTs is 73%. I sometimes think when I read these studies, where did they recruit such patients into the study? Patients included differ from others in gender, age, nationality, severity of the disease, social class and, subsequently, in the characteristics of the outcome of this disease.
04:08
(Slide show).
A special period is the run-in period of randomization, which is necessary to select patients who meet the requirements of the protocol. In the case of an introductory period with active treatment, patients with side effects and treatment failure are not included in the main part. Thus, when using Carvedilol, 6–9% were excluded from the study for one reason or another.
(Slide show).
Sometimes only patients with a good response to treatment continue further participation. All this reduces the sharp validity of the results obtained.
There are such CONSORT recommendations. These are uniform requirements: when you publish in biomedical publications, be sure to include all exclusion criteria.
(Slide show).
This is the data I found in the National Library in Washington. The National Institutes of Health meets these requirements in only 63% of cases when publishing randomized clinical trials and in 19% of clinical recommendations.
(Slide show).
The same is true for reports of adverse events or abnormal laboratory values, especially if the sponsor is the manufacturer. Of the 192 RCT reports on adverse effects, only a third provided information on the frequency of adverse events and changes in laboratory parameters.
(Slide show).
There are also difficulties when using surrogate and combined points as treatment. In real clinical practice, the results obtained in RCTs are not always applicable.
05:40
(Slide show).
Surrogate points are not considered a valid end point. Only such hard ones, such as mortality, the incidence of heart attack, stroke, can be considered from a position of significance. But the patient may be interested in other indicators. They are interested in quality of life, emotional comfort, general tone, and cognitive functions. He may not live as long as according to other studies, but it is the quality of life that is extremely important to him. For example, in a patient who develops dementia, life expectancy is not an adequate effect for the patient.
(Slide show).
For all the reasons listed above, real-world data (obtained from registers) are often more applicable in everyday work. It is known that RCTs do not take into account the formation of a therapeutic relationship between doctor and patient and the preferences of their patient. They also cannot exclude unintentional errors, for example, when adjusting factors.
(Slide show).
Although randomized clinical trials are fundamental to determining the effectiveness of treatment, we must always be aware of the low external validity of the data obtained. This occurs in guidelines where direct extrapolation of RCT data to the general population occurs. If more than 70% were excluded during the selection process, then the results obtained cannot be used without correction for the individual characteristics of the patient. Moreover, the best strategy requires modification of clinical recommendations.
(Slide show).
It should be noted that the term “evidence-based medicine” has recently undergone significant transformation. If you look at Sacket's original definition, "evidence-based medicine" is the conscious, precise, intelligent use of the best evidenced methods to decide on a patient's treatment strategy.
(Slide show).
Even if a young specialist asks his experienced colleague what the recommendations say, he will always make allowances for a specific patient. All this makes it possible to draw the following conclusion: medicine is not just about following recommendations.
Light as a physical structure can (depending on the need and methodology) be described from two positions: corpuscular and wave. This is a good example of complementarity.
07:53
(Slide show).
The term “complementarity” is generally understood in science and in art as the concept of two opposites interconnected. Romanticism during the Renaissance appeared as a result of the rejection of scientific rationalism not only in literature, but also in science.
(Slide show).
In a broad sense, this came down to the unity and struggle of two opposites: day and night, rationalism and irrationalism, the general and the individual.
(Slide show).
We often classify medicine as a natural science, but each patient has its own unique characteristics. The complementary approach in medicine implies an individual approach to the suffering person. From this point of view, medicine is not only a science, but also an art. From this point of view, it is absolutely logical that we should use not only those drugs that are included in the recommendations, given their fairly large number of shortcomings, but also the specific patient.
From this position, I would like to continue the topic of what we have been doing in our clinic for 20 years - this is the so-called metabolic therapy. If we look at the recommendations of the Europeans, they are present there, in 2006 there was stable angina, an energy modulator is present, but only for stable angina.
When you talk about cytoprotectors, many people say: “They are not in the recommendations, and we will not use them.” Doctors have a jumble in their heads: what is a cytoprotector and metabolic drugs. They often say: “Something like this is happening in the heart muscle. It’s impossible to understand what’s happening there.”
09:25
(Slide show).
I labeled the next slide as follows: cytoprotectors are an underestimated opportunity. Yes, only for stable angina, an energy modulator is recommended in European guidelines. But when I was preparing the lecture, I still tried to understand what we classify as cytoprotectors. Three positions must correspond to them: cellular metabolism, ion homeostasis and influence the structure and function of cell membranes.
If a drug has a proven experimental clinical effect, it can be classified as a cytoprotector. Everything else is beyond this concept. For myself, as a doctor, I know only three such drugs: ranolazine, which was removed from the market due to the influence of some (inaudible, 10:04), Trimetazidine and the drug with which we have been working for more than 20 years – phosphogenic creatine or “Neoton”.
(Slide show).
This energy production shown at the top is normal. It is produced by glucose and free fatty acids. Beta oxidation produces 60–80% of ATP, but requires a lot of oxygen. Glucose. If there is a lack of oxygen, then at the level of the first act everything ends, and the pH of the cell changes.
(Slide show).
Phosphogenic creatine is a drug that has been studied for a very long time. It should be noted that it was Russian scientists (Academician Sachs, Professor Rudai, Shakhov) in Moscow who developed this drug in their time. Unfortunately, he left us for Italy, but soon, as far as I understand, the patent will return to us. This is a drug that satisfies all three positions: it affects the cell membrane, it changes the energy pool and changes the pH of the cell in terms of removing acidosis.
(Slide show).
These are four slides, they talk about how phosphogenic creatine or “Neoton” affects energy production.
(Slide show).
I won’t go into detail - these are more biochemical. This is Lochman's reaction.
(Slide show).
This is a diagram of the creative path. This beautiful slide shows where the source of fast energy (to which points) is applied. Here in words we have stated it. Cytoplasmic membrane. Mitochondria are charged. On the action of ions and myofibrils. This is where the energy of the cardiomyocyte is required for contraction.
11:45
(Slide show).
The energy consumption of cardiomyocytes is broken down here: 80% for contraction, 10–15% for excitability, and 5–10% for the passage of ATP channels.
(Slide show).
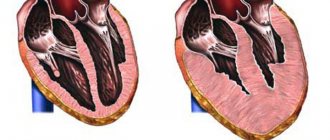
In heart failure, especially over a long period of time, and in CHF in particular, the process of transfer and utilization of ATP in cardiomyocytes is disrupted. The level of phosphogenic creatinine decreases by 70% already in the early stages. Chronic heart failure leads to depletion of energy resources.
(Slide show).
These are the indicators according to the New York classification. It is no coincidence that chronic heart failure (CHF) is considered an epidemic; more patients die from it than from oncology. Treatment of this situation is a hot topic.
(Slide show).
Here is the ratio of phosphocreatine in patients with CHF for three years showed that while preserving resources, the survival rate of these patients increases.
(Slide show).
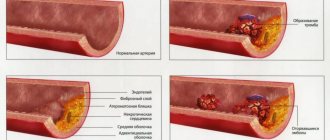
The mechanisms of irreversible damage to cardiomyocytes are outlined on this slide. This is a metabolic product, a change in the structural membrane, destruction of the cell membrane and a massive entry of various calcium into it.
(Slide show).
All this leads to an irreversible decrease in cells.
(Slide show).
The mechanism of protective action is multifaceted.
(Slide show).
It includes these four positions, protects membranes, is somewhat reminiscent of an anti-aggregation drug - it gives aggregation inside the cell and inhibits nucleotides, which produce energy.
13:20
(Slide show).
This drug affects all three links that we mentioned:
— cell membrane (here it is outlined here);
(Slide show).
— stabilization occurs during the interaction of charges of the zwitterion molecule;
(Slide show).
- phospholipase is involved.
(Slide show).
Clinical manifestations in patients with myocardial infarction: heart rhythm disturbances are reduced precisely due to the cell membrane. It is not an antirhythmic drug, but by stabilizing the membrane, it prevents arrhythmia from occurring.
(Slide show).
Contractile functions of the heart in experiment and in the clinic (Grazioli conducted a study in 1992, and it completely satisfied evidence-based medicine).
(Slide show).
The addition of "Neoton" or exogenous phosphocreatines to heart failure reduced its class according to the New York classification.
(Slide show).
Ventricular arrhythmia of heart failure for the same reason.
(Slide show).
Here are separate groups that we have studied a lot - these are acute forms, metabolic drugs, cytoprotectors. This is myocardial infarction in particular.
(Slide show).
Where phosphogenic creatine (“Neoton”) was added to the cardio shift, both the size of myocardial infarction and its mass decreased (there are corresponding calculations based on gram equivalents).
(Slide show).
The dynamics of troponins occurred faster, the time of normalization of other cardiac-specific enzymes when using “Neoton” in different schemes. Moreover, this is a dose-dependent drug.
(Slide show).
For the same reason, there was a decrease in ventricular tachycardia. That is why, Vladimir Trofimovich, we had a very good effect with post-reperfusion arrhythmias. I have published almost 15 candidate and doctoral dissertations, where we used phosphogenic creatine or “Neoton” as the main drug.
In conclusion, I want to say that if the European recommendations include an energy modulator only for chronic forms, for stable angina, then according to our research they should also be used in acute forms of coronary artery disease. For myocardial infarction, unstable angina, during thrombolysis. There are very interesting works by cardiac surgeons on the use of this drug as plegic solutions.
This is what I wanted to say in the time you gave me. Thank you very much for your attention.
Vladimir Ivashkin: Thank you very much.
15:45
Drugs for lipid metabolism disorders
Violation of lipid metabolism occurs due to failures in the absorption and breakdown of lipids (fats) with the formation of accumulation and the appearance of excess weight or active processing and depletion. This directly affects human morbidity and the occurrence of severe pathologies of the gastrointestinal tract and blood vessels. Medicines to improve fat metabolism include different drugs:
- Enzymes;
- Metabolics;
- Antioxidants;
- Fibrates;
- Statins (lowering cholesterol);
- Combined metabolism correctors.
Vitamins for impaired lipid metabolism include Fish oil, Nicotinic acid, vitamin E (retinol acetate or palmitate).
Metabolic syndrome - symptoms and treatment
Treatment of metabolic syndrome should be divided into non-pharmacological and medicinal.
Non-drug treatment of Reaven syndrome is maintaining a healthy lifestyle, quitting smoking and alcohol abuse, optimal physical activity [14], balanced nutrition, as well as the reasonable use of natural and preformed physical healing factors (massage, underwater shower massage, hypoxic therapy and hypercapnia, hydrotherapy, thalassotherapy, balneo- and thermotherapy, internal intake of mineral waters, general magnetotherapeutic effects)[15], psychotherapeutic techniques and training programs.[13]
Drug treatment of metabolic syndrome, depending on the presence of certain of its components, may include lipid-lowering, antihypertensive drugs, medications to reduce insulin resistance, postprandial hyperglycemia and weight.
The main drugs used in the treatment of arterial hypertension in patients with Reaven syndrome and diabetes mellitus are angiotensin-converting enzyme inhibitors, sartans and imidazoline receptor agonists. However, achieving target blood pressure often requires a combination of different classes of medications, such as long-acting calcium channel blockers, highly selective beta-blockers, and thiazide-like diuretics (indapamide) in combination with first-line medications.[10]
To correct lipid metabolism disorders in metabolic syndrome, statins are initially used, possibly in combination with esetrole and fibrates. The main mechanism of action of statins is a decrease in intracellular OX synthesis due to reversible blocking of the enzyme 3-hydroxy-3-methylglutaryl-coenzyme A reductase. It leads to an increase in the number of LDL-C receptors on the surface of the hepatocyte and a decrease in the concentration of LDL-C in the blood. In addition, statins have pleiotropic effects, such as antithrombogenic, anti-inflammatory, and improvement of endothelial function, which leads to stabilization of atherosclerotic plaque. Modern statins are capable of reducing LDL cholesterol by up to 55%, reducing triglycerides by up to 30% and increasing HDL cholesterol by up to 12%. At the same time, the key advantage of statin therapy is the reduction of cardiovascular complications and overall mortality[1]. It is most effective to use atorvastatin (10-80 mg/day) or rosuvastatin (5-40 mg/day).[11]
If statin monotherapy is ineffective, it is advisable to add ezetrol at a dose of 10 mg/day, which prevents the absorption of TC in the intestine and can enhance the reduction of LDL-C by 15-20%.
Fibrates are another class of lipid-lowering drugs. They break down triglyceride-rich fat particles, reduce the synthesis of free fatty acids and increase HDL-C by increasing the breakdown of LDL. This leads to a significant decrease in triglycerides (up to 50%), LDL-C (up to 20%) and an increase in HDL-C (up to 30%). Fibrates also have pleiotropic effects: they reduce the concentration of uric acid, fibrinogen and improve insulin sensitivity, but their positive effect on the prognosis of patients has not been proven. The most effective and safe drug in this group is fenofibrate 145 mg/day.
To reduce insulin resistance, the drug of choice is metformin, which has a proven positive effect on tissue insulin resistance through enhancing glucose uptake by target tissues. Metformin reduces the rate of absorption of carbohydrates in the small intestine, has a peripheral anorexigenic effect, reduces glucose production by the liver, and improves glucose transport within cells. The positive effects of metformin (1500-3000 mg/day) on endpoints are due to a decrease in insulin resistance, systemic metabolic effects (weight loss, lipid disorders, blood clotting factors, etc.).[9]
To reduce postprandial hyperglycemia, acarbose is used, which reversibly blocks glucoamylase, sucrose and maltase in the upper small intestine. As a result, undigested carbohydrates reach the lower intestines, and the absorption of carbohydrates is prolonged. However, acarbose has been shown to have additional effects. The STOP-NIDDM study (2002) in patients with metabolic syndrome taking acarbose at a dosage of 300 mg/day demonstrated a reduction in the development of diabetes mellitus by 36%, new cases of arterial hypertension by 34%, and the total rate of cardiovascular events by 46%[6 ].
If a patient with Reaven syndrome has type 2 diabetes mellitus, modern classes of antihyperglycemic drugs, such as glucagon-like peptide analogue-1, dipeptidyl peptidase-4 inhibitor, and sodium-glucose transporter type 2 inhibitor, can be used. A representative of the latter class, empagliflozin (Jardins), in the EMPA-REG OUTCOME study (2016) reduced cardiovascular mortality in patients with type 2 diabetes by 36%.
Drug correction of morbid obesity is indicated if non-drug treatment does not lead to a decrease in body weight by more than 5% of the initial one. Drugs for the treatment of obesity are divided into centrally acting anoretic drugs (sibutramine) and drugs that act on the gastrointestinal tract, such as orlistat (Xenical).
The appetite suppressant drug sibutramine has a lesser effect on dopamine and cholinergic processes, but reduces the consumption of fats and carbohydrates, which leads to weight loss and improves fat and carbohydrate metabolism. Blood pressure and heart rate increase by only 5%.
Orlistat is an inhibitor of gastric and pancreatic lipases, as a result of which a third of dietary triglycerides are not absorbed and their concentration in the blood decreases, which leads to a decrease in food calories and weight. In addition, blood pressure, glucose levels and insulin resistance are reduced.
In medical practice, treatment of metabolic syndrome depends on the presence and severity of its components. The table below shows the tactics for selecting therapy for the most common variants of Reaven syndrome.
| AO+AG+NTG (SD) Moderate SSR | AO+AG+DL High SSR | AO+AG+NTG (SD)+DL High and very high SSR | ||
| D/FN+AGP+GGP | D/FN+AGP+GLP | D/FN+AGP+GGP+GLP | ||
| Note CRR – cardiovascular risk; AH – arterial hypertension; AO – abdominal obesity; DL – dyslipidemia; IGT – impaired glucose tolerance; DM – diabetes mellitus; D/FN – diet/physical activity; AHP – antihypertensive drug; HGP – hypoglycemic drug; GLP is a lipid-lowering drug. | ||||
Metabolism of vitamins, micro- and macroelements
Pharmacological drugs that help improve the metabolism of vitamins and minerals are prescribed in the following cases:
- lack of these elements in the body;
- excessive intake from food;
- failures in breakdown and digestibility;
- imbalance of vital systems.
As a result of hypovitaminosis or hypervitaminosis, deficiency of micro- and macroelements, a huge range of severe pathologies arises. An imbalance of these components causes illness, affects the condition of hair, skin, nails, and directly affects a person’s appearance.
For example, iodine deficiency leads to the development and progression of thyroid disease and an imbalance of thyroid hormones. Due to hormonal imbalance, weight changes occur. An excess of this microelement in the body is also dangerous; it can cause disruptions in the endocrine system. Therefore, it is recommended to use drugs as prescribed by a doctor.
A huge selection of multivitamin complexes with the rarest vitamins and microelements allows you to undergo a full course of treatment and restore the lost balance.
An exceptional correction of mineral metabolism is carried out with preparations containing iron, copper, zinc, phosphorus, calcium, chromium and others. Ferrum-LEK, rich in iron, allows you to replenish your body with this useful element. This complex is prescribed for iron deficiency anemia and pregnancy.
Detailed description of the study
Metabolic profile is a comprehensive laboratory test that allows you to assess the rate of metabolism (metabolism) and identify disturbances in this process, which can cause obesity, reproductive disorders, diseases of the cardiovascular system and many other pathological conditions.
This set of laboratory tests includes the determination of the following indicators: Thyroid-stimulating hormone (TSH) is a hormone produced by the pituitary gland (the gland that synthesizes hormones and is located at the base of the skull). TSH is involved in the regulation of the synthesis of thyroid hormones (thyroxine, tetraiodothyronine (T4) and triiodothyronine (T3)), stimulating the production of T4 and T3.
The level of TSH in the blood serum determines the presence of hyperthyroidism - overproduction of thyroid hormones - when the TSH concentration is below normal, and hypothyroidism (deficiency of thyroid hormones) when the TSH level is elevated. These pathological conditions are characterized by normal levels of T3 and T4.
T3 and T4 in the blood are almost completely bound by protein. A small part of the hormones remains unbound (free) and represents a biologically active form.
If the thyroid gland produces an excessive amount of T4, then a person may experience symptoms of hyperthyroidism: increased nervous excitability, rapid heartbeat, sweating.
If the thyroid gland does not produce enough T4, this condition is characterized by the presence of symptoms associated with hypothyroidism: facial swelling, peeling skin, constipation, and menstrual irregularities.
Both hyperthyroidism and hypothyroidism can also be associated with thyroid cancer or over/under TSH production. Differential diagnosis of these conditions can be made by measuring free T4 levels.
Cortisol (hydrocortisone) is a glucocorticoid hormone of the adrenal cortex, which is involved in the regulation of the metabolism of fats, proteins and carbohydrates in the body. The production of cortisol depends on the functional activity of the adrenal glands and the state of the pituitary gland.
In blood plasma, cortisol is presented in a free, that is, biologically active form (about 5% of all produced cortisol) and compounds with plasma proteins (mainly transcortin and albumin), as well as in the form of metabolites.
The secretion of cortisol in a healthy person is 15–30 mg and normally has a pronounced circadian rhythm. The highest concentration is observed in the early morning, then the level of the hormone gradually decreases throughout the day and reaches a minimum around midnight. This pattern may change if a person has a number of diseases associated with suppression or enhancement of hormone synthesis.
The combination of clinical symptoms that occur with chronically elevated cortisol levels is called Cushing's syndrome. Characteristic clinical symptoms include:
- Moon-shaped face;
- Central type of obesity;
- Thin limbs;
- Purple stretch marks (stretch marks) on the abdomen;
- Poor wound healing.
In high concentrations, cortisol increases sodium absorption and potassium excretion, which contributes to fluid retention and the occurrence of edema, the development of arterial hypertension and arrhythmia (impaired heart rate).
An excess of the hormone can provoke the development of neuroses, including delusional disorders and severe clinical depression.
Insulin is produced by the pancreas; its main task is to transport glucose from the blood into the cells of the body. Thus, it participates in the regulation of energy metabolism.
In the pancreas there are specialized cells (beta cells), in which biologically inactive preproinsulin, under the influence of stimulating factors (increased blood glucose concentrations), as a result of a chain of reactions, is converted into the biologically active hormone insulin, which is released into the bloodstream.
If the functioning of the pancreas is disrupted and insulin is not produced in sufficient quantities or the cells become unresponsive to insulin (insulin resistance), then glucose does not enter the cell and is not processed. Glucose accumulates in the blood serum, which is dangerous because it disrupts normal metabolism and can lead to the development of diabetes mellitus and damage to organs and systems.
C-peptide is a fragment of the proinsulin molecule, which is formed during the biosynthesis of insulin. When insulin is released into the bloodstream, an equal amount of free C-peptide is also released.
Approximately 50% of the resulting insulin is stored in the liver, having a half-life in the blood of no more than 4 minutes. C-peptide is not removed from the bloodstream by the liver and its content in the blood corresponds to production in the pancreas. Therefore, the insulin-secreting ability of pancreatic B cells can be indirectly judged by the level of C-peptide.
The protein leptin is a peptide hormone that is involved in the regulation of energy metabolism, signaling satiety in response to food intake. The hormone is produced to a greater extent by adipose tissue cells (adipocytes), a smaller part is secreted by the placenta, skeletal muscle and gastric mucosa.
The biological action of leptin occurs through specific receptors in the hypothalamus. When leptin interacts with its receptor, the synthesis of biologically active substances that suppress appetite is activated. The formation of appetite-stimulating substances also stops. As the concentration of leptin in the blood increases, the feeling of hunger gradually goes away.
Excess leptin in the blood can in rare cases be associated with genetic defects. But most often a person stops picking up “saturation signals” due to:
- Insensitivity to the effects of leptin caused by defects in leptin receptors;
- Excessive synthesis of leptin inhibitors;
- Leptin transport disorders.
An excess of leptin provokes excessive accumulation of adipose tissue in the body, which significantly increases insulin secretion, causing hyperinsulinemia.
Normally, leptin increases insulin consumption by body tissues and reduces its production. Excess insulin caused by hypersecretion of leptin is no longer absorbed by muscles and liver cells, and the number of insulin receptors in tissues decreases, insulin resistance develops, i.e. cell insensitivity to insulin. This condition increases the risk of developing type 2 diabetes.
Glucose is the main source of energy for all cells in the body. Glucose is constantly needed by cells, so normally its level in the blood serum should be maintained at a relatively constant level.
Glucose is formed during the digestion of food containing carbohydrates. Typically, serum glucose levels increase slightly immediately after a meal. In response to this, the pancreas produces the hormone insulin, which is necessary to transport glucose to cells and tissues, where it is used for energy. As glucose is utilized by insulin, its level in the blood gradually decreases, which stops the production of insulin by the pancreas.
If this system (glucose-insulin) is disrupted, glucose remains in the blood and cannot be utilized by cells. The most common disease associated with impaired glucose utilization and insulin production is diabetes mellitus.
Significant changes in serum glucose levels provoke life-threatening conditions, causing organ dysfunction, brain damage and other serious consequences.
The atherogenicity index is an indicator that allows you to assess the risk of developing heart and vascular diseases. To calculate the indicator, two parameters are determined: the level of total cholesterol and the level of high-density lipoproteins.
Cholesterol is a fat-like substance that is necessary for the normal functioning of the body. It is part of cell membranes, is used for the synthesis of certain hormones, and produces bile acids necessary for the absorption of nutrients from food in the intestines.
Small amounts of cholesterol circulate in the blood in the form of complex particles called lipoproteins. Each particle contains a combination of protein, cholesterol, triglyceride and phospholipids. These complexes are classified according to their density into:
- High density lipoproteins (HDL);
- Low density lipoproteins (LDL);
- Very low density lipoproteins (VLDL).
HDL helps remove excess cholesterol from blood vessels (for which they are called “good” cholesterol), while LDL and VLDL, on the contrary, retain it in tissues and organs.
Excess cholesterol is deposited in the form of plaques on the walls of blood vessels. Plaques, gradually increasing in size, lead to a narrowing of the lumen of blood vessels or to their complete blockage. This increases the risk of developing cardiovascular diseases and complications of these diseases.
Low-density lipoproteins (LDL) and very low-density lipoproteins (VLDL) are the main carriers of fats (triglycerides) in the body. These classes of lipoproteins are also called “bad cholesterol” because with an increase in the level of VLDL and LDL, the risk of developing atherosclerosis (the deposition of fatty “plaques” on the walls of blood vessels) and other diseases of the cardiovascular system increases.
The studies included in this complex allow us to evaluate the main types of metabolism (carbohydrate, protein, fat), as well as the exchange of hormones and other biologically active substances, which allows us to identify disturbances in these processes. Normally, the metabolism in the human body is balanced and ensures the normal functioning of all systems and organs.
A detailed description of the studies and reference values are presented on the pages with descriptions of individual studies.
Protein metabolism disorders
Insufficient supply of protein and amino acids and metabolic disorders lead to exhaustion of the body, weakened immunity, and a decrease in the transport function for the delivery of nutrients. This deficiency causes protein-energy deficiency, which is eliminated by various drugs:
- anabolics;
- amino acids;
- vitamins and minerals;
- immunomodulators;
- general tonic compounds.
In case of insufficiency of endocrine regulation, adaptogens and general tonics are prescribed. Profound depletion and dysfunction resulting from the lack of protein in food are eliminated by drugs to improve metabolism for parenteral and enteral administration, respectively, by injection into a vein and through a tube.
References
- El-Farhan, N., Rees, D., Evans, C. Measuring cortisol in serum, urine and saliva - are our assays good enough? Annals of clinical biochemistry, 2021. - Vol. 54(3). — P. 308-322.
- Clinical laboratory diagnostics: textbook / ed. V.V. Dolgova, Federal State Budgetary Educational Institution of Further Professional Education "Russian Medical Academy of Continuing Professional Education". - M.: FGBOU DPO RMANPO, 2021. - 668 p.
- Bobrik, M.I. Mutual influence of thyroid and carbohydrate metabolism. Paradigms and paradoxes. MJE, 2015. - No. 3(67).
- World Gastroenterology Organization Global Practice Guidelines: Obesity 2015.
Carbohydrate metabolism disorders
Diabetes mellitus, pancreatitis, arterial hypertension and other diseases occur against the background of carbohydrate metabolism disorders. The body is not able to independently process the main sources of energy resources, such as:
- glucose;
- fructose;
- galactose;
- glycogen.
Drug therapy includes drugs to improve metabolism, depending on the type of malfunction in the body. For this purpose, enzymes, anti-enzymes, hypoglycemic agents, drugs that regulate uric acid metabolism and others are used. The doctor prescribes Cocarboxylase, ATP, Vitrum Cardio Omega-3, and multivitamin complexes.
Metabolic drugs in cardiological practice
Recently, interest in the metabolic direction in the treatment of stable forms of coronary artery disease has increased. Metabolically active drugs can potentially preserve the viability of the myocardium (hibernating myocardium) until surgery to restore coronary blood flow. Metabolic therapy is aimed at improving the efficiency of oxygen utilization by the myocardium under ischemic conditions. Normalization of energy metabolism in cardiomyocytes is an important and promising approach to the treatment of patients with coronary artery disease.
Possible pathways of cytoprotection:
- inhibition of the oxidation of free fatty acids (trimetazidine, ranolazine);
- increased flow of glucose into the myocardium (glucose-sodium-insulin solution);
- stimulation of glucose oxidation (L-Carnitine);
- replenishment of macroerg reserves (phosphocreatine);
- improvement of transmyocardial transport of NAD+/NADH (amino acids);
- opening of K+-ATP channels (Nicorandil).
Of the currently known myocardial cytoprotectors, the most studied drug with proven antianginal and anti-ischemic effects is trimetazidine, which exerts its effect at the cellular level and acts directly on ischemic cardiomyocytes. The high effectiveness of trimetazidine in the treatment of coronary artery disease is explained by its direct cytoprotective anti-ischemic effect. Trimetazidine, on the one hand, rearranges energy metabolism, increasing its efficiency, on the other hand, it reduces the formation of free radicals, blocking the oxidation of fatty acids [10, 13].
The mechanism of action of trimetazidine is related to:
- with inhibition of 3-ketoacyl-CoA thiolase, leading to a decrease in beta-oxidation of fatty acids and stimulation of glucose oxidation;
- optimization of myocardial function under ischemic conditions by reducing proton production and limiting intracellular accumulation of Na+ and Ca2+;
- accelerating the renewal of membrane phospholipids and protecting membranes from the damaging effects of long-chain acyl derivatives.
These processes help maintain the required level of ATP in cardiomyocytes, reduce intracellular acidosis and excessive accumulation of calcium ions.
Thus, the anti-ischemic effect of trimetazidine is carried out at the level of the myocardial cell due to changes in metabolic transformations, which allows the cell to increase the efficiency of oxygen use in conditions of reduced oxygen delivery and thus preserve the functions of the cardiomyocyte.
Trimetazidine on the Russian pharmaceutical market is represented by such drugs as Preductal (France), Trimetazid (Poland), Trimetazidine, Rimecor (Russia).
Numerous studies have convincingly demonstrated the high antianginal and anti-ischemic efficacy of trimetazidine in patients with coronary artery disease, both in monotherapy and in combination with other drugs [14, 17, 18]. The drug is no less effective in the treatment of stable angina than beta-blockers or calcium antagonists, but it is most effective in combination with basic hemodynamic antianginal drugs. The advantages of trimetazidine include the absence of hemodynamic effects, which allows the drug to be prescribed regardless of the level of blood pressure, heart rate characteristics and myocardial contractile function.
Trimetazidine can be prescribed at any stage of the treatment of angina pectoris as part of combination antianginal therapy to enhance the effectiveness of beta-blockers, calcium antagonists and nitrates in the following categories of patients:
- with newly diagnosed exertional angina;
- in whom it is not possible to achieve a therapeutic effect with hemodynamic antianginal drugs;
- in elderly people;
- with left ventricular dysfunction;
- with CHF;
- with diabetes mellitus;
- with sick sinus syndrome;
- in whom traditional antianginal drugs cause side effects;
- in persons with severe side effects during treatment with antianginal drugs.
Trimetazidine allows you to reduce the dose of drugs that have side effects, improving the overall tolerability of treatment.
Important points are the absence of contraindications, drug incompatibility, and its good tolerability. Adverse reactions occur very rarely and are always mild. This allows the drug to be used by elderly people with diabetes mellitus and other concomitant diseases.
There are no data yet on the effect of trimetazidine on long-term outcomes and cardiovascular mortality in patients with coronary artery disease, so the advisability of its use in the absence of angina or episodes of silent myocardial ischemia has not been established.
Normalization of energy metabolism in cardiomyocytes is an important and promising approach to the treatment of patients with CHF. Metabolic therapy in such patients should be aimed at improving the efficiency of oxygen utilization by the myocardium under ischemic conditions. However, there are very few studies devoted to studying the characteristics of the action of trimetazidine in patients with CHF [7, 11, 16].
In this regard, at the Department of Clinical Pharmacology and Pharmacotherapy of the FPPOV MMA named after. I.M. Sechenov conducted a study to determine the limits and capabilities of trimetazidine in the complex therapy of patients with CHF, which has complicated the course of coronary artery disease.
The study included 82 patients with NYHA functional classes II–III CHF, which complicated the course of coronary artery disease. Among them there were 67 men, 15 women, the average age was 62.2 ± 7.3 years. Before inclusion in the study, all patients achieved stabilization of their condition during therapy with cardiac glycosides, diuretics, and beta-blockers in individually selected doses. All patients were divided into two groups: the first (main) group included 40 patients, to whom trimetazidine at a dose of 60 mg/day and the ACE inhibitor enalapril at a dose of 5–10 mg/day were added to complex therapy; the second (control) group consisted of 42 patients who received only enalapril without trimetazidine to complex therapy. There were no significant differences between the groups in age, gender, duration of the disease, or functional class of CHF. The observation period was 16 weeks.
The clinical effectiveness of therapy was assessed by the dynamics of the functional class of CHF. All patients underwent Holter ECG monitoring with assessment of the average daily heart rate (HR), the total number of episodes of ST segment depression, and the maximum value of ST segment depression. ST segment trends were regarded as ischemic when it decreased horizontally by at least 1 mm relative to the J point for 1 minute or more. The anti-ischemic effect was considered significant if the number of episodes of myocardial ischemia decreased by 3 or more and/or total ST segment depression decreased by 50% or more. The nature of heart rhythm disturbances was also assessed: the number of isolated ventricular extrasystoles (VCs), paired VCs, supraventricular extrasystoles (VVCs), episodes of unsustained ventricular tachycardia (VT), runs of supraventricular tachycardia (SVT). The criteria for the antiarrhythmic effect were considered to be a reduction in isolated PVCs by 50%, paired PVCs by 90% with complete elimination of VT episodes.
To assess exercise tolerance, patients underwent a treadmill test. The criteria for a positive test were a typical attack of angina and/or persistent horizontal ST segment depression of 1 mm or more. When analyzing the results of the treadmill test, the maximum power of the load performed and the total duration of the load were assessed.
In order to assess the state of intracardiac hemodynamics, patients underwent an echocardiographic study with assessment of the following morphofunctional parameters of the heart: left atrium (LA) size, cm; end-diastolic size (EDD), cm; end-systolic size (ESR), cm; ejection fraction (EF) of the left ventricle, %.
Clinical and instrumental studies were carried out before and after 16 weeks of continuous therapy.
Statistical analysis of the obtained data was carried out using standard statistical methods, including calculation of the unpaired Student's t test. All data are presented as mean standard deviations (M ± m).
Analysis of the dynamics of the FC of CHF showed that after 16 weeks of treatment, 28% of patients in the first group and 26% of patients in the second group achieved an improvement in clinical condition and a transition to a lower FC of CHF. The number of patients with FC III decreased in the first group from 50 to 27.5%, in the second - from 64.3 to 30.9%. The number of patients with FC II increased to 67.5 and 66.7%, respectively. During treatment, patients with FC I appeared in both groups: 5% in the first group and 2.4% in the second. Overall, the FC of CHF decreased by 11% (p < 0.05) and 10% (p < 0.05), respectively (
).
According to Holter ECG monitoring at baseline, the following data were obtained in patients included in the study: NVEs were recorded in all patients in both groups; in 9 patients of the first group and in 7 patients of the second group, runs of NVT were recorded. In all patients, isolated PVCs were recorded, including potentially life-threatening PVCs of high grades: paired PVCs and episodes of unstable VT.
After 16 weeks of treatment in the first group, the number of paired VTs decreased by 57.6% (p < 0.05), in the second group - by 28.8% (p < 0.05), the number of episodes of unstable VT - by 58.3% (p < 0.05) and 36.8% (p < 0.05), respectively, the number of isolated PVCs - by 23.6% (p > 0.05) and 6.9% (p > 0.05), respectively , the number of NVEs - by 26.4% (p 0.05) and 10.8% (p > 0.05), respectively.
No new paired PVCs or episodes of nonsustained VT were reported in any patient receiving trimetazidine therapy.
According to Holter ECG monitoring, a significant decrease in the daily number of episodes of ST segment depression was noted in the first group by 55.5% (p < 0.05), in the second - by 23.3% (p < 0.05).
The improvement in the clinical condition of the patients was accompanied by an improvement in the morphofunctional parameters of the heart, which was more pronounced in patients of the first group who received trimetazidine. After 16 weeks of continuous treatment, there was a decrease in EDR in the first group by 4.7% (p < 0.05), in the second group - by 2.1% (p < 0.05); TFR - by 7.5% (p < 0.05) and 4.8% (p < 0.05), respectively; EF increased in the first group by 13.7% (p < 0.05), in the second group - by 10.4% (p < 0.05).
The results of the treadmill test provide objective confirmation of the high antianginal and anti-ischemic activity of trimetazidine: the maximum load power in patients of the first group increased by 12.3% (p < 0.05), in patients of the second group - by 6.7% (p < 0. 05), the total duration of the load increased by 16.8% (p < 0.05) and by 8.2% (p < 0.05), respectively.
Thus, a clear understanding of the pathophysiological mechanisms of damage to myocardial cells under conditions of ischemia and hypoxia, which are based on metabolic disorders, necessitates the inclusion of antioxidants and antihypoxants in the complex therapy of stable forms of IHD.
Normalization of energy metabolism in cardiomyocytes is also an extremely important and promising approach to the treatment of patients with coronary heart disease complicated by the development of chronic heart failure. Adding the metabolic drug trimetazidine to the traditional therapy of patients with CHF makes it possible to achieve more pronounced dynamics of clinical manifestations of the disease and a more pronounced improvement in the morphofunctional parameters of the heart. Along with antianginal and anti-ischemic effects, trimetazidine also has a positive effect on the contractile function of the left ventricular myocardium and reduces the ectopic activity of the heart by reducing the electrical instability of the ischemic myocardium.
To obtain evidence of the positive effect of metabolic agents on endpoints, the incidence of cardiovascular events, mortality and disease prognosis in patients with coronary artery disease, they need to be further studied in large-scale randomized trials.
For questions regarding literature, please contact the editor.
T. E. Morozova , Doctor of Medical Sciences, Professor of MMA named after. I. M. Sechenova , Moscow
Other types of metabolic disorders
The appearance of metabolic failures in muscles provokes the development of severe neuromuscular diseases. This leads to disruption of the activity of the heart and blood vessels. In these cases, antioxidants, cardioprotectors, enzymes, antienzymes and other drugs are used.
Violation of water and mineral balance leads to the appearance of edema, kidney disease, pressure surges, the formation of excess fluid in tissues and other pathological processes. Antioxidants and acid-base regulators (ABC) are prescribed.
In each case, an individual scheme is recommended:
- Prescribing and taking medications.
- Special diet.
- A radical lifestyle change.
- Correction of physical activity.
- Sleep patterns to improve brain function.
In modern neurology, metabolic therapy is widely used, in particular drugs with a cytoprotective effect. An important area of its application is the treatment of dyscirculatory encephalopathy (DE), since drugs that affect hemodynamic parameters are effective in preventing stroke, but do not protect the neuroglial complex from metabolic changes that form the basis for the progression of the pathological process. In particular, atherosclerosis leads to hypoperfusion and the development of an imbalance between the delivery of oxygen to neurons and the need for it - ischemia is formed, changing cellular metabolism. Neuronal dysfunction and clinical manifestations of the disease are based on acidosis, local inflammation and peroxidation, ionic imbalance, and a decrease in ATP synthesis [3, 11, 14].
One of the important factors in the development of tissue hypoxia in DE is microcirculation disorders [10, 20, 21]. Increased blood viscosity is a risk factor for the development of DE, transient ischemic attacks, and precedes strokes [1, 6]. There are various forms of hyperviscosity syndrome: hemoconcentration, increased cell adhesion, increased platelet aggregation and decreased red blood cell deformability, which lead to fibrin formation and thrombosis [13]. Correction of the rheological properties of blood is an important element of complex treatment of patients with vascular pathology.
There are three main areas of metabolic therapy in neurology: prevention of necrosis and apoptosis of neurons; optimization of energy formation and consumption processes; normalization of the balance between the intensity of free radical oxidation and antioxidant protection. For this purpose, antihypoxants are prescribed in clinical practice to optimize mitochondrial functions, activate the Krebs cycle, and prevent the uncoupling of oxidation and phosphorylation [16, 18].
The range of drugs that can effectively influence the rheological properties of blood is limited. Albumin solutions are used for this purpose, but a significant number of side effects limit their use [12]. Plasma-substituting solutions, dextran preparations, derivatives of gelatin, hydroxyethyl starch, and polyethylene glycol are widely prescribed. They have a normovolemic effect due to the entry of interstitial fluid into the vascular bed, as well as an antithrombotic effect [2, 15], but require caution when prescribed to patients with cardiac and respiratory failure.
Considering the above, the means of choice for the correction of hemorheological disorders should be drugs that are safer and more effective. Of interest is the original drug created on the basis of polyhydric alcohols - rheosorbilact, 1 liter of which contains sorbitol - 60.0 g, sodium lactate - 19.0 g, sodium chloride - 6.0 g, calcium chloride - 0.1 g, potassium chloride - 0.3 g, magnesium chloride - 0.2 g, water for injection - up to 1 l; osmolarity 900 mOsm/l; energy value - 240 kcal/l; pH 6.0-7.6. Reosorbilact has a multifunctional effect, normalizing several types of homeostasis disorders: due to hyperosmolarity, rheosorbilact causes fluid to flow from the intercellular space into the vascular bed, improving microcirculation and tissue perfusion; sorbitol, partially metabolized to fructose, helps normalize carbohydrate and energy metabolism (in this case, sorbitol, unlike glucose, is metabolized without the participation of insulin), which has a particularly beneficial effect on improving the functional state of neuroglia and hepatocytes, in which the glycogen depot is restored; sorbitol stimulates the oxidation of fatty acids through the non-ketogenic metabolic pathway and facilitates the inclusion of ketone bodies in the Krebs cycle; sorbitol increases intestinal motility due to a direct effect on the neuroreceptor apparatus of the intestinal wall and increased synthesis and secretion of villikinin, cholecystokinin and B vitamins; sodium lactate helps correct the acid-base balance of plasma, lactate anion restores and stimulates the functions of cells of the reticuloendothelial system of the liver and kidneys. These properties make it possible to use rheosorbilact to correct water-electrolyte, acid-base and energy balance, and improve the rheological properties of blood.
The purpose of the work is to study the possibility of using rheosorbilact as a means of metabolic therapy in neurological practice.
Material and methods
An open clinical study of the effectiveness of the drug rheosorbilact as part of complex therapy for patients with DE and diabetic polyneuropathy (DPN) was conducted. The study involved 89 patients aged from 42 to 70 years (average - 54.2±5.8 years).
The criteria for inclusion of patients in the study were a verified diagnosis of stage I-II DE or DPN, as well as the availability of informed consent from the patient. Exclusion criteria were alkalosis, individual intolerance to the components of the drug, gastric ulcer, hemorrhagic colitis, severe liver disease, refractory arterial hypertension and heart failure in the stage of decompensation.
The first group consisted of 45 patients, 25 men and 20 women, with DE, who were randomized into two subgroups comparable by gender, age and body mass index. In the treatment of 20 patients of subgroup Ia, nootropic, vascular, and vitamin preparations were used. Complex therapy for 25 patients of subgroup Ib, in addition, included the administration of rheosorbilact 200-400 ml per day (at the rate of 3 ml/kg) intravenously at a rate of 80 drops per minute every other day for 20 days.
The second group included 44 patients, 24 men and 20 women, with DPN, who were also divided into 2 comparable subgroups IIa and IIb of 22 patients each. Complex treatment of patients in both subgroups included vitamin preparations and thioctic acid.
In subgroup IIb, in addition, parenteral administration of rheosorbilact was used according to the above scheme.
The study included a screening period, a period of active treatment, a stage of observation and analysis of results. At the screening stage, the patient's compliance with the inclusion/exclusion criteria was determined. After a 20-day course of treatment, patients remained under observation for another 10 days. The total duration of the study was 30 days.
The primary end point of the study in both groups of patients was improvement in the quality of life of patients 1 month after the start of treatment, assessed on the SF-36 scale. All patients of group 1 before treatment and on the 30th day of observation, in addition to a neurological examination [8], underwent a study of cognitive functions using a battery of frontal dysfunction tests (FAB), a brief mental function assessment scale (MMSE), and also studied parameters acid-base balance in venous blood (pH and base excess - BE). Before the start of the study and upon its completion, duplex ultrasound scanning (USDS) of the main arteries of the head was carried out on the SONOLINE Elegra device (Germany, SPECTROMED) using a 7 MHz linear sensor. The study included determination of the intima-media thickness (IMT) of the carotid arteries at standard points; diameters of the common (CCA) and internal (ICA) carotid arteries; degree of stenosis according to the ECST criterion [11]. Velocity and spectral parameters of blood flow were determined in the CCA, ICA and vertebral arteries (VA) at the extracranial level. Peak systolic and end-diastolic blood flow velocities, time-averaged peak and volumetric blood flow velocities (Vvol) were assessed separately in each vessel; We also assessed the total volumetric blood flow velocity in the CCA (σVvol CCA) and PA (σVvol PA), and the total volumetric velocity of cerebral blood flow (σVvol MC).
In group 2, in addition to assessing quality of life according to SF-36, anxiety level (HARS questionnaire), pain intensity (NRS questionnaire) and parameters of the acid-base state in venous blood (pH and BE) before treatment and on the 30th day of the study We analyzed the concentration of glucose in capillary blood and performed electroneuromyography (ENMG) of the tibial and peroneal nerves using the Nicolet Viking-IV diagnostic complex (USA). The velocity of impulse conduction along motor fibers (SPI eff), the velocity of impulse conduction along sensory fibers (SPI eff), the amplitude of the M-response, and the latent period of the evoked potential were studied. The severity of treatment side effects was assessed using the UKU side effect rating scale [17].
Statistical analysis of the obtained data was carried out using the Statistica 6.0 program in accordance with the recommendations for processing the results of biomedical research [9]. The choice of methods was carried out taking into account the principles of system analysis and modeling of dynamic research. The conclusion about statistical significance was given at the level of probability of an erroneous conclusion p
<0,05.
results
In the initial period of the study, astheno-neurotic syndrome predominated in the majority of patients with DE; in the neurological status, diffuse neurological symptoms, lateralized pyramidal-cerebellar deficit and mild cognitive disorders were observed (Table 1)
.
An analysis of the acid-base state of the blood in this category of patients revealed a base deficiency (BE) at a normal pH value, which indicated a mild acidosis, which probably developed due to insufficient energy supply to the tissues during their chronic hypoperfusion.
Patients with DE noted a decrease in quality of life indicators (on the SF-36 scale) in the physical and psychological spheres, which corresponded to the nature of the complaints. After 30 days of observation, in patients with DE in subgroup Ia, there was only a tendency to improve the indicators of the studied parameters in the absence of statistically significant changes. An improvement in their quality of life by the end of the study was observed mainly due to the psychological component. In patients of subgroup Ib, significant changes were revealed in a number of studied parameters compared with similar indicators in subgroup Ia and the initial data. Thus, according to the results of USDS analysis, a significant ( p
<0.05) improvement in the total volumetric blood flow velocity in all studied systems (CCA, PA, MK), which indicated an increase in cerebral perfusion.
In addition, there was a significant decrease in the severity of blood acidosis due to a significant restoration of base deficiency (up to –2.0±1.7 mmol/l, p
<0.05), not accompanied by a pronounced change in blood pH.
There were no significant differences in changes in the average scores of the MMSE and FAB scales compared to the initial values. Patients in this subgroup noted a significant improvement in quality of life by the end of treatment ( p
<0.05) due to both physical and psychological components.
At the screening stage, the vast majority of patients with DPN complained of numbness and paresthesia in the feet, worsening at night. The neurological status was dominated by polyneuritic syndrome with damage to the lower extremities, accompanied by moderate pain (according to the NRS scale). Peripheral blood examination revealed mild hyperglycemia and metabolic acidosis (based on BE study) with a normal pH. ENMG of the nerves of the lower extremities made it possible to establish a significant decrease in SPI in sensory and motor nerve fibers, a decrease in the amplitude of the M-response and an increase in its latency.
After 30 days after the start of treatment, in patients of subgroup IIa who received conventional complex therapy for DPN, a significant ( p
<0.05) decrease in the level of hyperglycemia, which was accompanied by a decrease in the severity of blood base deficiency (increase in BE to –3.52±1.2 mmol/l,
p
<0.05) and a tendency towards normalization of the studied ENMG parameters.
No significant changes in the severity of pain syndrome or blood acidity levels were recorded. However, by the end of the observation, the vast majority of patients noted a significant improvement in the quality of life compared to its initial level, mainly due to the psychological component ( p
<0.05). Positive changes were associated with a decrease in hyperglycemia due to better control of blood glucose concentrations and increased compliance with drug treatment for both diabetes mellitus and DPN.
In subgroup IIb, by the end of the study there was a significant ( p
<0.05) improvement in all studied parameters with the exception of blood pH, which remained virtually unchanged compared to the initial value.
A significant decrease in the level of glucose in the blood plasma was accompanied by a decrease in the severity of pain according to the NRS scale to the degree of mild algic syndrome (3.6±1.8 points, p
<0.05), an increase in the BE value to –1.7±1.3 (
p
<0.05), which indicated the relief of metabolic blood acidosis.
According to ENMG data of the nerves of the lower extremities, in patients of subgroup IIb, 30 days after the start of therapy, signs of a significant improvement in neural conduction (increased SPI eff and SPI aff values) and neuromuscular transmission (increased amplitude of the M-response and decreased its latency) were observed (Table 2)
.
Patients noted that the treatment significantly improved their physical, psychological condition and overall quality of life ( p
<0.05). During the observation period, no significant side effects were recorded in all study groups, which indicates that the drugs were well tolerated and there was no negative interaction between them.
Discussion
The assessment of the metabolic effect of rheosorbilact in DE and DPN is due to the common pathogenesis (impaired microcirculation) of these diseases (acidosis, oxidative stress, decreased mitochondrial activity, etc.). The established effectiveness of rheosorbilact as part of complex therapy for patients with DE and DPN is due to the metabolic effect of the drug. In particular, the study revealed the ability of rheosorbilact to eliminate metabolic acidosis - a significant decrease in the severity of blood acidosis was observed due to a significant restoration of BE without pronounced changes in blood pH.
It has been shown that the presence of sorbitol in the sciatic nerve and spinal cord [5] reduces the consumption of vitamins in the nervous system and promotes their more economical use. Sorbitol not only reduces intracranial pressure, but also improves blood circulation in the brain [19]. This allows us to recommend its use for cerebral edema, subdural hematoma, and stroke [4, 7].
An analysis of the effectiveness of therapy for patients with DPN showed that the use of rheosorbilact reduced the severity of pain, improved neural conduction and neuromuscular transmission. This circumstance emphasizes the advisability of systemic therapy for DPN. Treatment with rheosorbilact significantly improved the physical, psychological state and quality of life of patients. Thus, rheosorbilact has a number of therapeutic properties that determine the advisability of its use in various neurological diseases.
Weight changes due to metabolic disorders
An important condition in the treatment of obesity is the establishment of the very causes of the disease and excess weight. Before losing weight, metabolic disorders are first eliminated. These two phenomena are closely interrelated; in this case, it is better to consult a doctor.
The patient is prescribed laboratory tests of blood, urine, and other tests, and based on the results, corrective therapy is recommended.
- Medicines for disorders of lipoprotein metabolism with the addition of drugs that affect appetite, as well as enterosorbents.
- Special complexes for replenishing the deficiency of vitamins, micro- and macroelements in the form of tablets, dragees and solutions.
Modern single-dose medications and complex medications allow you to maintain your body in ideal shape and prevent the occurrence of failures and deficiency conditions.
Journal "Arterial Hypertension" 6 (26) 2012
Diseases of the circulatory system still remain the main cause of death in the developed countries of the world, including Ukraine. Despite the fact that in the USA, Great Britain and Canada, heart and vascular diseases are also the main cause of death, mortality from these diseases in Ukraine is 2–4 times higher than in other countries of the world. Every year in Ukraine, about 400 thousand people die from cardiovascular diseases (CVDs). These diseases cause 66.3% of deaths in our country. And if in the countries of Western Europe and North America there is an annual decrease in mortality and disability from CVDs, in our country there was a clear increase until 2008, and only in recent years has there been a downward trend. Despite the successes achieved in the treatment of CVD, about a million Ukrainians died from heart attacks, strokes and other cardiovascular diseases in 2011–2012 alone [10, 11, 13].
According to a number of authors, the leading place in the structure of mortality from CVD is occupied by coronary heart disease (CHD) and cerebral stroke, which, as a rule, develop against the background of arterial hypertension (AH), since high blood pressure (BP) increases the risk of death from CHD in 3 times, and from a stroke - 6 times. Despite the emergence of modern antianginal and antihypertensive drugs, the constant improvement of their pharmacokinetics and pharmacodynamics, the effectiveness of traditional drugs remains insufficient even with adequate regular therapy. Therefore, the problem of increasing the effectiveness of treatment of chronic diseases of the cardiovascular system, and primarily IHD and hypertension, remains very relevant [21, 23].
The modern strategy for providing care to patients with coronary artery disease and hypertension, firstly, involves the prescription of drugs whose action is aimed at improving the prognosis in this category of patients (antiplatelet and lipid-lowering drugs, angiotensin-converting enzyme inhibitors and beta-blockers). Secondly, an equally important aspect in the treatment of patients with angina pectoris is to improve their quality of life, which is achieved by the use of antianginal agents such as nitrates, calcium antagonists, beta-blockers and sinus node If channel inhibitors [6]. Considering the fact that the formation of morphofunctional changes in the myocardium and vascular bed is based on a violation of intracellular energy metabolism caused by its hypoxia due to disruption of coronary blood flow, the use of hemodynamic drugs (beta-blockers, calcium antagonists, nitrates) should fully optimize the relationship between the needs of the heart muscles in oxygen and its delivery. However, as the results of a number of studies show, these drugs do not always effectively control the symptoms of the disease, even when used in rational combinations [15, 20]. This is probably due to the fact that the possibilities of therapy are limited by the functioning conditions of the myocardium during ischemia, the presence of other adaptive and maladaptive processes that have a significant impact on cardiomyocytes and the myocardium as a whole [31]. In addition, the traditional hemodynamic approach to the treatment of patients with stable angina often does not satisfy either the doctor or the patients themselves: more than 60% of patients with coronary artery disease rate their quality of life as unsatisfactory or poor, and half of the patients experience resting angina attacks at least twice a week [19].
Therefore, at present, there is a need to use fundamentally new ways in the treatment of CVD in connection with the understanding of the essence of the disorders occurring in the metabolism of the cardiomyocyte during hypoxia, the formation of new ideas about the pathogenesis of IHD, and the emergence of new adaptive ischemic syndromes (stunning, hibernation and preconditioning of the myocardium). One of the directions of medicinal effects on ischemic myocardium has become the use of myocardial cytoprotectors - drugs that successfully eliminate disturbances in cellular metabolism, ion homeostasis and the functions of cardiomyocyte membranes, thereby preventing the development of irreversible processes in the myocardium. In modern literature, the term “myocardial cytoprotectors” refers to drugs of various chemical classes, the action of which is not associated with a hemodynamic effect, but is mediated by optimizing the processes of energy formation and consumption, correcting the function of the respiratory chain, normalizing the balance between the intensity of free radical oxidation and antioxidant protection, as well as direct effect on cardiomyocytes, which ultimately promotes their survival under ischemic conditions and prevents the formation of “myocardial metabolic remodeling” (the term was proposed by M. van Bilsen et al. in 2004 to designate pathological changes mediated by excess activation of fatty acids in the cardiomyocyte) [ 43].
The history of the emergence of metabolic drugs used for the treatment of coronary artery disease begins with the appearance of a glucose-insulin-potassium mixture, which was first studied by D. SodiPallaris et al. in 1962 and proved its positive effect on the early survival of patients with acute myocardial infarction [41]. Further studies demonstrated a decrease in the release of free fatty acids (FFA) by adipocytes when using a glucose-insulin-potassium mixture, which led to a decrease in their concentration in the area of ischemic myocardium. In the 70–80s of the twentieth century. drugs such as inosine and ATP began to be widely introduced into practice. However, their use did not have a significant effect on improving the condition of patients with either coronary artery disease or hypertension. There is an urgent need to search for other approaches to metabolic therapy of IHD and hypertension. The data obtained in subsequent studies led to the conclusion that significant activation of glucose oxidation can be achieved by blocking FFA oxidation [19, 26, 35].
Today, therapy with metabolic drugs has rightfully taken its place in treatment regimens for CVD and has been included in international recommendations for the treatment of coronary artery disease. However, it should be noted that in this case we are not talking about replacing the hemodynamic approach with a metabolic one, but about a complementary combination of two effects, which are based on different mechanisms of drug action [12, 16].
What requirements must modern metabolic therapy in cardiology meet? Firstly, drugs with metabolic activity must have an evidence base regarding anti-ischemic effectiveness according to the clinical picture, electrocardiography (ECG), stress test parameters, 24-hour ECG monitoring and, most importantly, strong arguments in favor of limiting the size of necrosis during myocardial infarction, proven in experiment and in the clinic. Secondly, they must be characterized by the absence of hemodynamic effects - influence on heart rate, myocardial contractility, blood pressure and other parameters. Finally, an ideal cardiometabolic drug should improve the long-term prognosis of the disease, be well tolerated, and have minimal side effects.
In modern experimental studies, a direct cardioprotective mechanism of action has been established in almost 2000 molecules. However, only a few drugs with metabolic properties are currently used in real clinical practice. The group of cardiometabolic protectors includes drugs that can, on the one hand, positively influence cellular metabolism, ion homeostasis, the structure and function of cell membranes, and, on the other hand, prevent the development of their damage and reperfusion. There is no unified classification of cardiocytoprotectors. One of the latest presented in the medical literature is the classification proposed by V.P. Mikhin (2011), built on the basis of the localization of the pharmacological effect of the drug [14].
Classification of cardiocytoprotectors by localization of pharmacological effect
1. Intramitochondrial cytoprotectors:
1.1. Inhibition of fatty acid oxidation:
- suppression of beta-oxidation of fatty acids (trimetazidine);
- suppression of the transport of fatty acids into mitochondria (Mildronate);
1.2. Direct stimulation of glucose oxidation (2ethyl6methyl3oxypyridine succinate);
1.3. Stimulation of the cytochrome chain (coenzyme Q10).
2. Transport of energy substrate into mitochondria (phosphocreatine, glucose-insulin mixture, succinic acid).
3. Stimulation of anaerobic glycolysis (thiatriazoline) - little developed and ineffective.
4. Antioxidants and mitochondrial cytoprotectors with antioxidant properties.
The most physiological inhibitors of fatty acid oxidation are pFOX inhibitors (partial inhibitors of fatty acid oxidation). One of the most widely used metabolic drugs in cardiological practice is trimetazidine, the basis of which is the blockade of b-oxidation of free fatty acids in mitochondria under ischemic conditions, resulting in inhibition of ATP synthesis from free fatty acids. Therefore, the main source of energy for ATP synthesis is glucose, the oxidation of which to carbon dioxide and water requires 30% less oxygen (per ATP molecule) than for the oxidation of fatty acids, which ultimately leads to significant savings in oxygen for ATP synthesis inside mitochondria [3, 36]. To date, a number of studies have shown the positive effect of trimetazidine on the pathological cascade of disorders that develop during myocardial ischemia. Thus, the use of trimetazidine prevents the depletion of energy sources (in particular, glycogen) in the heart muscle and reduces the content of sodium and calcium ions in cardiomyocytes [33, 37, 38]. Trimetazidine reduces the passive permeability of membranes and increases their resistance to hypoxic and mechanical damage. Under the influence of the drug, there is a decrease in the release of enzymes that damage cardiomyocytes, such as creatine phosphokinase and lactate dehydrogenase [27, 30].
Another representative of this group is Mildronate, which, unlike trimetazidine, reduces the rate of carnitine biosynthesis from its precursor, gammabutyrobetaine. This results in a slowdown in carnitine-mediated transport of long-chain fatty acids across mitochondrial membranes without affecting the metabolism of short-chain fatty acids. This turns on an alternative energy production system - glucose oxidation, which more efficiently uses oxygen for ATP synthesis. The advantage of Mildronate is that when taken in the mitochondria, the concentration of under-oxidized intermediate products of fatty acid metabolism does not increase, which, in turn, can serve as a source of the formation of toxic lipoperoxides as a result of activation of free radical processes during myocardial ischemia and reperfusion. In addition, the accumulation of gammabutyrobetaine stimulates the biosynthesis of nitric oxide, which leads to the normalization of the functional state of the endothelium, a decrease in platelet aggregation and, ultimately, to the normalization of vascular tone. However, we cannot exclude another mechanism for increasing the formation of nitric oxide during the use of Mildronate - a decrease in the intensity of its inactivation by free radicals [7, 18, 28]. A number of scientific studies have shown that the use of Mildronate in patients with stable angina reduced the frequency of angina attacks and the average daily consumption of short-acting nitrates, while at the same time there was an increase in exercise tolerance [8]. The therapeutic and protective effects of Mildronate are realized due to its effect on the metabolic links of the energy chain, which ensures the full functioning of the cell under ischemic conditions. These effects are achieved by reducing the intensity of fatty acid oxidation under ischemic conditions (energy saving), activating glycolysis for energy production, pharmacological training (preconditioning), inducing nitric oxide biosynthesis, and reducing peripheral vascular resistance [17].
Thus, Mildronate, due to the unique features of its mechanism of action, is the drug of choice among other cardiometabolic drugs for the treatment of patients with chronic forms of coronary artery disease, chronic heart failure of ischemic origin, as well as for the correction of metabolic disorders of target organs in hypertension [29, 32, 39, 40 ]. Positioning the mechanism of action of Mildronate on the clinic, several important points can be highlighted: firstly, the administration of the drug already at the initial manifestations of coronary artery disease makes it possible to protect the myocardium from ischemia and prevent the worsening of cardiac pathology, since metabolic disorders in the myocardium begin much earlier than the clinical picture of angina pectoris develops. Secondly, the addition of Mildronate to standard antianginal therapy leads to a significant reduction in the number of angina attacks, a decrease in the daily requirement for nitroglycerin, an increase in exercise tolerance, a decrease in functional class and, ultimately, an improvement in the quality of life of patients. Thirdly, in acute myocardial ischemia, the use of Mildronate leads to a limitation of the necrosis zone by 30%, in acute myocardial infarction - to a decrease in metabolic changes, and with reperfusion - to the restoration of cardiac function and a decrease in the frequency of ventricular fibrillation.
The effectiveness and safety of the original drug Mildronate for ischemic heart disease and hypertension has been proven in numerous clinical studies that meet the requirements of evidence-based medicine. Thus, a comparative assessment of the effectiveness of Mildronate in patients with coronary artery disease with stable angina showed that the addition of Mildronate to traditional therapy for chronic ischemic heart disease, which included aspirin, statins, selective beta-blockers and long-acting nitrates (patients received it at least 4 months before inclusion in the study and continued to receive in constant daily doses during observation), allowed to significantly reduce the frequency of angina attacks and reduce the need for short-acting nitrates [22, 25]. At the same time, some studies clearly showed a decrease in the frequency of anginal attacks and an increase in the need for sublingual nitrates while taking Mildronate (doses of Mildronate were estimated at 500 mg/day and 1000 mg/day) [2]. Another open-label controlled study examined the effect of Mildronate on oxidative processes and endothelial function in elderly patients with coronary artery disease. When taking basic drugs in combination with Mildronate (500 mg per day) for 12 weeks, there was a decrease in the initial level of lipid peroxidation products by an average of 33% and an increase in the resistance of low-density lipoproteins to oxidation by 26%. In addition, patients experienced an increase in the level of nitric oxide metabolites in the blood (on average 1.4 times) compared to the levels before taking the drug.
Of particular interest are the results of the international multicenter, randomized, double-blind, placebo-controlled clinical trial MILSS II, which demonstrated that taking Mildronate in the treatment of stable angina in combination with standard therapy leads to a significant improvement in the patient’s condition and an increase in the patient’s quality of life. The purpose of the study was to evaluate the effectiveness and safety of Mildronate therapy at a dose of 1000 mg per day against the background of standard therapy in patients with stable angina. The results of the study showed that in the group of patients taking Mildronate, the duration of functional activity (FL) increased by 10%, while in the placebo group it increased by only 2.4%. After 12 months of treatment, the difference in the duration of physical exercise between the groups was 13% in favor of the group of patients taking Mildronate (p = 0.009). It should be noted that in the placebo group, the duration of physical activity by the 12th month of therapy was 2.1% lower compared to the indicator at the 6th month of treatment. Before the start of therapy, the average time for the onset of ST segment depression of 1 mm or more in the group of patients taking Mildronate was 425.63 ± 160.97 s, while in the placebo group it was 398.98 ± 145.75 s (differences between groups are statistically insignificant, p = 0.185). After 12 months of treatment, this indicator in the active therapy group increased to 483.83 ± 193.99 s, while in the placebo group it increased to 425.98 ± 159.12 s (p = 0.01). The results obtained led to the conclusion that 12-month therapy with mildronate increased the duration of physical exercise before the onset of ST segment depression by 1 mm by 13.6% compared to baseline values. The difference in indicators between the study groups at the 12th month of treatment was 13.9% in favor of the Mildronate group. Thus, the results of the MILSS II study demonstrated that the addition of Mildronate to standard therapy for coronary artery disease increases patients’ tolerance to exercise, increases the level of maximum exercise achieved, the duration of exercise before the onset of an attack of angina and ST segment depression, and also improves the quality of life of patients [5].
A special place in the study of the effectiveness of cardioprotectors in coronary artery disease is given to their use in coronary angioplasty. Percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) are associated with the development of complications from the cardiovascular system, which include myocardial dysfunction with the development of “stunned myocardium” with impaired local contractility of the left ventricular myocardium, hemodynamic disorders and the appearance of various arrhythmias [34 ]. According to modern concepts, ischemic and reperfusion changes in the myocardium, including during coronary revascularization, develop as a result of metabolic disorders of cardiomyocytes [42]. The effectiveness of the use of Mildronate for the correction of the above-described pathological changes was confirmed by the results of a clinical study conducted at the State Educational Institution of Higher Professional Education "Russian State Medical University", which involved 149 patients with stable angina pectoris II-III FC aged from 41 to 75 years. All patients underwent coronary bypass surgery under artificial circulation or percutaneous coronary intervention. In patients of the first group, 10–15 days before the proposed revascularization, Mildronate was added to drug therapy (nitrates, beta-blockers, antiplatelet agents, ACE inhibitors, antiarrhythmics) for three days, then twice a week. The second group (control) did not receive metabolic drugs. On the 2nd–3rd day after CABG, with the use of Mildronate, a 15% decrease in the index of impaired local segmental contractility of the left ventricle (INLS) was found, while in the comparison group the value of INLS decreased by only 3.5%. Before performing balloon angioplasty, as a result of the preoperative use of Mildronate, the INLS decreased by 14%, in the comparison group - by 2.5%. After performing balloon angioplasty in the main group, the SILR decreased by 19.5% from the initial level, and in the comparison group - by 12%. The inclusion of Mildronate in the preoperative preparation allowed immediately after angioplasty to increase the left ventricular ejection fraction by 12%, while no significant change in the left ventricular ejection fraction was recorded in the control group. This study confirmed the ability of Mildronate to reduce the degree of myocardial hibernation in chronic ischemia. The use of Mildronate during coronary angioplasty as part of preoperative and postoperative therapy accelerated the restoration of myocardial contractile function while improving coronary blood flow and thus increased the efficiency of revascularization [4].
Regarding the use of cardioprotectors for hypertension, it should be noted that in recent years a number of studies have been published that present positive results of this group of drugs. Interest in this kind of research is due to the multiorgan nature of target organ damage in arterial hypertension, the leading role in the pathogenesis of which is played by disruption of intracellular energy metabolism and activation of free radical processes. In a clinical study devoted to the comparative assessment of the effectiveness of cardioprotectors in patients with hypertension, patients of the first group were prescribed Mildronate in addition to the antihypertensive drug enalapril, patients of the second group were given trimetazidine, and the third (control) group received monotherapy with enalapril until the end of the study. After 6 months of taking the drugs, all patients experienced a decrease in the level of lipid peroxides in the blood, and in the Mildronate group the level of diene conjugates decreased more significantly (by 31%) than in the comparison groups (about 20%). Against this background, there was an increase in the degree of endothelium-dependent vasodilation during the cuff test, however, in individuals taking Mildronate, the level of endothelium-dependent vasodilation was significantly higher. In addition to the above effects, the use of Mildronate against the background of enalapril enhanced angioprotection (the thickness of the intimamedia complex in the Mildronate group decreased by 16.2%, and in the trimetazidine and enalapril groups - by 9.7 and 9.5%, respectively). And finally, in patients with hypertension, the combination of Mildronate with enalapril enhanced the hypotensive effect of the latter, accelerated the achievement of the target blood pressure level, and contributed to the normalization of the daily blood pressure profile in a greater number of cases than monotherapy with an angiotensin-converting enzyme inhibitor [24].
Thus, the use of Mildronate as part of complex therapy with basic antihypertensive drugs allows its use as a means for secondary prevention of hypertension, progression of target organ damage and the development of associated diseases.
So, to summarize the above, we can conclude that modern cardiocytoprotectors are a new evidence-based direction in the treatment of cardiovascular diseases. Due to the short time of their study, there is no serious evidence base for their effect on survival and mortality in patients with CVD. However, the clinical data obtained to date on increasing the effectiveness of treatment of patients with coronary heart disease and arterial hypertension indicate the prospects of their use in combination therapy of patients with cardiovascular pathology.