Atherosclerosis is a common chronic artery disease in older people. It occurs due to a violation of fat and protein metabolism, as a result of which cholesterol is deposited in the vessels. Plaques close the lumen in the arteries, which leads to their deformation and blockage. Atherosclerosis of blood vessels without treatment leads to coronary heart disease.
Elderly people need help with atherosclerosis. The diagnosis is quite serious, so a person in old age requires appropriate care, regular examinations, and monitoring the intake of necessary medications.
What people are at risk and what triggers the development of this disease?
- Smoking.
- Diabetes.
- Hypertension.
- Passive lifestyle.
- Stress.
Rehabilitation for atherosclerosis
If you do not have time to monitor the health of an elderly person around the clock, we advise you to provide him with proper care and register him in the Parents' Estate nursing home in Irkutsk. Our specialists will be able to provide the necessary comprehensive assistance to people suffering from atherosclerosis and other cardiovascular diseases, and will provide round-the-clock monitoring and careful care for the elderly.
The staff of the boarding house for the elderly in Irkutsk has extensive experience working with pensioners with various diseases. They will be able to help people with atherosclerosis recover, take prescribed medications on time, and attend physical education classes. Rehabilitation after atherosclerosis and exercises for physical therapy are selected for each patient strictly individually. We will be able to provide our patients with the necessary assistance during the rehabilitation period and eliminate the risks of complications. Most often, at the age of 60+, atherosclerosis of the lower extremities develops. The disease leads to vascular inconductivity and tissue necrosis. You can get rid of thrombosis not only with medications, but also with surgery. In our boarding house, nurses provide assistance for atherosclerosis of the lower extremities, as well as for elderly people after surgery.
Nursing care for atherosclerosis
How can our nurses and nurses help a sick elderly person? Competent staff of the boarding house carefully ensure that the patient follows all the recommendations of the attending physician, takes medications on time and reports the first symptoms of illness. Naturally, atherosclerosis has its own peculiarities of nursing care, which our employees are aware of.
Authors):
Associate Professor V.K. Milkamanovich
Medical institution:
Belarusian State University Atherosclerosis is a systemic, irreversible chronic disease in which degenerative-inflammatory transformations (transformations) of the inner and middle layers of large and medium-sized arteries develop (Fig. 1). The disease process is localized in areas of focal or global dysfunction (dysplasia) of the connective tissue of elastic and muscular vessels as a result of disturbances in biochemical, immunological and molecular genetic processes in the body.\
Rice. 1. Healthy artery.
Usually the thoracic and abdominal aorta, coronary, mesenteric, renal vessels, as well as arteries of the lower extremities and brain are affected. The disease has a slow wave-like course; it can occur in childhood and accelerate the pace of its development as a person grows and ages.
Atherosclerosis is a global medical and social problem of humanity among representatives of different races, which is a very common cause of disability and premature death. Currently, mortality from diseases associated with atherosclerosis averages 750–800 per 100,000 population, which significantly exceeds that from cancer. Among the reasons for the high prevalence of atherosclerosis, a significant place is occupied by low atherogenic alertness and insufficient education of the population.
Atherosclerosis in its clinical manifestations is usually detected at 40–45 years of age. In men, the development of atherosclerosis occurs 10–15 years earlier and is 4 times higher than the incidence rate of atherosclerosis among women. After 50–55 years, the incidence of atherosclerosis among women and men levels off. This is explained by a decrease in estrogen production in women during menopause. Even domesticated animals often suffer from atherosclerosis when their diet and lifestyle change; it can be modeled quite simply in laboratory conditions.
The causes of primary (initial) damage to the endothelium of the main arteries during atherosclerosis remain unclear, however, a number of the most dangerous factors have now been identified, in the presence of which it develops earlier and progresses faster. These are dyslipidemia, chronic autoimmune inflammation, arterial hypertension and lack of adherence to treatment for existing atherosclerosis.
Dyslipidemia (dyslipoproteinemia) is a disorder of fat metabolism in the body, manifested by an increased content of total cholesterol (TC), triglycerides (TG) and lipoproteins. A normal level of total cholesterol in the blood is observed only in 38–42% of men and 36–40% of women. In other words, about 60% of the adult population have its concentration in the blood above the normal level, which indicates a high risk of developing atherosclerosis.
High-density lipoproteins (HDL) transport excess free cholesterol from tissues to the liver for processing and elimination. A sufficient level of HDL in the blood is characteristic of a healthy body, so these lipoproteins are often called good. High molecular weight lipoproteins are highly soluble and do not tend to precipitate cholesterol and thereby protect blood vessels from atherosclerotic changes (that is, they are not atherogenic).
Low-density lipoproteins (LDL) are designed to transport cholesterol from the liver to tissues. Very low-density lipoproteins (VLDL) transport endogenous cholesterol and TG in the body. It is believed that LDL and VLDL are atherogenic lipoproteins, the so-called bad ones. The higher their level, and the higher their cholesterol content, the greater the risk of atherosclerosis progression.
Atherogenic disorders of lipid metabolism include:
- increase in blood cholesterol level >5 mmol/l;
- increase in TG level >1.7 mmol/l;
- decrease in HDL level <0.9 mmol/l.
With chronic autoimmune inflammation in the body (for example, rheumatoid arthritis, psoriasis, autoimmune thyroiditis, etc.), inflammatory factors (proinflammatory cytokines, macrophages, monocytes, T-lymphocytes, etc.) damage the endothelial lining of the arteries and the associated platelet activation. In addition, induction by systemic inflammatory factors entering the blood from atherosclerotic formations with an already formed active inflammatory process is possible.
Under the influence of high blood pressure more than 140/90 mm Hg. Art. (arterial hypertension) the endothelium of the vascular wall can be damaged, and conditions are created for the vascular wall to become saturated with fats. On the other hand, a decrease in the elasticity of the arteries during atherosclerosis helps maintain high blood pressure. A so-called vicious circle is formed.
Lack of adherence to treatment in the presence of morphological signs of atherosclerosis, when the patient requires special medications and medical procedures leads to severe uncontrolled consequences of atherosclerosis.
The presence of even one of the listed risk factors for atherosclerosis increases the mortality rate of men aged 50–69 years by 3.5 times, and the combined effect of several factors – by 5–7 times.
The atherosclerotic process develops in places of primary damage to the endothelium of the main arteries. Blood cells – monocytes and platelets – play an important role in atherogenesis. In the presence of hyperlipidemia and disruption of the integrity of the endothelial barrier, monocytes penetrate the cell and rush to peroxidized lipids. The latter acquire the properties of a foreign element and become toxic. Monocytes are loaded with absorbed lipids and turn into macrophages, “scavenger cells”, “cleaner cells”. Macrophages accumulate at the cell membrane in the form of foam cells filled with cholesterol.
At the same time, in areas of endothelial damage, adhesion (sticking) of platelets occurs with their aggregation, disintegration of part of the platelets, which leads to the release of various active substances from platelets, in particular the so-called growth factor of smooth muscle cells, as well as serotonin, thromboxane, etc. As a result, proliferation of smooth muscle cells and a number of other processes occur in the walls of arteries.
This entire complex of interaction of lipids with macrophages, smooth muscle cells, and platelet aggregates leads to the appearance of atheromatous lipid strips and yellowish plaques filled with liquid lipids in the form of a mushy mass (Fig. 2).
Rice. 2. Atheromatous plaque protruding into the lumen of the artery.
Stripes and plaques are localized in areas of branching, narrowing and tortuosity of blood vessels, where the blood flow is not linear and turbulent flows are formed, especially in conditions of constantly elevated blood pressure. Over time, some of them dissolve, while others, on the contrary, grow, occupying an increasingly larger area. In this case, the damaged artery wall around these atherosclerotic formations ulcerates, becomes inflamed and thromboses.
Subsequent proliferation of fibrous tissue (sclerosis) and calcification lead to a decrease in the elasticity of the vascular wall, steadily progressive deformation and narrowing of the lumen, up to complete desolation (Fig. 3).
Rice. 3. Narrowing of the artery lumen.
The passage of blood through the affected vessel decreases significantly or stops, and the degree of reduction in blood flow is usually proportional to the degree of stenosis (narrowing) of the vessel. A chronic, slowly increasing insufficiency of blood supply to the organ fed through the affected artery is formed.
In addition, acute blockage of the arterial lumen is possible either with a thrombus, or (much less often) with the contents of a disintegrated “young” atheromatous plaque, or both at the same time (Fig. 4), which leads to serious vascular disasters (the formation of foci of necrosis or gangrene in the fed artery of an organ or part of the body).
Atherosclerotic arterial disease is always a solid foundation for many disabling cardiovascular diseases (CVDs): coronary heart disease, ischemic stroke, obliterating lesions of the lower extremities, chronic occlusion of mesenteric vessels, etc. There is a high probability of developing these CVDs in persons with atherosclerosis, if present and exposed to such unfavorable medical and social factors as:
- social deprivation is a state of social discomfort accompanied by the individual’s awareness of the gap between expectations and reality; usually formed in the conditions of loneliness of an urbanized society, social inequality and unfavorable lifestyle of marginal and socially vulnerable groups of the population, people with deviant behavior, pensioners, the unemployed, the disabled, prisoners, etc.;
- psychosocial stress (excessive emotional stress and negative personality traits);
- smoking - its effect on the development of atherosclerosis is explained by the negative effects of nicotine and tar on blood vessels; Smoking also prevents sufficient oxygen from entering the tissues of the human body;
- physical inactivity (lack of physical activity), which contributes to impaired fat metabolism, the development of obesity and diabetes;
- obesity (waist circumference in men >94 cm, in women >80 cm) and diabetes mellitus (fasting blood glucose >6 mmol/l), in which the likelihood of developing atherosclerosis is increased by 5–7 times;
- tendency to overeat, eating large amounts of animal fats, which significantly accelerates the development of atherosclerotic changes in blood vessels;
- a family history of atherosclerosis – the disease develops in patients whose relatives suffer from this disease; atherosclerosis is not a hereditary disease, and its occurrence in persons whose parents suffered from atherosclerosis is not at all necessary, but a predisposition to atherosclerosis can be inherited; it has been proven that a predisposition to atherosclerosis contributes to the early (before 50 years) development of the disease, while after 50 years genetic factors do not play a leading role in its development;
- burdened hereditary history of CVD - the development of a disease of the circulatory system in close relatives: in men under 55 years of age, in women under 60 years of age;
- obstructive sleep apnea syndrome - this disorder manifests itself in the occurrence of pauses in breathing or shallow breaths during sleep; if this is not brought under control, the risk of life-threatening complications of atherosclerosis in a sick person increases - ischemic stroke, angina pectoris, myocardial infarction, hypertensive crisis, etc.;
- chronically ongoing infections (herpes simplex and human immunodeficiency viruses, cytomegalovirus, chlamydial infection, etc.) and intoxications, in which infectious and toxic agents have a damaging effect on the vascular walls, contributing to their atherosclerotic changes.
The main insidiousness of the disease is that the first stages of vascular atherosclerosis are asymptomatic. For a long time, most people with atherosclerosis may not even be aware of their illness. A clear clinical picture develops only after the occurrence of complications such as angina pectoris, myocardial infarction, cerebral stroke, chronic cerebrovascular insufficiency, intermittent claudication, etc.
There are no symptoms specific to atherosclerosis itself. However, there are general signs of ill health, which are mainly associated with various metabolic disorders in atherosclerosis. People with atherosclerosis, as a rule, look older than their years: early gray hair, hair loss, dry and wrinkled skin, xanthelasmas and xanthomas (especially on the upper eyelids), etc. They complain of fatigue, decreased performance, chronic fatigue, shortness of breath , interruptions in heart function, increased heart rate, etc.
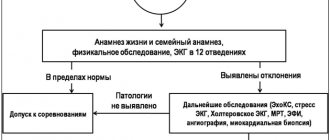
Early detection of atherosclerosis and unfavorable factors contributing to its development in a sick person is especially important, since at the initial stage the harmful effects of atherogenesis can be significantly weakened, slowed down, or even completely eliminated.
For atherosclerosis, the diagnosis is based on taking into account the above CVD risk factors, especially their combinations, clinical symptoms of organ damage, data from laboratory and instrumental studies, as well as after consultation with specialists.
The first clinical manifestations of atherosclerosis (including acute atherothrombosis) appear when more than 50–70% of the vessel lumen is stenotic. In each specific case, the complaints of a sick person depend on the atherosclerotic lesion of certain vessels and the severity of the process:
pain in the heart area - with atherosclerosis of the thoracic aorta and coronary arteries;
attacks of abdominal pain – with atherosclerosis of the abdominal aorta;
headaches, dizziness, paresthesia, pain in the arms, paresis - with atherosclerosis of the carotid arteries;
memory impairment, sleep disturbance, irritability under slight psychological stress, frequent mood swings, tearfulness - with atherosclerosis of the cerebral arteries;
bloating, pressure in the epigastric region and right hypochondrium, belching, periodic abdominal pain, etc. - with atherosclerosis of the arteries of the abdominal organs;
pain in one or both legs when walking, stopping or decreasing with rest - with atherosclerosis of the arteries of the extremities.
Most often, sick people first consult a doctor only after the symptoms of the disease arising from vascular atherosclerosis begin to significantly complicate their lives (inability to climb stairs without severe shortness of breath, tachycardia and a feeling of lack of air at rest, inability to move independently from -for pain in the legs, etc.).
Assessment of lipid metabolism is a mandatory element of the biochemical examination of any patient at high risk or with the presence of atherosclerosis and its main clinical manifestations. It includes determination of the level of total cholesterol, cholesterol associated with LDL (LDL-C, beta-cholesterol), cholesterol associated with VLDL (C-VLDL, pre-beta-cholesterol), cholesterol associated with HDL (HDL-C, alpha-cholesterol) , as well as determination of beta-lipoproteins and TG.
The normal level of total cholesterol should not exceed 5.0–5.2 mmol/l, LDL cholesterol - up to 3.3 mmol/l, HDL cholesterol - 0.9 mmol/l, TG - up to 1.7 mmol/l. The levels of total cholesterol, LDL and HDL have similar values in blood plasma taken on an empty stomach and taken after a meal, the difference is no more than 0.3 mmol/l.
Classification of conditional levels of total cholesterol in the blood:
- optimal – 5 mmol/l or less;
- moderately elevated – 5–6 mmol/l;
- dangerously elevated – 7.8 mmol/l.
The most informative and integral indicator reflecting the state of lipid metabolism is the cholesterol atherogenicity coefficient.
The normal value of the atherogenic coefficient is up to 2.5–3.0. Its increase is an unfavorable indicator, indicating the possibility of progression of atherosclerosis.
To reliably confirm atherosclerosis, it is necessary to detect its morphological signs using ECG, echocardiography, ultrasound of the pelvic and abdominal organs, Dopplerography of the vessels of the head, neck, legs, renal arteries, etc. An MRI may be recommended.
If necessary, consultation with specialists is possible:
- ophthalmologist (assessment of the condition of the fundus);
- neurologist (detection of neurological disorders);
- angiosurgeon (for severe lesions, to determine the need for surgical treatment) and a neurosurgeon (if intracranial arteries are affected);
- cardiologist (to select therapy or correct already prescribed treatment);
- endocrinologist (when identifying background endocrinological pathologies);
- hematologist (to correct coagulogram parameters and prevent thrombus formation through the selection of antiplatelet therapy).
The main tasks of medical and social rehabilitation of patients with atherosclerosis and their solution.
Unfortunately, there are no guaranteed methods of getting rid of atherosclerosis. However, modern approaches to medical and social adaptation and rehabilitation of a sick person with atherosclerosis can significantly improve the quality and duration of his life, as well as functional activity.
Firstly, to prevent the occurrence of the disease and its development, you need to make appropriate adjustments to your usual lifestyle:
- include foods low in cholesterol and salt in your diet (mainly whole grains, vegetables, fruits, fish);
- carry out all necessary measures to prevent and combat existing chronic autoimmune diseases;
- Regularly monitor blood pressure levels; it should always be less than 140/90 mmHg. Art., if necessary, carry out adequate antihypertensive therapy;
in the presence of atherosclerosis and the risk of its dangerous complications, maintain adherence to anti-sclerotic drug therapy. To do this you need:
– master the technique of self-control of your disease and promptly recognize the beginning deterioration of your condition;
– have a good knowledge of the scheme (protocol) and all components of drug therapy and skillfully use prescribed medications.
Secondly, to protect against possible life-threatening cardiovascular consequences of atherosclerosis, it is necessary to minimize the influence of unfavorable medical and social factors:
influence social isolation and mental health disorders (especially depression);
completely stop smoking tobacco in any form;
minimize and eliminate general physical detraining, to do this, provide 2.5–5 hours of moderate physical activity per week or 30–60 minutes during the day;
maintain body weight within normal limits; body mass index (BMI) should be 20–25 kg/m2, waist circumference <94 cm in men and <80 cm in women;
regularly monitor fasting blood glucose levels; it should always be 3.33–5.55 mmol/l, provided that the measurement was taken on an empty stomach; the blood level of glycated hemoglobin (HbAlc), which is a compound of hemoglobin with glucose, must be less than 7%; if necessary, carry out adequate sugar-lowering therapy;
if you have a family predisposition to atherosclerosis, make every effort to implement measures to prevent it in order to counteract the implementation of an inherited predisposition;
implement timely measures to prevent and combat existing chronic infections and intoxications.
It is necessary to take into account that all of the indicated approaches and tasks of medical and social adaptation and rehabilitation must be agreed upon with the attending physician.
It is very important to form in the patient a clear understanding of atherosclerosis as a dangerous disease, the causes of its occurrence and the mechanisms of development.
It is necessary to convince the ward of the advisability of overcoming erroneous behavioral stereotypes and develop in him an attitude towards combating risk factors for life-threatening CVDs. Many of them suffer from arterial hypertension in combination with hypercholesterolemia and excess body weight, smoke a lot, lead a sedentary lifestyle, etc.
The level of each of the existing risk factors in itself can be increased moderately, but their combination always gives grounds to classify sick people with atherosclerosis as a high-risk group. They need regular examinations, recommendations for lifestyle changes (quitting smoking and alcohol), constant monitoring in terms of compliance with dietary recommendations, weight loss, physical activity, drug treatment, etc.
The nurse should give all recommendations regarding the patient’s lifestyle and health status only in the form of wishes and advice, and not any instructions or orders.
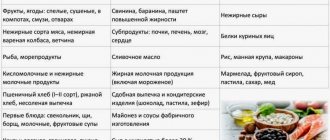
Dietary recommendations to reduce LDL levels and improve lipid profile.
The basis of non-drug treatment of dyslipoproteinemia is a special diet. The nurse should have a list of the main foods that she can recommend to a patient with atherosclerosis to reduce LDL levels and improve the lipid profile (or advise them to limit or eliminate them altogether).
Recommended products must be constantly present in the patient's diet.
Foods that can be eaten in moderation contain polyunsaturated fats or small amounts of saturated fat. They are allowed to be consumed on average no more than 1–3 times a week.
Non-recommended foods contain high amounts of saturated fat. If possible, they should be excluded from the diet.
Fats.
All fats should be limited.
Moderate consumption: sunflower, corn, soybean and olive oils, margarine marked “enriched with polyunsaturated fats”, low-fat sandwich masses.
Not recommended: butter, ghee and coconut oil, lard (rendered pork fat), meat fat, lard, cooking fat, hydrogenated (solid) fats, oils, margarines.
Meat.
Recommended: chicken, turkey, veal, rabbit, game.
Moderate consumption: lean beef, bacon, lean ham, pork, lamb, lean minced meat, good quality cutlets, pate cooked with permitted fat - no more than once a week.
Not recommended: visible fat on meat, fatty pork belly, lamb brisket, flaky bacon, smoked sausages, minced meat containing lard, duck, goose, poultry skin, heavily fried appetizers, pate.
Fish.
Recommended: cod, flounder, haddock, herring, mackerel, sardines, tuna, salmon.
Moderate consumption: fish fried in permitted oil, shellfish, fish pastes prepared with permitted fat - no more than once a week.
Not recommended: fish roe.
Dairy products.
Recommended: skim milk, low-fat cheeses and cottage cheese, cottage cheese, low-fat kefir, yogurt, egg whites.
Moderate consumption: semi-skimmed milk, medium-fat cheeses (less than 30%) - no more than 1 time per week, 1-3 eggs per week.
Not recommended: whole, dry and condensed milk, sour cream, full-fat and processed cheeses of regular fat content, yogurt, kefir.
Soups.
Recommended: clear soups, homemade vegetarian soups.
Moderate consumption: soups from concentrate, meat soups.
Not recommended: soups with fatty broths, puree soups.
Bread, cereals, flour products.
Recommended: wholemeal bread, whole grain dishes, oats, corn, rice, crispbread, oatmeal cookies.
Moderate consumption: white bread, sweet grain dishes, sweet cereals, sweet, semi-sweet and unleavened cookies, muffins, cakes, cookies prepared with the permitted type of margarine or vegetable oil - no more than 2 times a week, homemade snacks prepared with polyunsaturated fats
Not recommended: bread made from premium flour, puff pastries, spicy cheese cookies, cakes, muffins and cookies cooked with saturated fat, dumplings made with lard, pork and beef pies.
Vegetables, fruits, nuts.
Recommended: all fresh and frozen vegetables, peas, beans, sweet corn, all varieties of dried legumes, lentils, boiled potatoes, including in their jackets (possibly with peel), fresh and unsweetened canned fruits, dried fruits, walnuts, chestnuts.
Moderate consumption: dried and fried potatoes cooked in vegetable oil - once every 2 weeks, fruits in syrup, hazelnuts, almonds.
Not recommended: dried and fried potatoes cooked in non-recommended fat, coconuts.
Seasonings and sauces.
Recommended: low-fat sauces, herbs, spices, mustard, pepper, vinegar, low-fat gravies, clear marinades.
Moderate consumption: meat and fish pastes, low-calorie sour cream salad dressing, low-calorie mayonnaise, tomato and soy sauce.
Not recommended: sour cream, mayonnaise, sauces with sour cream or processed cheese, sauces based on butter or sour cream.
Sweets.
Recommended: sweeteners, low-fat puddings, jellies, mousses, skim milk puddings.
Moderate consumption: sweet marinades and compotes, jam, marmalade, honey, syrup, marzipans, marshmallows, sugar, sorbitol, glucose, fructose.
Not recommended: puddings cooked with non-recommended fat, chocolate spreads, chocolate candies, chocolate, milk ice cream, coconut sticks.
Beverages.
Recommended: tea, weak coffee, mineral water, sugar-free soft drinks, sugar-free fruit juices, non-alcoholic beer.
Moderate consumption: sweetened soft drinks, low-fat malt drinks, low-fat chocolate, alcoholic beverages.
Not recommended: strong coffee, malt drinks, chocolate.
Recommendations for developing conscious adherence to drug therapy.
The nurse is obliged to inform the sick person and his relatives that modern anti-sclerotic drugs effectively correct lipid metabolism disorders and allow regression of atherosclerosis. As a rule, after about 2 years of active drug treatment, the diameter of the lumen of blood vessels increases. At the same time, clinical improvement is detected much earlier - after 6 weeks. This is due to the restoration of endothelial functions, normalization of vascular tone, as well as improvement of the rheological properties of blood.
Drug therapy is prescribed by the attending physician for persistent dyslipoproteinemia that cannot be corrected by diet. It may consist of lipid-lowering, antioxidant, antiaggregation and other drugs.
Lipid-lowering drugs.
Inhibitors of the enzyme HMC-CoA reductase - statins. This is the basis for the treatment of dyslipidemia at the present stage. Statins are prescribed at night, since cholesterol synthesis occurs mainly at night. The initial dose is increased every 4 weeks if the target level of total cholesterol and plasma LDL cholesterol is not achieved. When prescribing high doses, statins can be taken 2 times - morning and evening. The hypocholesterolemic effect is achieved after 3 days of treatment, the maximum effect is achieved after 4–6 weeks.
Statins are taken orally once a day (in one dose): atorvastatin 10 mg with a gradual increase in the daily dose with an interval of 4 weeks up to 40 mg; lovostatin 10–40 mg; pravastatin 10–40 mg at bedtime; simvastatin 10–40 mg (usually at bedtime); fluvastatin 20–40 mg at bedtime.
Inhibitors of cholesterol absorption in the intestine (ezetimibe). The inhibitory effect of ezetimibe on the absorption of cholesterol and plant sterols occurs due to blocking the exogenous cholesterol transporter localized on the brush border of the small intestinal epithelium.
Nicotinic acid – niacin (2–4 g/day), enduracin (0.5 g/day). The effect of nicotinic acid is manifested in a decrease in the levels of total cholesterol and TG, as well as in an increase in the level of antiatherogenic HDL.
Bile acid sequestrants (resins) – cholestyramine, colestipol, colesevelam, questran, colestimide. The mechanism of action of bile acid sequestrants is to bind bile acids in the intestinal lumen and excrete them with feces. Cholestyramine is available in 4 g packets and is prescribed before meals 2-3 times a day.
Fibric acid derivatives (fibrates and omega-3 polyunsaturated fatty acids (PUFAs). They predominantly reduce TG levels and moderately increase HDL levels.
Fibrates: gemfibrozil orally 1.2 g per day in two doses; fenofibrate orally 200 mg per day in one dose; ciprofibrate orally 100 mg per day in one dose.
PUFA preparations of fish origin – omakor (2–4 g/day), eikonol, maxepa, etc.; soluble fiber preparations – plant cholesterol sorbents (pectins, guare).
Antioxidant drugs.
At the site of arterial damage, the presence of oxidized LDL is characteristic. This implies the need to use antioxidants to inhibit the atherosclerotic process. The group of antioxidant drugs includes tocopheryl acetate (vitamin E), which is prescribed orally at 0.05–0.1 g per day or intramuscularly, bioflavonoids (vitamin P) - rutin, quercetin, etc.
There are known foods rich in antioxidants: dark green, yellow, orange and red vegetables, citrus fruits, strawberries, cherries, etc.
Antiaggregation drugs.
Considering the important role of platelet aggregation in the formation of atherosclerotic plaques and other thromboembolic complications, the prescription of anticoagulants is justified, among which acetylsalicylic acid (aspirin) comes first. For long-term treatment, it is enough to take 80-100 mg of aspirin for 5 days, then take a break for 2 days, after which the cycle is repeated. The minimum but sufficient dose of aspirin ranges from 30–150 mg per day.
References.
1. Krylov V. P. Atherosclerosis: a look at the problem (results of discussion) // Medicine. – 2021. – No. 1. – P. 23–24.
2. Milkamanovich V.K. Gerontology and geriatrics: textbook. allowance. – Minsk, 2010. – 279 p.
3. Milkamanovich V.K. Therapy: textbook. allowance. – Minsk, 2005. – 608 p.
4. Sudzhaeva O. A. What’s new in the treatment of dyslipidemia? // Family doctor. – 2021. – No. 1. – P. 28–39.
5. Khapalyuk A. V. Mechanisms of atherogenesis and statins // General Medicine. – 2013. – No. 2. – P. 31–40.
What does caring for a patient with atherosclerosis include?
- Assistance with hygiene procedures: washing, brushing teeth, bathing, cutting hair and nails.
- If the patient is a bedridden patient, special care is required, including feeding, daily change of linen, diapers, ducks, cleanliness, prevention of bedsores and much more.
- Ironing, washing and regular change of linen and clothes.
- Cleaning and airing rooms.
- Accompaniment for a walk.
- Preparing for the examination.
- Health monitoring.
When caring for a patient with atherosclerosis, psychological assistance and support from boarding house workers is very important. Care, attention and a polite, considerate attitude work wonders. Patients recover quickly, their condition does not worsen, but goes into remission, and their mood returns to normal. Nurses must explain to the patient why it is so important to follow the doctor’s instructions and adhere to the diet. This attitude is the best way to promote recovery.
Possible causes of the disease
It is impossible to name one single reason leading to atherosclerotic restructuring of the artery wall and the formation of atherosclerotic plaques. Most researchers agree with the fact that atherosclerosis is based on a violation of fat metabolism (more precisely, cholesterol esters) at the level of genetic predisposition. Familial hypercholesterolemia (FH) is a known disease. It is an autosomal dominant disorder caused by a decreased rate of clearance of low-density lipoprotein (LDL) from the bloodstream due to mutations in the specific LDL receptor gene.
In patients with FH, there is an increase in the blood level of total cholesterol and cholesterol associated with LDL, and the development of atherosclerotic disease. Moreover, familial hypercholesterolemia is the most common genetic disease due to a mutation of one gene (monogenic disease).
Psychological support
The first days after surgery are the most difficult time.
The patient experiences severe pain, discomfort, and anxiety. A person may have significant fears about restoring organ function and motor activity, especially if the process is difficult. During this period, support, participation, and a friendly attitude are extremely important. The constant presence of a nurse next to the patient, her help and encouraging words will help the patient get rid of unpleasant thoughts and will contribute to his speedy rehabilitation and recovery. In contact with
What is nursing care?
Organizing proper care for a person after surgery is a responsible and difficult task. It is necessary to ensure and maintain sterility in the ward or other room where the patient is located, carry out the necessary medical and hygienic procedures, and provide psychological support.
The main tasks of nursing care include the following activities:
- Preparing the room for the reception of a postoperative patient and maintaining sterility in it. It is necessary to carefully prepare the room - carry out quartzing, ventilation, change bedding.
- Systematic monitoring of the patient. It is required to regularly monitor body temperature, check pulse rate, blood pressure, inquire with the patient about his general health, pain, discomfort, and monitor wound healing. If the patient is unconscious, information about his condition is obtained by measuring physiological parameters and visual examination.
- Wound care. It is necessary to promptly change dressings, drainages, catheters, and treat the wound with antibacterial agents; monitor patient comfort.
- Providing vital functions. The patient should be provided with a food and drinking regime appropriate to his condition, and dynamic control over the excretion of urine and feces should be carried out.
- Carrying out hygiene procedures. From the first day, it is necessary to prevent bedsores, cleanse the skin of contaminants, and sanitize the oral cavity.
- In order to speed up the recovery of the patient, he needs exercise therapy sessions, massage of the back muscles and limbs.
Causes and risk factors
Despite numerous studies, doctors cannot say for sure what provokes atherosclerosis, but there is a direct relationship between a person’s age and the likelihood of getting sick. Risk factors also include:
• unfavorable family history; • prolonged smoking and alcohol abuse; • metabolic disorders (diabetes mellitus, thyroid diseases, etc.); • excess body weight; • sedentary lifestyle; • high blood pressure; • frequent stressful situations, nervous overload; • pathology of the aorta; • gout; • other disorders of the cardiovascular system.
Surgical methods for treating atherosclerosis
- elimination of atherosclerotic plaque by open surgery on the vessel,
- expansion of the lumen of the vessel from the inside using special instruments and installation of a metal frame that prevents further narrowing,
- when the lumen of the vessel is completely closed by a plaque, a bypass operation is performed (a bypass of the blood flow).
Surgical treatment is prescribed when the risk of developing disabling complications without surgery exceeds the development of such complications after surgery.
Why nursing care is needed
Surgical operations affect the functioning of all organs and systems of the body. After they are carried out, the patient is deprived for some time not only of his ability to work, but also of the ability to provide for his own physiological needs. He cannot eat and drink on his own, go to the toilet, take care of hygiene, or even move. At the same time, he requires special conditions of detention, daily monitoring of psychophysiological parameters, medical procedures for treating wounds, sutures, and relieving pain.
If the patient's condition is unstable in the postoperative period, the participation of a nurse is vital. Only a professionally trained person can provide the necessary assistance in an emergency situation.
Nursing care for a postoperative patient will speed up the patient's recovery and return to normal life, and prevent the development of possible complications.
What are the main signs of atherosclerosis?
The disease develops gradually, and at the initial stage it can be confused with the consequences of severe fatigue. A person gets tired quickly, periodically hears tinnitus, and dizziness and headaches may also occur, which gradually disappear. Symptoms intensify as atherosclerotic plaques increase, preventing blood from flowing through the vessels to the brain, internal organs, upper and lower extremities. At the second stage, the patient faces:
1. Insomnia. 2. Memory impairment. 3. Regular migraines. 4. Convulsive syndrome. 5. Substernal pain (with damage to the aorta). 6. Difficulty breathing. 7. Significant decrease in performance. 8. Swelling, numbness of the hands and feet. 9. Stable high blood pressure. 10. Pain in the spine.
If nothing is done, then the old man may develop dementia, spatial and/or temporal disorientation against the background of atherosclerosis. In this state, a person is absolutely helpless and needs constant care and attention. Timely consultation with doctors and monitoring your well-being will help you avoid complications such as stroke, heart attack, and chronic renal failure.
Classification of forms of the disease
Atherosclerosis is a systemic disease that affects all arteries, however, depending on the predominance of the severity of atherosclerosis in a particular group of vessels, it is divided into:
- atherosclerosis of the coronary arteries (causing coronary heart disease and angina, which can result in myocardial infarction),
- atherosclerosis of the brachiocephalic arteries (causing chronic insufficiency of cerebral blood flow, which can result in a stroke),
- atherosclerosis of the aorta, iliac arteries and arteries of the lower extremities (causing intermittent claudication, which can result in gangrene of the lower extremity or fingers),
- atherosclerosis of the visceral branches of the aorta (impaired blood flow in the internal organs, which can result in infarction of the intestine, kidney, etc.),
- multifocal atherosclerosis (damage to several of the above groups of vessels).