What is D-dimer
D-dimer is the part of the protein that remains after the blood clot breaks down. It is a breakdown product of fibrin, the fibers of which form a blood clot. D-dimer consists of two D-particles of fibrinogen contained in blood plasma.
The amount of D-dimer in the blood can be determined using a test. If this indicator is excessively high, then the patient has a high risk of thrombosis.
This analysis is not included in the mandatory laboratory tests. It is prescribed only to those who are at risk for thrombosis.
Decoding the results
Increased D-dimer levels
When the level of D-dimer in the blood increases, it is necessary to search for a probable cause, since some conditions accompanied by an increase in its concentration require immediate medical attention.
An increased level of D-dimer as a physiological norm occurs in old age (after eighty years), as well as during pregnancy (gradually increasing in proportion to the gestational age).
- Outside of pregnancy, a high D-dimer may indicate the presence of thrombosis in the veins or arteries. This is usually accompanied by complaints characteristic of thrombosis (pain in the limb, swelling, redness or pallor) or thromboembolism (shortness of breath, chest pain, hemoptysis). In this case, help must be urgent. But in approximately 20-30% of cases, thrombosis is asymptomatic. In this case, your doctor will help you draw up an examination plan and decide on tactics.
- D-dimer often increases in people suffering from obesity, autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, etc.), as well as liver disease and cancer. In this case, the increase is most likely secondary, and if there are no signs of thrombosis, observation by your doctor is sufficient.
- Often, D-dimer is elevated in older people (also without signs of thrombosis). Prescribing thinning drugs in this situation is not always necessary, since the risk of bleeding must also be taken into account.
- Since D-dimers are breakdown products of already formed blood clots, their concentration may increase after bleeding or during the period of hematoma resorption.
- The most difficult thing to interpret is the increase in D-dimer due to thrombosis during pregnancy. The same level of D-dimer can be observed both in a patient with thrombosis and in a healthy pregnant woman. Therefore, complaints and the likelihood of thrombosis (the degree of risk, which is calculated on a special scale) are always assessed in parallel.
Normal D-dimer levels
A normal test result indicates that the patient is not at risk of thrombosis. However, in rare cases (no more than 2 per hundred) in the presence of thrombosis, the level of D-dimer remains normal. As a rule, this is due either to the very small size of the blood clot, or to improper storage of the material for the study. Thus, the diagnostic value of the D-dimer test is quite high (98%) and allows its active use to exclude the process of thrombus formation.
Low D-dimer levels
A low D-dimer should not be a concern. If the value is below the lower limit (although most laboratories indicate only the upper limit, which is correct), this can reliably indicate only one thing: you definitely do not have thrombosis.
It makes no difference whether to take a D-dimer test before or after taking thinning drugs, since this indicator is cumulative and reflects the activity of the coagulation and anticoagulation systems retrospectively.
What does D-dimer show in a blood test?
A blood test for D-dimer (also called dedimer) shows whether there are small blood clots in the bloodstream. These clots can clog blood vessels and cause life-threatening conditions:
- deep vein thrombosis;
- heart attack;
- stroke;
- pulmonary embolism.
To assess the risk of such serious diseases, doctors prescribe patients to do a D-dimer test.
Blood from a vein is donated on an empty stomach in the morning. You must not eat 8 hours or smoke 2 hours before the test. You are allowed to drink only water; tea, coffee, juices and other drinks, especially sweetened ones, should be avoided. The result is ready within 2 days.
Sports and medicine
It has been established that among marathon athletes, increased levels of inflammatory and hemostatic markers of cardiovascular risk increase the likelihood of developing acute coronary pathology. There was a twofold increase in the levels of CRP, von Willebrandt factor, D-dimer, leukocyte count, and fibrinolytic activity, which persisted for 4 hours after the end of the competition. The level of fibrinogen decreased immediately after stopping running, but the content of its breakdown product, D-dimer, increased. Consequently, blood clots formed, although this was not clinically evident.
D-dimer: what kind of analysis is it?
Checking the condition of the blood and the possible presence of clots in it is carried out using a blood test. There are two types of tests:
- Quantitative - reveals whether the D-dimer level is elevated or within the normal range. The results show o (increased) or “no” (normal).
- Qualitative - the exact number of D-dimer is indicated in numbers.
Quantitative analysis is more informative and provides doctors with more information about the condition of the patient's bloodstream. During the treatment of hemostasis, the analysis is carried out several times. If the indicator decreases, it means that the blood clot is dissolving and the patient is recovering. But high-quality analysis is cheaper and therefore more accessible to patients.
The test result will allow the doctor to accurately determine the risk of cardiovascular and cancer diseases in a particular patient.
Orthopedics and traumatology for the elderly
Elderly individuals (over 60 years of age) are characterized by changes in the ratio of coagulation, anticoagulation and fibrinolytic systems. Most often they are expressed by shifts towards hypercoagulation. Such patients pose a great risk in terms of endoprosthetics of large joints. In all groups of patients after hip replacement surgery during anticoagulant therapy, the data obtained indicate the development of changes towards hypercoagulation.
Assessment of plasma D-dimer level is one of the sensitive and informative tests for determining the degree of risk of developing thrombotic complications and the effectiveness of anticoagulant therapy.
Indications for analysis
Doctors order a D-dimer blood test for a variety of symptoms and medical history. The test result will allow you to monitor the patient’s condition and prescribe appropriate treatment.
List of indications:
- tendency to thrombosis, disseminated intravascular coagulation syndrome;
- chest pain;
- rapid heartbeat;
- sudden shortness of breath, breathing problems;
- hemoptysis;
- cough;
- cyanosis of the skin and mucous membranes;
- abdominal pain, nausea, vomiting;
- muscle pain;
- sharp pain in the leg or arm;
- change in color of an arm or leg (pallor, blueness, blackening);
- swelling of the limb;
- varicose veins of the legs;
- decrease in daily urine output;
- bleeding from gums;
- pregnancy;
- after injury;
- coronavirus infection COVID-19;
- control during treatment with anticoagulants.
During pregnancy, the risk of blood clots increases, so to monitor a woman’s health, she periodically undergoes a D-dimer test.
With these diseases and conditions, the patient should carefully monitor his well-being and consult a doctor in case of any ailments.
obstetrics and gynecology
The level of D-dimer is of great importance in obstetrics and gynecology. Its level gradually increases from the early stages of pregnancy, and by the end of pregnancy it can exceed the initial level by 3-4 times. Even higher levels of D-dimer are determined in women with complicated pregnancy. D-dimer during in vitro fertilization, along with other indicators of hemostasis (PT, TT, APTT, fibrinogen), serves as a marker of the effectiveness of the stimulation cycle (pregnancy).
Clinical data indicate the high importance of assessing the level of D-dimer as a diagnostic criterion and a method of adequacy of therapy for miscarriage.
Oncological diseases
Thrombosis, as a complication, very often develops with:
- ovarian tumors;
- tumors of the pancreas, stomach;
- lung tumors;
- tumors of the rectum and colon;
- tumors of the mammary glands.
Thrombosis has a wide variety of characteristics:
- thrombosis of deep and superficial veins of the lower extremities;
- thrombosis of the subclavian veins;
- thrombosis of the superior vena cava;
- nonbacterial thrombotic endocarditis;
- various forms of internal combustion engines
Migrating, difficult-to-treat thrombophlebitis of the superficial or deep veins may be the first signs of a latent malignant disease, often ahead of the clinical manifestation of tumors. An unmotivated increase in recurrent vein thrombosis in patients with varicose veins should alert doctors to the presence of malignant diseases. The frequency of such manifestations is up to 35%.
D-dimer serves as an early marker of breast cancer metastasis, indicating lymphovascular invasion and tumor involvement of regional lymph nodes. This should be taken into account when determining the optimal extent of breast surgery
.
What should the normal indicator be?
The normal level of D-dimer in blood plasma is 250 ng/ml. this indicator confirms that the patient is not at risk of thrombosis. In pregnant women, this figure can reach 1000 ng/ml or more, i.e. grow 3–4 times.
Normal D-dimer levels in pregnant women:
- up to 450–500 ng/ml in the 1st trimester;
- up to 900–920 ng/ml in the 2nd trimester;
- up to 1450–1500 ng/ml in the 3rd trimester.
If a pregnant woman, on the contrary, has a low level, she is urgently referred to a hematologist, who will prescribe medications. A decrease in dedimer during pregnancy is a sign of long-standing problems with blood clotting that arose long before pregnancy. With good treatment, childbirth proceeds normally.
Increasing values
Elevated D-dimer levels can occur for two reasons.
- Pathological - thromboembolism, disseminated intravascular coagulation, oncopathology, post-traumatic condition, sickle cell anemia, atrial fibrillation, stroke, heart attack, gastrointestinal bleeding, sepsis, infections, inflammation, nephrotic syndrome and renal failure, liver disease, stress.
- Non-pathological - age, pregnancy, smoking, condition after surgery for a month, invasive manipulations, prolonged immobilization or inactivity, taking estrogen.
In any case, a rise in D-dimer above normal is a sign of the development of thrombosis (the diseases are listed above).
The risk of developing thrombosis in patients with high levels of D-dimer increases 3.5 times than in patients with low concentrations. This indicator only indicates the activation of thrombus formation processes, but does not indicate the location. For a more in-depth study of the condition of the veins, Doppler sonography or scintigraphy is performed.
The following patients are at risk for thrombotic conditions:
- over the age of 50;
- with obesity;
- suffering from cardiovascular diseases;
- have had a stroke or heart attack;
- pregnant women;
- after major operations;
- after burns and injuries;
- cancer patients;
- septic patients - in 95% of cases they have thrombosis.
In the absence of venous thromboembolic complications, D-dimer may also be elevated, then the reasons may be:
- fibrinolytic therapy in the last 7 days before the procedure, meaning taking antiplatelet agents;
- atherosclerosis;
- infections and cirrhosis of the liver.
What does elevated D-dimer mean?
Even a slight increase in this indicator may indicate probable thrombosis. If the D-dimer reaches 273 ng/ml or higher, it is deadly.
D-dimer is elevated in many diseases:
- cardiac ischemia;
- acute coronary syndrome;
- thrombosis of the pulmonary artery (PE) or deep veins;
- DIC syndrome;
- acute or chronic heart failure;
- infections, injuries;
- sepsis;
- hematomas;
- kidney disease;
- preeclampsia and gestosis in pregnant women;
- coronavirus COVID-19;
- old age (over 80 years);
- malignant neoplasms.
The D-dimer level depends on the size of the clot, as well as the time and duration of taking thrombolytic drugs or anticoagulants.
With a decreased D-dimer level, the patient's risk of bleeding increases, so the patient needs to consult a hematologist and other specialists. Doctors conduct additional examinations and laboratory tests and prescribe an appropriate course of treatment.
D-DIMER AS A MARKER OF THROMBUS FORMATION AND ITS APPLICATION IN CLINICAL PRACTICE.
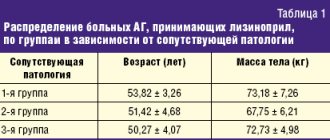
A laboratory test for determining D-dimer based on the frequency of measurements is one of the most popular studies in the practical study of the blood coagulation system. It ranks fourth in terms of the number of prescriptions after prothrombin time (PT), activated partial thromboplastin time (APTT) and fibrinogen. Since the discovery of D-dimer (1970s) and the beginning of its use in clinical practice (1990s), the blood test for D-dimer has firmly entered the arsenal of frequently used tests by doctors of many specialties to diagnose diseases associated with pathological thrombus formation. D-dimer is the end product of a process that occurs in the human body as fibrinolysis. In 1893, the term “fibrinolysis” was proposed to be used by the French physiologist Dastre, and in 1905, a scientist from Germany Morawitz suggested that some enzymes take part in fibrinolysis. This was confirmed by Dr. Sherry (USA) in 1959, who proved that the activator of fibrinolysis is plasmin, formed from its precursor plasminogen. In 1973, two research groups simultaneously reported the discovery of a unique fragment obtained from the hydrolytic cleavage of fibrin protein by the enzyme plasmin in human serum (1). Later, this fragment was called D-dimer and it began to be used as a tool for diagnosing various diseases. Many clinical conditions are characterized by an increase in the concentration of D-dimer in the blood plasma (Table 1).
| Pathological | Not pathological |
| Condition after injury (7) | Smoking (2) |
| Preeclampsia/eclampsia (8.9) | Age (healthy older adults) (3) |
| Oncopathology (10) | Normal pregnancy (4) |
| Disseminated intravascular coagulation (11) | Postoperative condition (5.6) |
| Sickle cell anemia (12) | Invasive manipulations |
| Arterial and venous thromboembolism (13,14) | Inactivity or prolonged immobilization |
| Atrial fibrillation (15) | Long-term use of estrogen drugs |
| Acute coronary syndrome (16) | |
| Stroke (17-19) | |
| Acute gastrointestinal bleeding (20) | |
| Nephrotic syndrome | |
| Infections, sepsis, inflammation | |
| Pulmonary embolism (21) | |
| Kidney diseases (23) | |
| Acute renal failure | |
| Liver diseases (22) | |
| Myocardial infarction | |
| Stress (24) |
Mechanism of D-dimer formation.
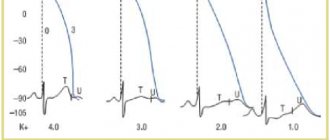
Currently, fibrinogen breakdown products are used to diagnose thrombosis (Fig. 1). Fibrinogen, under the action of thrombin, forms fibrin monomers by cleaving two small fragments (fibrinopeptides A and B). During this process, the negative charge E of fibrinogen (red circles) is converted to a positive charge, allowing fibrin monomers to spontaneously polymerize into a polymer that is stabilized by hydrogen bonds. Thrombin also activates factor XIII (a transglutaminase enzyme), which stabilizes the fibrin parent polymer by catalytically forming cross-linked covalent bonds between adjacent D domains (green circles). Tissue plasminogen activator (t-PA), a serine protease, converts inactive plasminogen into active plasmin, which breaks down fibrin into many small fragments called fibrin degradation products (FDPs). D-dimer, formed from two adjacent cross-linked monomers, is one of the main PDFs. In contrast to the final products of fibrinogen cleavage, which are presented in the form of separate fragments D and E, when cleavage of fibrin fibers cross-linked by factor XIIIa, larger fragments are formed - D-dimers, DED trimers, since plasmin is not able to cleave the covalent bond between D-domains.
Fig.1. Mechanism of D-dimer formation.
Thus, the action of the fibrinolytic system is aimed at the lysis of fibrin, and, with excessive activation, fibrinogen. The result is a mixture of fibrin/fibrinogen degradation products. The products of fibrin degradation are large fragments of D-dimers and trimers, and the products of fibrinogen degradation are individual oligopeptides with a small molecular weight. Only degradation products of cross-linked fibrin contain D-Dimers. The following rule applies:
| Clot + Fibrinolysis = D-dimer formed No clot + Fibrinolysis ≠ D-dimer not formed |
D-dimer refers to both markers of activation of coagulation and fibrin formation, and markers of activation of fibrinolysis. The half-life of D-dimer is approximately 8 hours, clearance is through the kidneys and the reticuloendothelial system. Determination of D-dimer is the most common laboratory marker of activation of coagulation and fibrinolysis.
Methods for determining D-dimer.
1. Qualitative and semi-quantitative methods:
– Agglutination reaction of latex particles (plasma);
2. Quantitative:
– Immunochromatography; Point-of-Care (diagnosis at the point of treatment).
– ELISA (enzyme-linked immunosorbent assay; enzyme-linked immunosorbent method);
– Immunodiffusion on porous membranes;
– Immunoturbidimetry.
Brief description of the methods.
1. Methods for determining D-dimer based on latex agglutination.
Latex beads coated with monoclonal antibodies against D-dimer are added to the plasma containing D-dimer and the time of appearance of macroscopic agglutination on the slide is noted. These are inexpensive and easy to carry out studies. They have moderate sensitivity but higher specificity for deep vein thrombosis (DVT) and pulmonary embolism (PE).
2. Immunochromatography method.
The relative insensitivity of latex agglutination tests led to the development of more sensitive tests based on immunochromatographic rapid diagnostics. This method combines the speed of research (from 2 minutes) with high sensitivity. The particular value of the immunochromatographic method for DVT was noted.
3. ELISA method.
ELISA methods for testing D-dimer have high sensitivity but relatively low specificity. The low specificity of these methods causes false positive results in a significant number of cases. The method consists of adding microplates coated with antibodies to the D-dimer of the plasma under study to the wells. After incubation, enzyme-labeled antibodies are added and, after stopping the reaction, a colorimetric measurement is performed. This method is labor-intensive and time-consuming to carry out, and also requires special equipment. These circumstances make it impractical for routine use in clinical practice.
4. Immunodiffusion on porous membranes .
In recent years, immunoenzyme methods for determining D-dimer have been developed, which allow obtaining results within 10 minutes. They use porous membranes coated with antibodies that capture D-dimer. The patient's plasma is filtered through a membrane and then labeled antibodies are added to the filtrate to detect bound D-dimer
5. Immunoturbidimetry.
One of the options for the latex method for determining D-dimer is the micro-latex agglutination method or the immunoturbidimetric method. When patient plasma containing D-dimer is added to the reagent, the optical density of the solution increases, which is directly proportional to the concentration of D-dimer in the test sample. Commercial kits for the determination of D-dimer have been developed for automatic analyzers (biochemical and coagulometers), which allows studies of this analyte to be carried out routinely.
Two types of D-Dimer units.
1. D-Dimer Units (DDU) - for methods using purified D-Dimer as a calibrator.
2. Fibrinogen Equivalent Unit (FEU ) – fibrinogen equivalent units (FEU), for methods that use PDF, formed under the influence of plasmin, as a calibrator.
The unit size is indicated by the test manufacturer (ng/ml, μg/ml, μg/l).
Reference values of D-dimer.
Threshold values for D-Dimer depending on measurement units:
1. DDU ≤ 0.25 µg/ml (250 ng/ml or 250 µg/l);
2. FEU ≤ 0.5 μg/ml (500 ng/ml or 500 μg/L).
The numerical values are easily converted into each other, since the mass of one FEU unit is equal to half the DDU. For example, 0.5 µg/ml FEU = 0.25 µg/ml DDU.
If the concentration of D-Dimer in plasma is less than the specified threshold values, then the presence of thrombosis in the patient can be excluded.
Limitations in determining D-dimer.
The D-dimer test is not a standardized marker. To date, there are about 30 commercial test systems for determining D-dimer, between which certain differences are observed, since each manufacturer establishes its own standardization method.
The main reasons for the limitations of the method are:
– the use of various monoclonal antibodies (more than 20), differing in specificity and sensitivity;
– lack of International Reference Preparation;
– lack of a standard calibrator;
– different units of measurement used for different methods.
The lack of standardization of different D-dimer test systems means that results, reference intervals and cut-off values cannot be extrapolated across different methods. When quantitatively measuring the D-dimer of the same patient with different test systems, different results are obtained, which are not correct to compare.
Reasons for differences in D-Dimer tests.
1. D-dimer antigen is not homogeneous, but consists of compounds containing fragments D and E with different molecular weights (Fig. 2.)
2. When analyzing D-dimer, various antibodies, buffers, measuring equipment, and standards are used.
Fig.2. D-dimer antigen, consisting of many fragments D and E.
This variability in the types and units of measurement of D-dimer has led to confusion in some laboratories, especially when it was necessary to establish a threshold to exclude venous thromboembolism.
It must be remembered that there are 2 different types of units for D-dimer (Fig. 3):
1. D-dimer unit – DDU with m.m. 195 kDa;
2. Fibrinogen equivalence unit – FEU with m.m. 340 kDa
Fig.3. Two types of units for D-dimer (DDU and FEU).
Because D-dimer is expressed in mass units, the type of units involved is very important in establishing the threshold to rule out venous thromboembolism and in interpreting the results.
Thus, methods for determining D-dimer are based on its interaction with monoclonal antibodies to specific epitopes in the D-domains of fibrin molecules. These specific antibodies bind to D-dimers containing DD covalent bonds, but do not react with fibrinogen and soluble fibrin monomers. D-dimers found in plasma are an indicator of the breakdown of fibrin, but not fibrinogen and fibrin monomers.
Clinical significance of D -dimer .
Clinical applications D-dimer measurement is indicated for:
– exclusion of venous thromboembolism (VTE);
– diagnosis and monitoring of disseminated intravascular coagulation (DIC);
– determination of the duration of anticoagulant therapy.
The issue of using D-dimer remains debatable when:
– prognosis of the course of diseases of the cardiovascular system;
– predicting adverse pregnancy outcomes;
– additional assessment of the risk of thromboembolism in other pathologies.
1. Venous thromboembolism..
Venous thromboembolism is a fairly common pathology that combines deep vein thrombosis and pulmonary embolism. The formation of any thrombus in the vascular bed always leads to the activation of fibrinolysis and the appearance of fibrin breakdown products in the blood. The sensitivity of the D-dimer test in the diagnosis of venous thromboembolism is very high - 90-100%. This test may be performed to confirm the presence of thrombosis. When assessing the results of the study, it should be taken into account that an increase in the level of D-dimer in the blood only indicates the formation of fibrin and its lysis, however, in which part of the vascular bed, in what volume and for what reason this happened must be decided in each specific case with the help of clinical and visualization methods (Doppler ultrasound). The level of D-dimer in PE is practically independent of the localization of the pulmonary thrombus. The D-dimer test has a high negative prognostic level - 97-100%. It is valuable not so much for confirming the fact of thrombosis, but for excluding it. A negative test result almost always indicates the absence of blood clots in the bloodstream. Therefore, the main goal of the D-dimer study is to exclude the presence of blood clots in the vascular bed in the differential diagnosis of DVT and PE.
There are certain limitations to the use of D-dimer in VTE (25-27) (Table 2).
| D-dimer cannot be used to diagnose VTE | D-dimer should be used with caution |
| patients with VTE symptoms > 14 days | patients with recurrent VTE |
| patients taking heparin or oral anticoagulants. | patients aged > 50 years |
| hospitalized patients | |
| pregnant women | |
| up to 30 days after surgery | |
| patients with blood diseases, diabetes mellitus |
Table 2. Limitations when using the D-dimer test for VTE.
It should be noted that D-dimer may be negative in PE if the clot is old (2 weeks or more after clot formation) and if the clot is very small. D-dimer may be falsely elevated in the presence of a high IgM titer. If the threshold value is exceeded, confirmation of the diagnosis is necessary using Doppler ultrasound, spiral computed tomography or contrast venography. Another strategic approach for diagnosing VTE is a preliminary assessment using clinical anamnestic scoring scales (Wells scale) (28-31).
2. Disseminated intravascular coagulation.
Disseminated intravascular coagulation (DIC) is a common pathology with high morbidity and mortality. It is characterized by systemic activation of the hemostatic system with intravascular fibrin formation and increased fibrinolysis (32,33). If patients are not treated appropriately, platelets, clotting factors, and inhibitors become depleted, which can result in life-threatening bleeding and/or thrombosis. DIC is most common in patients with infectious inflammatory diseases, malignant neoplasms, trauma, or obstetric pathology. The classification of DIC divides this pathology into asymptomatic (pre-DIC), organ failure, bleeding and subtypes of massive bleeding. ISTH (International Society of Thrombosis and Haemostasis) has harmonized guidelines for the diagnosis and treatment of DIC (34,35). D-dimer is included in the ISTH guidelines as a recommended laboratory test for the evaluation of patients with DIC.
3. Anticoagulant therapy.
Anticoagulants of indirect action.
After completion of treatment with indirect anticoagulants (ANDA) in patients (including the elderly), quantitative determination of D-dimer levels provides valuable information for individual assessment of the risk of venous thromboembolism. Using statistical methods, age-dependent cut-off levels for D-dimer in relation to the risk of VTE were determined, the components when using various test systems are 250-700 µg/l FEU for patients under 70 years of age and 450-1000 µg/l FEU for patients over 70 years of age (36) (Fig. 4).
Fig.4. Changes in D-dimer concentration depending on age.
At 30 days after warfarin discontinuation, normal D-dimer levels had a very high negative predictive value for recurrent VTE, especially in patients with congenital thrombophilia or new-onset spontaneous thrombosis, and elevated D-dimer levels corresponded to a higher risk of VTE. At the same time, a negative D-dimer test result 2 weeks after the end of a 3-month course of warfarin treatment was associated with a 3.5% risk of recurrent VTE within a year, and a positive result with a risk of 8.9%. These data indicate the important role of D-dimer in determining the optimal duration of AED treatment for reliable prevention of recurrent venous thrombosis.
Heparin therapy.
The effectiveness of heparin therapy is determined by changes in the level of D-dimer dynamics. A decrease in D-dimer indicates a correctly selected dose of heparin in patients with activation of hemostasis of any etiology. The test is also informative for treatment with low molecular weight heparins. Administration of clexane for 2-3 weeks leads to a decrease in the level of D-dimer by 1.5-2 times, and 10-day use of enoxyparine contributed to a decrease in the level of this analyte by 23%.
4. Cardiovascular system.
Circulating D-dimer levels are increased in patients with coronary artery disease, acute ischemic events, including myocardial infarction and unstable angina. In patients with chest pain, elevated D-dimer levels are an early marker of coronary artery ischemia and an independent prognostic factor for myocardial infarction (37). In a study of 18 biomarkers of coronary heart disease risk in a cohort of more than 27,000 postmenopausal women, only D-dimer levels were significantly increased and were a risk factor independent of other markers (38). The work of Marcucci R. et al. (39) showed that the content of D-dimers is significantly higher in patients with functional class IV of chronic heart failure (CHF) compared to patients with functional classes II and III. This study, which included 214 patients with functional classes II–IV, convincingly proved that an increase in D-dimers is a significant predictor of mortality in CHF.
5. D-dimer level during pregnancy.
In pregnant women, due to the activation of the synthesis of plasma hemostatic factors in the liver, even normally, a moderate thrombophilic situation is observed. By the time of birth, D-dimer levels may be 3-4 times higher than baseline (40) (Table 3).
| Units | Not pregnant | 1st trimester | 2nd trimester | 3rd trimester |
| ng/ml | < 500 | 50 – 950 | 320 – 1290 | 130 – 1700 |
Table 3. Plasma D-dimer levels in normal pregnancy.
Shifts in hemostasis parameters reach a maximum in the 3rd trimester of pregnancy, which has physiological significance and is aimed at reducing blood loss during childbirth. Positive D-dimer results in late pregnancy significantly complicate risk assessment and diagnosis of DVT and especially PE. A significant (5-10 times) increase in the level of D-dimer is observed in pregnancy pathologies (recurrent miscarriage, gestosis, premature placental abruption). This leads to the appointment of additional diagnostic procedures. In such cases, the combined use of ultrasound and D-dimer analysis is of particular importance. The cut-off level of D-dimer in relation to the risk of venous thromboembolism in pregnant women in the 3rd trimester appears to be significantly higher.
6. Assessment of the risk of thromboembolism in other diseases.
Elevated levels of D-dimer are observed in diseases such as benign and malignant tumors, infections, trauma, ischemia, bleeding or thrombosis. For many of these pathologies, researchers have attempted to use D-dimer levels as a diagnostic and prognostic test. For example, D-dimer levels have been studied as poor prognosis and/or risk factors in patients with malignancies, gastrointestinal bleeding and necrosis, intracerebral hemorrhage, sickle cell disease, migraine with severe headaches, traumatic brain injury, tuberculosis, Cushing's disease, asthma and many other diseases. Of all these diseases, cancer has attracted the greatest interest. Overall, the risk of venous thrombosis in cancer patients is 7% due to the prothrombotic effect of malignancy and associated risk factors such as immobilization, medications, and surgery (41,42). However, elevated D-dimer levels in cancer patients limit the diagnostic value of the result when used alone. Numerous studies have shown the unfavorable prognostic significance of elevated plasma D-dimer levels in patients with breast, colon, lung, ovarian, prostate, and other cancers (43–52).
Conclusion.
D-dimer is a reliable and sensitive test for the process of thrombus formation, and an increase in its content in the blood plasma indicates the presence of blood clots. In clinical practice, D-dimer is used as a marker of the body's ability to hypercoagulate and endogenous fibrinolysis. A positive D-dimer test has a negative prognostic value for patients with DVT and PE. This test is used to monitor anticoagulant therapy and is a sensitive marker in the diagnosis of DIC syndrome. It is advisable to prescribe a D-dimer test during pregnancy to exclude the diagnosis of DVT. D-dimer plays a significant role as one of the potential risk factors for the development of coronary heart disease. Therefore, D-dimer can be considered one of the most valuable laboratory tests for diagnosing and monitoring conditions associated with thrombosis.
LITERATURE
1. Gaffney PJ D-dimer. History of the Discovery, Characterization and Utility of this and other Fibrin Fragments. Fibrinolysis // l993.-7.-Suppl 2: P. 2-8.
2. Lowe GD, Yarnell JW, Rumley A, et al. C-reactive protein, fibrin D-dimer, and incident ischemic heart disease in the Speedwell Study: are inflammation and fibrin turnover linked in pathogenesis? Arterioscler Thromb Vasc Biol 2001;21:603–10.
3. Pieper CF, Rao KM, Currie MS, et al. Age, functional status, and racial differences in plasma D-dimer levels in community-dwelling elderly persons. J Gerontol Med Sci 2000;55:M649–57.
4. Eichinger S. D-dimer testing in pregnancy. Semin Vasc Med. 2005;5(4): 375–378.
5. Larsen JF, Ejstrud P, Svendsen F, et al. Randomized study of coagulation and fibrinolysis during and after gasless and conventional laparoscopic cholecystectomy. Br J Surg 2001;88:1001–5.
6. Nguyen NT, Owings JT, Gosselin R, et al. Systemic coagulation and fibrinolysis after laparoscopic and open gastric bypass. Arch Surg
2001;136:909–16.
7. Engelman DT, Gabram SGA, Allen L, et al. Hypercoagulability following multiple trauma. World J Surg 1996;20:5–10.
8. Kobayashi T, Tokunaga N, Sugimura M, et al. Coagulation/fibrinolysis disorder in patients with severe preeclampsia. Semin Thromb Hemost 1999;25:451–4.
9. Kobayashi T, Tokunaga N, Sugimura M, et al. Predictive values of coagulation/fibrinolysis parameters for the termination of pregnancy complicated by severe preeclampsia. Semin Thromb Hemost 2001;27:137–41.
10. Raimondi P, Bongard O, de Moerloose P, et al. D-dimer plasma concentration in various clinical conditions: Implication for the use of this test in the diagnostic approach of venous thromboembolism. Thromb Res 1993;69:125–30.
11. Lane DA, Preston FE, Van Ross ME, et al. Characterization of serum fibrinogen and fibrin fragments produced during disseminated intravascular coagulation. Br J Haematol 1978;40:609–15.
12. Tomer A, Harker LA, Kasey S, et al. Thrombogenesis in sickle cell disease. J Lab Clin Med 2001;137:398–407.
13. Di Nisio M, Squizzato A, Rutjes AW, Buller HR, Swinderman AH, Bossuyt PM. Diagnostic accuracy of D-dimer test for exclusion of venous thromboembolism: a systematic review. J Thromb Haemost. 2007;5(2):296–304.
14. Acosta S, Nilsson TK, Björck M. Preliminary study of D-dimer as a possible marker of acute bowel ischaemia. Br J Surg 2001;88:385–8.
15. Nakagawa K, Hirai T, Shinokawa N, et al. Relation of fibrillatory wave amplitude with hemostatic abnormality and left atrial appendage dysfunction in patients with chronic nonrheumatic atrial fibrillation. Jpn Circ J 2001;101:13–21.
16. Bayes-Genis A, Mateo J, Santalo M, et al. D-Dimer is an early diagnostic marker of coronary ischemia in patients with chest pain. Am Heart J 2000;140:379–84.
17. Berge E, Friis P, Sandset PM. Hemostatic activation in acute ischemic stroke. Thromb Res 2001;101:13–21.
18. Nina P, Schisano G, Chiapetta F, et al. A study of blood coagulation and fibrinolytic system in spontaneous hemorrhage. Correlation with Hunt-Hess grade and outcome. Surg Neurol 2001;55:197–203.
19. Koch HJ, Horn M, Bogdahn U, Ickenstein GW. The relationship between plasma D-dimer concentrations and acute ischemic stroke subtypes. J Stroke Cerebrovasc Dis. 2005;14(2):75–79.
20. Vreeburg EM, Levi M, Rauws EA, et al. Enhanced mucosal fibrinolytic activity in gastroduodenal ulcer hemorrhage and the beneficial effect of acid suppression. Aliment Pharmacol Ther 2001;15:639–46.
21. Jimenez Castro D, Perez-Rodriguez E, Montaner L, et al. Diagnostic value of D-dimer in pulmonary embolism and pneumonia. Respiration 2001;68:371–5.
22. Cioni G, Cristani A, Mussini C, et al. Incidence and clinical significance of elevated fibrin(ogen) degradation product and/or D-dimer levels in liver cirrhosis patients. Ital J Gastroenterol. 1990;22(4):70–74.
23. Noha M., Hiba B. D-dimer Levels in Patients Presenting Chronic Kidney Disease in Sudan. American Journal of Medicine and Medical Sciences 2021, 6(3): 120-122.
24. von Kanel R, Bellingrath S, Kudielka B. Association of vital exhaustion and depressive symptoms with changes in fibrin D-dimer to acute psychosocial stress. J Psychosom Res. 2009. 67(1): 93-101.
25. Thachil J, Fitzmaurice DA, Toh CH. Appropriate use of D-dimer in hospital patients. Am J Med. 2010;123(1):17–19.
26. Lippi G, Bonfanti L, Saccenti C, Cervellin G. Causes of elevated D-dimer in patients admitted to a large urban emergency department. Eur J Intern Med. 2014;25(1):45–48.
27. Spring JL, Winkler A, Levy JH. The influence of various patient characteristics on D-dimer concentration in critically ill patients and its role as a prognostic indicator in the intensive care unit setting. Clin Lab Med.
2014;34(3):675–686.
28. Rodger MA, Le Gal G, Wells P, et al. Clinical decision rules and D-Dimer in venous thromboembolism: current controversies and future research priorities. Thromb Res. 2014;134(4):763–768.
29. Streiff MB. Predicting the risk of recurrent venous thromboembolism (VTE). J Thromb Thrombolysis. 2015;39(3):353–366.
30. Sartori M, Cosmi B, Legnani C, et al. The Wells rule and D-dimer for the diagnosis of isolated distal deep vein thrombosis. J Thromb Haemost. 2012;10(11):2264–2269.
31. Novielli N, Sutton AJ, Cooper NJ. Meta-analysis of the accuracy of two diagnostic tests used in combination: application to the ddimer test and the wells score for the diagnosis of deep vein thrombosis. Value Health.2013;16(4):619–628.
32. Levi M. Diagnosis and treatment of disseminated intravascular coagulation. Int J Lab Hematol. 2014;36(3):228–236.
33. Wada H, Matsumoto T, Aota T, Yamashita Y. Progress in diagnosis and treatment for disseminated intravascular coagulation. 2015;56(2):169–176.
34. Wada H, Thachil J, Di Nisio M, et al. Harmonized guidance for disseminated intravascular coagulation from the International Society on Thrombosis and Haemostasis and the current status of anticoagulant therapy in Japan: a rebuttal. J Thromb Haemost. 2013;11(11):2078–2079.
35. Wada H, Matsumoto T, Yamashita Y. Diagnosis and treatment of disseminated intravascular coagulation (DIC) according to four DIC guidelines. J Intensive Care. 2014;2(1):15.
36. Lippi G, Favaloro EJ, Cervellin G. A review of the value of D-Dimer testing for prediction of recurrent venous thromboembolism with increasing age. Semin Throm Hemost 2014;40(6) 634-639.
37. Koenig W, Rothenbacher D, Hoffmeister A, Griesshammer M, Brenner H. Plasma fibrin D-dimer levels and risk of stable coronary artery disease: results of a large case-control study. Arterioscler Thromb Vasc Biol. 2001;21(10):1701–1705.
38. Kim HC, Greenland P, Rossouw JE, et al. Multimarker prediction of coronary heart disease risk: the Women's Health Initiative. J Am Coll Cardiol. 2010;55(19):2080–2091.
39. Marcucci R., Gori A. et al. Markers of hypercoagulability and inflation predict mortality in patients with heart failure // Ibid. 2006. Vol. 4. P. 1017–1022.
40. Abbassi-Ghanavati M, Greer LG, Cunningham FG. Pregnancy and laboratory studies: a reference table for clinicians. Obstet Gynecol. 2009 Dec;114(6):1326-31.
41. Arora M, Wun T. Adverse impact of venous thromboembolism on patients with cancer. Semin Thromb Hemost. 2014;40(3):313–318.
42. Stricker H. Venous thromboembolism and cancer: pathophysiology and incidence. Vasa. 2014;43(4):239–243.
43. Blackwell K, Hurwitz H, Liebe´ rman G, et al. Circulating D-dimer levels are better predictors of overall survival and disease progression than carcinoembryonic antigen levels in patients with metastatic colorectal carcinoma. Cancer. 2004;101(1):77–82.
44. Kilic M, Yoldas O, Keskek M, et al. Prognostic value of plasma D-dimer levels in patients with colorectal cancer. Colorectal Dis. 2008;10(3):238–241.
45. Khoury JD, Adcock DM, Chan F, et al. Increases in quantitative D-dimer levels correlate with progressive disease better than circulating tumor cell counts in patients with refractory prostate cancer. Am J Clin Pathol. 2010;134(6):964–969.
46. Ay C, Dunkler D, Pirker R, et al. High D-dimer levels are associated with poor prognosis in cancer patients. Haematologica. 2012;97(8):1158–1164.
47. Yamamoto M, Yoshinaga K, Matsuyama A, et al. Plasma D-dimer level as a mortality predictor in patients with advanced or recurrent colorectal cancer. Oncology. 2012;83(1):10–15.
48. Liu L, Zhang X, Yan B, et al. Elevated plasma D-dimer levels correlate with long term survival of gastric cancer patients. PLoS One. 2014;9(3):e90547.
49. Zhang X, Liu ZQ, Zhang W, Xu Q. A retrospective analysis of plasma Ddimer dynamic variation in terminal stage cancer patients: implications for disease progression. Int J Clin Exp Med. 2014;7(8):2395–2401.
50. Sakurai M, Satoh T, Matsumoto K, et al. High pretreatment plasma Ddimer levels are associated with poor prognosis in patients with ovarian cancer independently of venous thromboembolism and tumor extension. Int J Gynecol Cancer. 2015;25(4):593–598.
51. Wang Y, Wang Z. Predictive value of plasma D-dimer levels in patients with advanced non-small-cell lung cancer. Onco Targets Ther. 2015;8:805–808.
52. Fukumoto K, Taniguchi T, Usami N, et al. The preoperative plasma D-dimer level is an independent prognostic factor in patients with completely resected non-small cell lung cancer. Surg Today. 2015;45(1):63–67.
Blood donation
Externally, donating blood is no different from a regular intravenous injection. The prepared patient is placed on a couch or asked to sit in a special chair. Then the woman needs to expose her arm above the elbow. A nurse applies a venous tourniquet just above the elbow, and the woman is asked to clench and unclench her fist several times. The injection site is treated with alcohol twice, after which an injection is given and the required amount of blood is collected. At this point, the patient may experience minor discomfort. After completing the set, a cotton ball moistened with alcohol is applied to the injection site and asked to hold the arm in a bent position. The resulting material is sent to the laboratory for further research.
Preparation
In order for the D-dimer analysis to be as informative as possible, you should prepare for it. In principle, the doctor’s recommendations will be extremely simple, but failure to comply with them may lead to distorted results.
Blood donation occurs in the morning, on an empty stomach. 12 hours before the procedure, a woman should limit the amount of fluid she takes. You should not drink strong coffee or tea 24 hours before the test. During the week before the expected analysis, you should adhere to proper nutrition as much as possible. It is necessary to exclude fried, fatty and smoked foods, flavor enhancers, and copious amounts of spices. You should give preference to lean meats (veal, rabbit, chicken) and fatty fish. The latter contains a large amount of polyunsaturated fatty acids, which are essential for the normal functioning of the maternal cardiovascular system and the development of the fetal nervous system.
The diet should contain a large amount of fresh vegetables and fruits. They are rich in vitamins, macro- and microelements, which has a beneficial effect on the course of pregnancy. Your doctor or nurse will tell you more about preparing for the test. In most clinics, women after IVF are given a special leaflet in which all the recommendations are written down. This greatly simplifies preparation for the procedure.
Normal indicators during pregnancy
Regardless of how pregnancy occurs, the dimer concentration in a woman expecting a child will be slightly higher than in the general population. In the first three months of embryo development, it is considered normal to exceed the norm by one and a half times. By the end of the second trimester, the figure can exceed the norm by three times. In the future the level may be even higher. All options considered are the norm both for women whose pregnancy occurred naturally and for patients after IVF. These conditions do not require specialized treatment. On the contrary, drug-induced reduction in indicators is often accompanied by excessive blood thinning and severe bleeding, especially during or after childbirth.