What can affect the result?
Increased bilirubin levels are promoted by:
- Long-term refusal to eat
- Excessive exercise
- Smoking
- Some medications, microelements and vitamins
The study result may be distorted when contrast agents are administered during the day.
Important! The interpretation of the analysis is carried out only by a doctor. If necessary, the patient is referred for other examinations (including instrumental and functional).
We recommend that you consult your doctor and get a check-up.
Symptoms indicating increased bilirubin
There are symptoms the presence of which in a person means that the percentage of bilirubin in the blood is too high:
- The whites of the eyes began to turn yellow.
- The skin color becomes more jaundiced.
- Itching of the skin, which intensifies at night.
These symptoms are an important indicator that the body is undergoing internal bile poisoning; ignoring these problems can lead to serious disruptions in the functioning of the body.
The often manifested bitter taste in the mouth is also one of the symptoms of increased bilirubin in the blood.
treatment of direct bilirubin in the blood
A rapid increase in this substance provokes the darkening of the urinary fluid to a brown color, and solid bowel movements take on a white color. All of the above symptoms are accompanied by severe weakness, high fever and enlarged liver. If you detect at least one of the above symptoms, you should immediately seek help from the nearest hospital.
Analysis result
| Age | Reference values (in µmol/l) |
| The first day after birth | 24-149 |
| 1-3 years | 58-197 |
| 4-5 years | 26-205 |
| More than 5 years | 5-21 |
An increase in total bilirubin can lead to:
- Cholelithiasis
- Viral hepatitis
- Cirrhosis of the liver
- Choledocholithiasis
- Pernicious, hemolytic, or sickle cell anemia
- Autoimmune hemolysis
- Thalassemia
- Gilbert and Crigler–Nayjar syndromes
- Malaria
- Sepsis
- Transfusions of incompatible blood group
- Hemorrhages in tissue
- Hemorrhagic pulmonary infarction
- Myocardial infarction
- Alcoholic liver disease
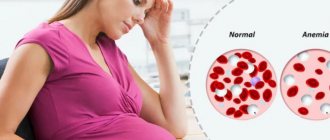
Bilirubin levels increase during pregnancy, infectious mononucleosis, liver abscesses, toxic hepatitis, cirrhosis, massive tumors or metastases in the liver.
Generally accepted norms of indicators
The acceptable level of bilirubin concentration for each age is different. The highest concentration of the substance in the blood is observed in newborns, in the initial stages of life, up to 200 µmol/l, this is due to the period of adaptation of the newborn’s gastrointestinal tract to the digestion of mother’s milk. The acceptable level of bilirubin concentration for each age will be different. The highest concentration of the substance in the blood is observed in newborn children, in the initial stages of life. In one-year-old children and children under 13 years of age, a satisfactory indicator of the concentration of indirect pigment is considered to be up to 20.3 µmol/l, for direct pigment up to 5.2 µmol/l.
The degree of concentration of the substance for adults should not cause concern if the survey analysis shows a level of up to 19.9 µmol/l for indirect, and 4.9 µmol/l for direct bilirubin, since such measurements are satisfactory for people of the adult age category.
Additional Research
For the most objective examination and obtaining accurate data for making a diagnosis or solving other problems, the patient may be referred to:
- Complete laboratory examination of the liver and pancreas
- Submission of biochemical markers
- Primary diagnosis of viral hepatitis
Patients also submit:
- General blood and urine tests
- Coprogram
- Analyzes to identify indicators such as AST and ALT, amylase, total cholesterol, albumin, gamma-GT, etc.
Causes of increased bilirubin in the blood
The source of the pathological condition is caused by disruption of the liver, resulting in improper outflow of bile, which causes the occurrence of viral lesions and hepatitis.
symptoms of increased bilirubin
The cause of increased bilirubin in the blood may be:
- Chronic or autoimmune hepatitis.
- Non-benign neoplasms in the liver area.
- Incorrect functioning of the pancreas.
- Intoxication of the body through poisoning can also cause an increase in bilirubin.
By the way, any of the above reasons is pathological and requires immediate medical intervention and long-term treatment
MEDSI cares about its patients
- Experienced specialists.
They professionally conduct research on biological material, which guarantees diagnostic accuracy - Comfortable conditions for taking the analysis.
You can take the test throughout the day. The results will be available in your personal account - Modern laboratory equipment.
It corresponds to a high European and global level. The laboratory uses equipment from leading manufacturers such as Beckman Coulter, Siemens, Ortho Clinical Diagnostics, Thermo Fisher, Sysmex, BD. All areas of testing and evaluation of biomaterials are equipped with the latest equipment that allows for high-level/high-precision diagnostics - Regular maintenance of equipment and automation of research processes.
All analytical installations are serviced and meet quality standards. All processes are automated as much as possible and built in accordance with LEAN management. This allows the laboratory to control processes, minimize time and errors during analysis - Automation of the process of sorting biomaterials.
Preliminary identification of the biomaterial is carried out in front of the patient. Eliminates the possibility of losing the test tube - The shortest processing time for materials.
They are provided with modern equipment and experienced specialists - It is possible to undergo a comprehensive examination. This ensures a quick and accurate diagnosis
To make an appointment with a doctor and clarify the conditions for taking the test (including its cost), call +7 (495) 7-800-500. Our specialist will answer your questions and suggest the optimal time to visit the clinic. Recording is also possible through the SmartMed application.
Treatment of elevated direct bilirubin
You can influence the high concentration of bilirubin in the blood by following a diet and doing physical exercise. After undergoing a biochemical examination of the blood, based on the tests obtained, the doctor prescribes the patient a set of treatment and recommendations aimed at establishing the proper functioning of the liver and the outflow of bile. Even with the slightest discrepancy with the norms, the doctor is obliged to prescribe treatment to correct the functioning of metabolic processes; you can often undergo such a course of treatment at home, while following all the recommendations. In this case, the examination results show a disappointing picture; if necessary, surgical intervention is required, followed by hospitalization in a hospital.
Direct bilirubin
Other names: Direct bilirubin, conjugated bilirubin, conjugated bilirubin, newborn bilirubin, Direct bilirubin, Conjugated bilirubin.
Service code for ordering 1049 (direct bilirubin) in the Sinevo medical laboratory.
general information
Bilirubin is a pigment found in bile. It is formed during the breakdown of waste hemoglobin, the main component of red blood cells. This is due to the constant renewal of red blood cells. The body reuses iron, which is part of hemoglobin, and the protein part of the molecule is converted into bilirubin.
Initially, when hemoglobin is broken down, indirect (unbound, unconjugated) bilirubin is formed. This bilirubin is toxic and to neutralize it, it is transported in the blood to the liver using a special protein - albumin. There it binds to a special component - glucuronic acid - and turns into direct (bound, conjugated) bilirubin, which, in turn, is non-toxic and is excreted with bile into the intestines and kidneys for excretion from the body. Total bilirubin determined in the blood is the sum of indirect and direct bilirubin.
Normally, direct bilirubin is practically not found in the blood. Its amount increases in cases where the liver is able to form direct bilirubin from indirect bilirubin, but cannot remove it in a timely manner. Most often this happens due to blockage of the bile ducts, as well as due to damage to liver tissue due to hepatitis or cirrhosis.
When the outflow of bile is obstructed (impaired outflow), bilirubin does not enter the intestines and, accordingly, does not turn into a brown pigment, so the stool becomes lightened. Excess amounts of direct bilirubin, penetrating into the urine, begin to give it a dark color.
In the Sinevo laboratory, total and direct bilirubin . The difference between them is the amount of indirect bilirubin.
Bilirubin is a marker of liver biliary tract dysfunction.
Indications for use:
- routine medical examination;
- preparation for surgical operations;
- alcohol abuse;
- jaundice of unspecified etiology;
- when symptoms appear (symptoms appear): weakness, loss of appetite, nausea, vomiting, abdominal pain (especially in the right hypochondrium), darkening of urine and lightening of stool, itching;
- assessment of the degree of bilirubinemia;
- differential diagnosis of various types of jaundice (jaundice) (study of bilirubin fractions);
- diseases of the liver and biliary tract;
- hemolytic anemia.
Method: colorimetric diazo method
Analyzer: Cobas 6000
Units: µmol/l
Material for research: venous blood serum
Preparation:
- Take on an empty stomach (after sleep and 8–12 hours of fasting). It is permissible to drink only clean non-carbonated water (up to 200 ml) (with the exception of glucose testing);
- do not consume spicy, fatty, fried foods and alcohol 1–2 days before the test;
- exclude physical and emotional stress 1 day before the analysis;
- do not smoke for at least 1 hour before the test;
- It is not recommended to take (take the test) after radiography, physiotherapeutic procedures and instrumental examinations.
Interpretation of results: (analysis results)
The result of laboratory tests is not a sufficient basis for making a diagnosis. Interpretation of the results and diagnosis is carried out only by the attending physician.
Reference values:
less than 5.0
Level up:
- hepatitis of various etiologies (acute viral hepatitis, hepatitis caused by cytomegalovirus, infectious mononucleosis, amoebiasis, opisthorchiasis, actinomycosis, secondary and tertiary syphilis, acute toxic hepatitis);
- taking hepatotoxic medications;
- pathology of the biliary tract (cholangitis, cholecystitis);
- oncopathology (primary hepatocarcinoma, metastatic liver lesions);
- hereditary hyperbilirubinemia (Dabin-Johnson syndrome, Rotor syndrome);
- hypothyroidism in newborns;
- obstructive jaundice (gastrointestinal tract disease, tumors of the head of the pancreas, helminthic infestation);
- biliary cirrhosis (primary or secondary);
- jaundice of pregnant women.
Downgrade:
- anemia of a non-hemolytic nature (CRF, tuberculosis, acute leukemia, post-hemorrhagic anemia);
- in premature babies (prematurity in children);
- smoking;
- the effect of sunlight or ultraviolet rays on a blood sample.
Factors influencing the result:
Promotion:
Substances that increase bilirubin levels: acebutolol, acyclovir, allopurinol, amitriptyline, antifungal drugs, antimalarial drugs, antipyretics, barbiturates, captopril, carbamazepine, cephalosporins, clindamycin, cyclosporine, diclofenac, doxorubicin, doxycycline, enalapril, furosemide, methotrexate, methyldopa, papaverine, penicillin, rifampicin, streptomycin, thiazides, hepatitis B vaccine, BCG vaccine, etc.
Demotion:
Substances that affect the decrease in bilirubin levels:
- alcohol,
- barbiturates,
- caffeine,
- prednisolone,
- penicillin,
- amikacin,
- anticonvulsants,
- theophylline, etc.
Where to get tested for direct bilirubin
take a blood test for direct bilirubin at any Synevo point in Minsk, Baranovichi, Bobruisk, Borisov, Brest, Vitebsk, Gantsevichi, Gomel, Grodno, Zhlobin, Lida, Mogilev, Mozyr, Molodechno, Novogrudok, Novopolotsk, Orsha, Pinsk, Polotsk, Rechitsa, Svetlogorsk, Slutsk, Smorgon, Soligorsk.
Signs of increased bilirubin
The liver is the main link in the production and removal of bilirubin from the body. Therefore, most diseases that provoke an increase in the amount of pigment in the blood are associated with the liver. In liver pathologies, increased bilirubin manifests itself as follows:
- Discomfort in the right side;
- Nausea, belching after eating (especially after fatty foods);
- Dizziness, loss of strength, bad mood;
- Light stool and dark urine;
- With viral hepatitis, increased body temperature.
The following symptoms are observed in gallstone disease:
- yellowness of the skin and mucous membranes;
- pain in the right side;
- bloating, abnormal stool;
- skin itching.
To failure: how liver diseases progress In the initial stages, liver diseases are completely reversible, but there are conditions when medications are powerless and only a transplant can save the patient’s life.
How is bilirubin formed?
Erythrocytes - red blood cells - contain hemoglobin. It carries oxygen to the body tissues from the lungs. When old and damaged red blood cells die, hemoglobin is released and converted into bilirubin.
Bilirubin is converted hemoglobin
Newly formed bilirubin is called indirect: it is highly toxic and dangerous to humans, especially to the central nervous system (CNS). Therefore, the body then starts the process of neutralizing bilirubin - this happens in the liver. When bilirubin becomes safe - straight - the liver secretes it along with bile, and it leaves the body through the intestines.
When an analysis is made for bilirubin levels, there are three types: indirect, direct and total. For an adult under 60 years of age, the following indicators are considered normal:
- Indirect bilirubin – within 3.4-12 mmol/l;
- Direct bilirubin – within 1.7-5.1 mmol/l;
- Total bilirubin is in the range of 5.1-17 mmol/l.
If the bilirubin level is higher than normal, you need to find out the reason for the jump, because it may indicate the development of a serious illness.
Where do diffuse liver changes come from? Diffuse changes affect the structure of the liver, its main functional tissue – the parenchyma.