Vertebral (vertebral) artery syndrome is the definition of a group of syndromes (vascular, autonomic) resulting from impaired blood flow in the vertebral arteries caused by various problems. The main etiological causes of the development of vertebral artery syndrome are the following diseases.
- Vascular diseases with impaired vascular patency, such as atherosclerosis, various arthritis, embolism.
- Changes in the shape of the arteries (deformations) - abnormal tortuosity, significant kinks, abnormal structural changes in the arteries.
- Extravasal vascular compression (compression of arteries by osteophytes, hernias, disc protrusions, compression by bone abnormalities, tumors, scar tissue)
Considering that the syndrome can be caused by various factors, sometimes difficulties arise with the interpretation of such a diagnosis as vertebral artery syndrome , since this syndrome can designate a variety of conditions, for example, acute circulatory disorders. But in clinical practice, the most important are degenerative-dystrophic changes in the cervical spine and abnormal phenomena in the atlas, which lead to disruption of blood flow in the vertebral arteries and the appearance of symptoms of cerebrovascular accident.
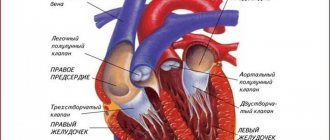
There are extracranial and intracranial sections of the vertebral artery.
A significant part of the extracranial section of the vertebral arteries passes through a mobile canal formed by openings in the transverse processes of the vertebrae. The sympathetic nerve (Frank's nerve) also passes through this canal. At the C1-C2 level, the vertebral arteries are closed only by soft tissue. This anatomical feature of the passage of the vertebral arteries and the mobility of the cervical spine significantly increase the risk of developing compression effects on the vessels from surrounding tissues.
The resulting compression from surrounding tissues leads to compression of the artery of the autonomic endings and constriction of blood vessels due to reflex spasm, which leads to insufficient blood supply to the brain.
Degenerative changes in the cervical spine (osteochondrosis, arthrosis of the facet joints, uncovertebral arthrosis, instability of motor segments, disc herniations, spondylosis deformans, bone growths (osteophytes), muscle reflex syndromes (inferior oblique muscle syndrome, anterior scalene muscle syndrome) are often the cause of compression vertebral arteries and the development of vertebral artery syndrome . Most often, compression occurs at the level of 5-6 vertebrae, slightly less often at the level of 4-5 and 6-7 vertebrae. The most common cause of the development of vertebral artery syndrome is uncovertebral syndrome. The close location of these joints to the vertebral arteries leads to the fact that even small exostoses in the area of uncovertebral joints lead to mechanical effects on the vertebral arteries.With significant uncovertebral exostoses, significant compression of the lumen of the vertebral arteries is possible.
Anomalies of Kimberly and Powers play a fairly significant role in the development of vertebral artery syndrome.
Symptoms
According to the clinical course, two stages of vertebral artery syndrome are distinguished: functional and organic.
The functional stage of vertebral artery syndrome is characterized by a certain group of symptoms: headaches with some autonomic disorders, cochleovestibular and visual disturbances. Headache can have various forms, both acute throbbing and constant aching or sharply intensifying especially when turning the head or prolonged static load. The headache may spread from the back of the head to the forehead. Disturbances in the cochleovestibular system can manifest as paroxysmal dizziness (swaying instability) or systemic dizziness. In addition, some hearing loss may occur. Visual disturbances can manifest as darkening of the eyes, a feeling of sparks, sand in the eyes.
Prolonged and prolonged episodes of vascular disorders lead to the formation of persistent foci of ischemia in the brain and the development of the second (organic) stage of vertebral artery syndrome . In the organic stage of the syndrome, symptoms of both transient and persistent hemodynamic disorders of the brain appear. Transient hemodynamic disturbances are manifested by symptoms such as dizziness, nausea, vomiting, and dysarthria. In addition, there are characteristic forms of ischemic attacks that occur during turning or tilting the head, during which attacks of falling with preserved consciousness may occur, so-called drop attacks, as well as attacks with loss of consciousness lasting up to 10 minutes (syncope episodes). Symptoms usually regress in a horizontal position and are thought to be due to transient ischemia of the brainstem. After such episodes, general weakness, tinnitus, and autonomic disturbances may occur.
Based on the type of hemodynamic disturbances, several variants of vertebral artery syndrome are distinguished (compressive, irritative, angiospatic and mixed forms).
Vessel narrowing in the compression variant occurs due to mechanical compression on the artery wall. In the irritative type, the syndrome develops as a result of reflex spasms of the vessel due to irritation of sympathetic fibers. In the clinic, most often, combined (compression-irritative) variants of vertebral artery syndrome are encountered. In the angiospastic variant of the syndrome, there is also a reflex mechanism, but it arises from irritation of receptors in the area of the motor segments of the cervical spine. In the angiospastic variant, vegetative-vascular disorders predominate and the symptoms are not so strongly associated with head turns.
Features of pharmacotherapy of pain syndrome due to vibration disease
Pain is the main complaint in vibration disease and a characteristic manifestation of its main clinical syndromes: polyneuropathy, radiculopathy, degenerative joint damage, angiodystonic disorders, causing a decrease in quality of life and ability to work.
Modern vibration disease is characterized by polymorphism of symptoms with a predominant involvement of the vascular, nervous and musculoskeletal systems in the pathological process. The formation of clinical symptoms of vibration disease depends on the duration of action and parameters of vibration, its combination with other harmful production factors (noise, cooling, static-dynamic loads) [4].
Industrial vibration, when exposed to the human body, causes a complex set of regulatory disorders with the simultaneous or sequential formation of neurohumoral, neurohormonal and reflex disorders [1].
As a result of dysregulation of vascular tone, regional circulatory disorders develop, characterized by specific phenomena of peripheral angiodystonic syndrome, including attacks of vasospasm (Raynaud's syndrome). Vibration disease from exposure to general vibration is characterized by the development of not only peripheral, but also cerebral angiodystonic syndrome.
Vascular disorders lead to changes in transcapillary metabolism with the progression of tissue hypoxia and the subsequent development of trophic disorders [1].
Violation of the trophism of peripheral neurons leads to demyelination, disintegration of axial cylinders and the development of the second most common vibration disease syndrome - sensory polyneuropathy. At the initial stage of vibration disease, exposure to local vibration may lead to the formation of mononeuropathy of the upper extremities, primarily in the form of damage to the median nerve—carpal tunnel syndrome [4, 10].
As the pathological process progresses, sensory polyneuropathy of the upper extremities from exposure to local vibration can be accompanied by vegetative-trophic disorders, combined with myofibrosis of the forearms and shoulder girdle, arthrosis or periarthrosis, most often of the wrist and elbow joints [8].
When exposed to general vibration, polyneuropathy of the upper and lower extremities with sensory and, possibly, vegetative-trophic disorders, as the pathological process progresses, is most often combined with radiculopathy of the lumbosacral level [6].
The combination of vibration with physical activity and functional overstrain of the musculoskeletal system of the corresponding localization contributes to the aggravation of the course of vibration disease.
Pain syndrome in the clinic of vibration disease
Depending on the leading etiopathogenetic mechanism, pain syndromes are divided into nociceptive (somatogenic), associated with tissue damage, neuropathic (neurogenic), caused by primary dysfunction or damage to the structures of the nervous system, and psychogenic, arising from mental disorders [7].
The clinical structure of pain syndrome in vibration disease is heterogeneous and is often a combination of symptoms reflecting manifestations of nociceptive, neuropathic and psychogenic pain.
In the genesis of pain in peripheral angiodystonic syndrome, the ischemic factor is of primary importance.
Peripheral angiodystonic syndrome is manifested by aching pain in the extremities, accompanied by numbness, increased chilliness, aggravated by cooling.
Sudden attacks of “whitening” of the fingers are characteristic, followed by cyanosis, then hyperemia, accompanied by pain (Raynaud's syndrome).
Sensory polyneuropathy of vibration origin is characterized by the classic neuropathic type of pain. The pain is of an aching, aching nature, localized in the distal parts of the extremities, often combined with paresthesia, usually occurs spontaneously, and is more pronounced in the morning, at night or after work. According to patients, 10–15 minutes after starting to work with vibrating tools, the pain, as a rule, disappears, and their health improves (symptom of “working in”). The intensity of pain varies (from mild to severe) and depends on the severity of the disease.
Polyneuropathy is most often accompanied by various disorders of surface sensitivity, among which positive and negative sensory symptoms are distinguished.
Positive symptoms include:
- hyperalgesia - intense pain with mild nociceptive irritation of the innervation zone of the damaged area of the nervous system (primary hyperalgesia) or neighboring and even distant zones (secondary hyperalgesia);
- allodynia - the occurrence of pain when exposed to non-painful stimuli of different modalities, which can be contact (tactile/mechanical or temperature allodynia), caused by movement (motor (kinesiogenic) allodynia) or distant (light, sound);
- hyperpathy - a pronounced reaction to repeated painful stimuli with the persistence of a feeling of severe pain after the cessation of painful stimulation;
- spontaneous pain or paresthesia.
Negative symptoms include:
- hypalgesia/anesthesia - decrease/absence of sensation of pain, tactile, temperature, proprioceptive (vibration) sensitivity [5].
Compression-ischemic neuropathy of the median nerve in the wrist (carpal or carpal tunnel syndrome) is accompanied by nightly excruciating arching pain and paresthesia (paresthetic brachialgia) in the hand area, usually in the 1st, 2nd, 3rd fingers. The pain may radiate to the forearm, or less commonly the shoulder. Due to such sensations, patients' sleep is disturbed.
Neuropathic pain is characterized by comorbid disorders, in particular sleep disorders, emotional disorders such as depression and anxiety. It is known that there are complex interactions between pain, sleep and mood, and often these comorbid conditions reinforce each other [3].
Degenerative-dystrophic changes are very characteristic when exposed to local vibration: the musculoskeletal system in the form of osteoporosis, myofibrosis, periarthrosis and arthrosis, accompanied by pain in the muscles and joints of the upper extremities of a nociceptive nature. Thus, the severity and complexity of the pain syndrome in vibration polyneuropathy increases.
Chronic lumbosacral radiculopathy from exposure to general vibration is also characterized by severe pain syndrome, which is based on a combination of nociceptive and neuropathic mechanisms. The LIV, LV, SI roots are most often affected, which determines the specific features of clinical symptoms.
Compression of the LIV root is manifested by pain along the anterior inner surface of the thigh, decreased strength and subsequent atrophy of the quadriceps femoris muscle, loss of the knee reflex.
Compression of the LV root is manifested by pain in the lower back with irradiation along the outer surface of the thigh, the anterior surface of the leg, the inner surface of the foot and big toe. Hypotonia and wasting of the tibialis muscle and decreased strength of the dorsal flexors of the thumb are noted.
The most commonly diagnosed compression of the SI root is manifested by pain in the buttock, radiating along the outer edge of the thigh, lower leg and foot. The strength of the triceps surae muscle decreases, sensitivity in the areas of pain irradiation is impaired, and the Achilles reflex fades.
To objectify the pain syndrome in radiculopathy, electromyography data is used, which is characterized by a decrease in frequency and a decrease in the amplitude of potentials at maximum voltage, and the appearance of fasciculations during a pain test in the case of severe and moderate pain syndrome [9].
Principles of pharmacotherapy of pain syndrome due to vibration disease
Adequate pain control is the most important condition for the treatment of vibration disease. To successfully solve this problem, a differentiated approach to pain pharmacotherapy is required depending on its pathophysiological mechanisms [7].
The main groups of drugs used to combat pain in various vibration disease syndromes are nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, muscle relaxants, antidepressants, anticonvulsants, as well as vascular and desensitizing drugs.
The use of vasodilating drugs helps reduce pain in peripheral angiodystonic syndrome of vibration origin. The most effective drugs for solving this problem are nicotinic acid and pentoxifylline.
Nicotinic acid is a vasodilating, hypolipidemic drug that replenishes vitamin PP deficiency. It has a vasodilating effect, improves microcirculation, increases fibrinolytic activity of the blood and reduces platelet aggregation by reducing the formation of thromboxane A2, and has anti-atherogenic properties. Prescribed 0.05–0.1 g orally or intravenously in the form of a 0.5% solution according to the scheme.
Pentoxifylline (Trental) is a xanthine derivative. The mechanism of its action is associated with the inhibition of phosphodiesterase and the accumulation of cAMP in the cells of vascular smooth muscles and blood cells.
Improves the rheological properties of blood (fluidity) by affecting the pathologically altered deformability of red blood cells, inhibiting platelet aggregation and reducing high blood viscosity. Pentoxifylline improves microcirculation in areas of poor circulation.
Nonsteroidal anti-inflammatory drugs are the main means for relieving nociceptive pain of moderate intensity. Their point of application is peripheral pain receptors.
Selecting a drug from the NSAID group is a complex task, when solving which the following parameters should be taken into account:
- individual characteristics of the drug;
- features of the clinical situation (the nature and severity of the pain syndrome, its dependence on the time of day and load, previous and concomitant therapy, psychological characteristics of the patient);
- safety of treatment;
- cost of treatment.
Of the drugs in this group, diclofenac has proven itself well, which is available in the form of tablets of 50 and 100 mg, rectal suppositories and solutions for parenteral administration. The drug ketorolac has a powerful analgesic effect, which is recommended to be administered for severe pain syndromes at 30 mg intramuscularly for 3–5 days, and then switch to tablet forms, prescribing 10 mg 3 times a day after meals for no more than 5 days.
In addition to those listed above, you can use other drugs in this group: meloxicam (Movalis), lornoxicam (Xefocam), ketoprofen (Ketonal) and others. But it should be remembered that most NSAIDs are contraindicated for peptic ulcers, with a tendency to bleeding. In such cases, the drugs of choice are selective COX-2 inhibitors, which do not have such a significant effect on the gastrointestinal tract. These drugs include celecoxib (Celebrex), which should be prescribed at a dose of 200 mg 3 times a day after meals for 7–10 days.
The use of Meloxicam as a dominant alternative complies with European recommendations and is economically justified within the framework of insurance medicine in the following groups of patients:
- with a high risk of gastrointestinal complications;
- over the age of 65;
- those suffering from cardiovascular diseases;
- taking daily low doses of Aspirin to prevent cardiovascular accidents;
- those requiring long-term or constant use of standard NSAIDs;
- combining the use of various medications;
- patients with a combination of cardiovascular, renal, hepatic pathologies, diabetes mellitus.
Meloxicam in therapeutic concentrations slows down the apoptosis of chondrocytes, inhibits the synthesis of matrix metalloproteinases, and stimulates the synthesis of hyaline cartilage proteoglycans.
To enhance the analgesic effect, a combination of NSAIDs and antihistamines (Tavegil, Diazolin and others) is necessary.
An alternative to NSAIDs in the treatment of patients with chronic pain syndrome is the drug Zinaxin, manufactured using a unique technology based on medicinal plants (two ginger extracts), which has anti-inflammatory, analgesic and chondroprotective properties without the side effects inherent in NSAIDs. Zinaxin is taken orally, 1 capsule 2 times a day with meals.
For radicular pain, the use of the drug flupirtine (Katadolon), which is a selective activator of neuronal potassium channels, is pathogenetically justified.
In terms of its pharmacological effects, the drug is a non-opioid analgesic of central action, which does not cause dependence or addiction; in addition, it has a muscle relaxant and neuroprotective effect. Flupirtine 100 mg (1 capsule) 3-4 times a day is used.
Achieving a muscle relaxant effect is the most important condition for relieving pain in radiculopathy. The main representatives of muscle relaxants are the drugs Mydocalm, Baclofen and Sirdalud.
Baclofen is a GABA receptor agonist that inhibits mono- and polysynaptic spinal reflexes, which leads to a decrease in muscle tension and an analgesic effect. The initial dose is 5 mg 2 times a day after meals, then the dose is increased every 5-7 days until the effect is achieved; the maximum daily dose is 25 mg 4 times a day. It should be discontinued gradually (in susceptible individuals, hallucinations and seizures may occur).
Tizanidine (Sirdalud, Tizanil) is an α2-adrenergic receptor agonist, acting mainly at the level of the spinal cord, reducing the release of excitatory amino acids from interneurons and selectively suppressing polysynaptic mechanisms responsible for muscle hypertonicity. For painful muscle spasms, 2 mg 3 times a day is prescribed, with the dose increasing if the effect is insufficient to 8–12 mg/day (in 3 doses). The maximum dose is 36 mg/day.
Tolperisone (Mydocalm) is a centrally acting muscle relaxant. Inhibits the conduction of impulses in primary afferent fibers and motor neurons, which leads to blocking of spinal mono- and polysynaptic reflexes. Reduces excess Na+ entry into the cell by blocking voltage-dependent sodium channels, thereby reducing pathologically increased impulses and reducing the severity of pain. Inhibits the release of mediators by inhibiting the entry of Ca2+ into synapses. Has a local anesthetic effect. Increases peripheral blood flow. A weak antispasmodic and adrenergic blocking effect plays a role in the development of this effect, which makes it possible to additionally combat pain.
It is administered orally at an initial dose of 50 mg 2 times a day, the maximum dose is 150 mg 3 times a day, intramuscularly - 100 mg 2 times or intravenously - 100 mg 1 time a day.
Adequate control of pain in polyneuropathy is a difficult task, since neuropathic pain, unlike nociceptive pain, is difficult to treat with conventional analgesics and non-steroidal anti-inflammatory drugs.
According to the recommendations of the European Federation of Neurological Societies (EFNS), the drugs of choice for the treatment of neuropathic pain syndromes are anticonvulsants and antidepressants, and in some situations, local anesthetics and opioid analgesics.
Antidepressants have a moderate effect in chronic pain of any origin, but they occupy a particularly important place in the treatment of neuropathic pain.
It is assumed that the analgesic effect of antidepressants is associated with increased activity of noradrenergic and, to a lesser extent, serotonergic systems, which have an inhibitory effect on the transmission of pain impulses along nociceptive pathways in the central nervous system.
The analgesic effect usually develops faster than the antidepressant effect, often occurring at significantly lower doses.
Tricyclic antidepressants have the highest analgesic activity and are the first choice drugs for neuropathic pain.
The most widely used are amitriptyline and imipramine (Melipramine).
Amitriptyline is usually initially prescribed at a dose of 10 mg at night, then the dose is gradually increased by 10–25 mg every 7 days until the effect is achieved (maximum 150 mg/day). The daily dose is taken once at night or divided into 2-3 doses. Although amitriptyline is effective in approximately 70% of patients with neuropathic pain, excessive sedation, pronounced anticholinergic effects (dry mouth, constipation, urinary retention, etc.), adverse effects on the cardiovascular system (hypotension, tachycardia) limit the use drug. Imipramine has a less pronounced sedative effect.
Selective serotonin reuptake inhibitors (SSRIs): sertraline (Zoloft), citalopram (Cipramil), escitalopram (Selectra), fluoxetine (Prozac), fluvoxamine (Fevarin), paroxetine (Paxil) - cause fewer side effects, but also have less distinct pain relief effect, which may be explained by the lack of a direct effect on noradrenergic transmission. SSRIs are indicated mainly in cases where pain is associated with depression, and the patient does not tolerate tricyclic antidepressants.
The mechanism of action of anticonvulsants in neuropathic pain remains unclear. Perhaps it is associated with inhibition of the ectopic generation of nerve impulses in partially damaged nerve fibers. Controlled studies have shown that anticonvulsants reduce pain by at least half in more than 50% of patients with neuropathic pain.
The most commonly used anticonvulsants in clinical practice are gabapentin (Neurontin), pregabalin (Lyrica) and carbamazepine (Finlepsin). Gabapentin is a structural analogue of GABA, but its mechanism of action is explained by the interaction of the drug with the alpha2?delta subunit of voltage-gated calcium channels. This leads to a decrease in the release of mediators such as glutamate and substance P, and inhibition of the passage of nociceptive impulses at the level of the spinal cord.
The starting dose of gabapentin is 100–300 mg at night. Then the daily dose is gradually increased every 3-5 days by 100-300 mg, moving to a three-time dose. The average effective dose is 1800 mg/day (600 mg 3 times a day). The maximum dose is 3600 mg/day (1200 mg 3 times a day). Titration of the gabapentin dose can last from 2 to 8 weeks. Before concluding that the drug is ineffective, its maximum tolerated dose should be taken for 1–2 weeks. In addition to reducing pain, the drug can help normalize night sleep, however, some patients may develop unwanted drowsiness, so it is recommended to prescribe most of the dose at night.
Among opioid analgesics, a synthetic drug, tramadol hydrochloride (Tramal), is widely used to relieve neuropathic pain. Its analgesic effect has a dual mechanism of action.
Some tramadol molecules activate analgesic μ-opioid receptors. The second part of tramadol molecules simultaneously activates non-opioid analgesic systems (inhibits the reuptake of serotonin or norepinephrine at nerve synapses). It is the synergism of the two mechanisms of action of tramadol that determines its high effectiveness.
Treatment begins with a dose of 50 mg at night (or 25 mg 2 times a day), after 5–7 days the dose is increased to 100 mg/day, switching to a double dose of the drug. If necessary, the dose is increased to 100 mg 2–4 times a day (maximum dose 400 mg/day).
Although the risk of drug dependence with tramadol is lower than with other opioids, a similar danger exists with long-term use.
Local anesthetics, such as lidocaine, along with anticonvulsants, are drugs that stabilize cell membranes. The mechanism of action of drugs of this class is mediated by blockade of sodium channels, associated with the suppression of ectopic spontaneous generation of impulses in damaged nerve fibers and blockade of non-synaptic transmission of excitation from one fiber to another.
Skin patches with 5% lidocaine are easy to use (apply 1 to 3 patches at a time for no more than 12 hours a day).
Recommended doses of drugs used to relieve neuropathic pain are presented in Table.
Although the number of medications simultaneously taken by the patient should be limited as much as possible, in some cases, for neuropathic pain, a combination of two or more drugs with different mechanisms of action is advisable.
Chronic neuropathic pain is often accompanied by mood symptoms and sleep disturbances, the interaction of which forms a kind of vicious circle. In this regard, when treating pain, special attention should be paid to normalizing sleep and the affective status of patients.
The use of pathogenetic therapy (vitamins, antioxidants, neuroprotectors, anticholinesterase drugs) is important in the treatment of polyneuropathy, which helps not only to restore the function of the affected nerves, but also to reduce pain.
Literature
- Artamonova V. G., Mukhin N. A. Occupational diseases. 4th ed., revised. and additional M.: Medicine. 2004. 480 p.
- Izmerov N.F., Bukhtiyarov I.V., Prokopenko L.V. Issues of occupational morbidity: retrospect and modernity / Materials of the XI All-Russian Congress “Profession and Health”, Moscow, November 27–29, 2012. 36 p.
- Zhulev N. M. Neuropathies. St. Petersburg: SPbMAPO, 2005. 416 p.
- Lagutina G. N., Prokopenko L. V., Rudakova I. E. Vibration disease in modern conditions / Materials of the II All-Russian Congress of Occupational Pathologists. Rostov-on-Don, 2006. pp. 186–188.
- Levin O. S. Polyneuropathy. M.: Med. information agency, 2005. 496 p.
- Order of the Ministry of Health and Social Development of the Russian Federation dated April 27, 2012 No. 417n “On approval of the list of occupational diseases.”
- Shukhov V.S. Pain. Clinical recommendations for the management of patients with various pain syndromes // RMZh. 2004. T. 12, No. 7. P. 437.
- Yanshina E. N. Occupational autonomic-sensory polyneuropathy of the hands from exposure to local vibration and physical stress in workers in modern production conditions. Author's abstract. diss. doc. honey. Sci. M., 2005. 90 p.
- Magy L, Gallouedec G. et al. // J. Peripher. Nerv. Syst. 2005. Vol. 10, No. 3. P. 329–337.
- Leger JM, Behin A. Multifocal motor neuropathy // Curr. Opin. Neurol. 2005. Vol. 18, No. 5. P. 567–573.
S. A. Babanov, Doctor of Medical Sciences, Professor T. A. Azovskova, Candidate of Medical Sciences, Associate Professor N. E. Lavrentyeva1, Candidate of Medical Sciences, Associate Professor
Federal State Budgetary Educational Institution of Higher Education SamSMU Ministry of Health of the Russian Federation, Samara
1 Contact information
Clinical types of the syndrome
Posterior cervical sympathetic syndrome (Barre–Lieu)
Posterior cervical syndrome is characterized by headaches localized in the cervical-occipital region with radiation to the front of the head. The headache is usually constant, often in the morning, especially after sleeping on an uncomfortable pillow. Headache may occur when walking, driving a car, or when moving the neck. The headache can also be pulsating, piercing, localized in the cervical-occipital region and radiating to the parietal frontal and temporal zones. Headache may intensify when turning the head and is accompanied by vestibular, visual and autonomic disorders.
Migraine basilar
Basilar migraine does not result from compression of the vertebral artery, but from stenosis of the vertebral artery, but clinically has much in common with other forms of vertebral artery syndrome. As a rule, a migraine attack begins with a sharp headache in the back of the head, vomiting, and sometimes loss of consciousness. Visual disturbances, dizziness, dysarthria, and ataxia are also possible.
Vestibulo-cochlear syndrome
Disturbances from the hearing system manifest themselves in the form of noise in the head, decreased perception of whispered speech and are recorded by changes in data during audiometry. Tinnitus is persistent and long-lasting and tends to change when the head moves. Cochlear disorders are associated with dizziness (both systemic and non-systemic).
Ophthalmic syndrome
With ophthalmic syndrome in the foreground, visual disturbances such as scintillating scotoma, decreased vision, photopsia may also be symptoms of conjunctivitis (lacrimation, conjunctival hyperemia). Loss of visual fields can be episodic and is mainly associated with changes in head position.
Autonomic change syndrome
As a rule, autonomic disorders do not appear in isolation, but are combined with one of the syndromes. Autonomic symptoms are usually the following: a feeling of heat, a feeling of cold extremities, sweating, changes in skin dermographism, sleep disturbances.
Transient ischemic attacks
Ischemic attacks can occur during the ischemic stage of vertebral artery syndrome. The most common symptoms of such attacks are: transient motor and sensory disturbances, visual disturbances, hemianopsia, ataxia, attacks of dizziness, nausea, vomiting, speech impairment, swallowing, double vision.
Syncopal vertebral syndrome (Unterharnscheit syndrome)
An episode of syncopal vertebral syndrome is an acute circulatory disorder in the area of the reticular formation of the brain. This episode is characterized by a short-term loss of consciousness when turning the head suddenly.
Drop attack episodes
An episode of a drop attack (fall) is caused by impaired blood circulation in the caudal parts of the brainstem and cerebellum and will clinically manifest itself as tetraplegia when the head is thrown back. Restoration of motor functions is quite rapid.
Diagnostics
Diagnosis of vertebral artery syndrome presents certain difficulties and both overdiagnosis and underdiagnosis of vertebral artery syndrome often occur. Overdiagnosis of the syndrome is often due to insufficient examination of patients, especially in the presence of vestibulo-atactic and/or cochlear syndrome, when the doctor fails to diagnose diseases of the labyrinth.
To establish a diagnosis of vertebral artery syndrome, 3 criteria must be present.
- The presence in the clinic of symptoms of one of 9 clinical options or a combination of options
- Visualization of morphological changes in the cervical spine using MRI or MSCT, which may be the main reasons for the development of this syndrome.
- The presence of changes in blood flow during ultrasound examination when performing functional tests with flexion - extension of the head and rotation of the head.
Treatment
Treatment of vertebral (vertebral) artery syndrome consists of two main areas: improving hemodynamics and treating diseases that lead to compression of the vertebral arteries.
Drug treatment
Anti-inflammatory and decongestant therapy is aimed at reducing perivascular edema resulting from mechanical compression. Drugs that regulate venous outflow (troxerutin, ginkgo biloba, diosmin). NSAIDs (Celebrex, lornoxicam, celecoxib)
Vascular therapy is aimed at improving blood circulation in the brain, since hemodynamic disturbances occur in 100% of patients with this syndrome. Modern diagnostic methods make it possible to evaluate the effectiveness of treatment with these drugs and the dynamics of blood flow in the vessels of the brain using ultrasound examination. The following drugs are used for vascular therapy: purine derivatives (trental), vinca derivatives (vincamine, vinpocetine), calcium antagonists (nimodipine), alpha-blockers (nicergoline), instenon sermion.
Neuroprotective therapy
One of the most modern areas of drug treatment is the use of drugs to improve energetic processes in the brain, which allows minimizing neuronal damage due to episodic circulatory disorders. Neuroprotectors include: cholinergic drugs (citicoline, gliatiline), drugs that improve regeneration (Actovegin, Cerebrolysin), nootropics (piracetam, Mexidol), metabolic therapy (mildronate, Thiotriazoline, Trimetazidine)
Symptomatic therapy includes the use of drugs such as muscle relaxants, antimigraine drugs, antihistamines and others.
Treatment of degenerative diseases includes non-drug treatment methods, such as exercise therapy, physiotherapy, massage, acupuncture, and manual therapy.
In most cases, the use of complex treatment, including both drug and non-drug treatment, can reduce symptoms and improve blood circulation in the brain.
Surgical treatment methods are used in cases where there is severe compression of the arteries (disc herniation, osteophyte) and only surgical decompression can achieve a clinical result.
Causes of astheno-neurotic syndrome
The condition is provoked by many etiological factors. Infectious or somatic pathologies cause asthenia, which for children with unstable mental health is fraught with exhaustion. The prerequisites for asthenoneurosis include too much workload of the child both at school and outside its walls. The risk of developing the syndrome increases with poor social adaptation and an unhealthy family environment. The main provocateurs of the disease are:
- disorders of intrauterine brain development due to hypoxia, bad habits of a pregnant woman;
- head injuries;
- infectious diseases, chronic kidney or liver pathologies;
- vitamin B deficiency;
- overvoltage;
- hormonal disorders;
- stress due to fear, tragic events;
- features of upbringing and temperament.