Sometimes patients complain of wandering pains throughout the body of varying intensity; they can suddenly appear and disappear regardless of the time of day. There is no such disease in ICD 10; symptoms are usually provoked by various pathologies or disorders that occur in a latent or subacute stage. Often clients come to a traumatologist and ask why their arms and legs are numb, and in such cases a consultation with a neurologist is needed. But migrating muscle pain can be cured by a therapist. Diagnostics will help determine the provoking factor.
Having pain in your vagina?
If you have unpleasant, painful sensations in the vagina, diagnosing yourself, let alone taking measures, prescribing treatment is very dangerous. You need to urgently undergo examination by a gynecologist. Often, all sorts of folk remedies will not only not improve the situation, but will even worsen it .
Only a doctor can carry out the necessary tests and, based on them, make an accurate diagnosis and prescribe treatment.
Before being examined by a doctor, you should not douche, use suppositories or other medications. After using them, the test results will be incorrect and it will be difficult to choose the right treatment.
Causes of pain, itching, burning in the vagina
There are three groups of reasons
that cause discomfort in the vagina:
- Gynecological diseases;
- Non-gynecological diseases;
- External and internal factors;
Inflammation of the mucous membrane is caused by the development of pathogenic microflora in the genitals, which causes itching in the vagina. The most common infections include gardnerellosis, candidiasis (thrush), etc. This condition is called bacterial vaginosis, and it often becomes a consequence of intestinal dysbiosis.
Pain, itching, burning may be symptoms of an STI
(sexually transmitted infections):
- chlamydia (yellowish discharge with a fishy odor);
- trichomoniasis (excessive foamy greenish discharge);
- genital herpes, etc.
Itching in the vagina can be caused by allergies, for example to contraceptives or sanitary pads. Lack of genital hygiene, tight underwear, and unnecessary douching disrupt the balance of vaginal microflora and cause itching.
External factors
that can cause itching:
- overheating or hypothermia;
- mechanical impact (friction against laundry);
- mechanical damage to the mucous membrane (for example, during rough sexual intercourse);
- emotional stress;
- stress, feeling of fear.
In any case, whatever the reason, if you have these symptoms, you should consult a gynecologist.
Causes of wandering pain
When all the muscles, bones and joints of the whole body hurt, the search for the causes begins with a visit to the doctor. But in order to know which doctor to go to, you need to take into account the presence of chronic diseases, previous infections or a predisposition to the development of various pathologies.
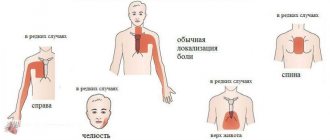
All provoking factors may be common and characteristic of a specific localization of the symptom. Most often, the causes of wandering pain throughout the body are systemic disorders and pathologies:
- physical overload and muscle strain;
- previous acute respiratory viral infections or infectious poisonings;
- postural disorders and spinal diseases;
- muscle inflammation due to hypothermia;
- constant stress and neuroses;
- various chronic diseases (diabetes mellitus, rheumatism, arthritis, etc.).
These are the most common causes of the symptom. It is possible to determine why the muscles of the whole body hurt only by conducting instrumental diagnostics and examination. Before going to the doctor, you need to assume a provoking factor that may cause pain. To do this, you need to take into account its localization and manifestations.
How is a gynecologist examined?
At the Alan Clinic medical center, gynecological examinations are performed in comfortable conditions, using disposable sterile instruments. The initial appointment takes 40 minutes.
The initial examination by a gynecologist includes a standard gynecological examination, including:
- conversation with a doctor
- smear of vaginal discharge to determine the degree of purity
Depending on the clinical symptoms and complaints, the gynecologist may prescribe additional examination methods.
- scraping from the cervix for oncocytology
- Ultrasound of the pelvic organs
- extended colposcopy
- study for tumor markers CA-125, CA-15-3
Calf pain: differential diagnosis
Pain in the calf muscle (calf) is a universal symptom that can occur with a large number of diseases.
The main muscle mass of the posterior surface of the leg (calf) is formed by two muscles - the superficially located gastrocnemius muscle and the more deeply located soleus muscle. The tendons of these muscles come together and attach to the heel bone, forming the so-called. Achilles tendon. The calf muscles provide movement in the ankle joint (flexion and extension), which is necessary for walking, maintaining body balance in an upright position and shock absorption during movements. The arterial blood supply to the gastrocnemius muscle comes from its own arteries, originating from the popliteal artery. Venous outflow is carried out through the veins accompanying the arteries, which in the thickness of the muscle form wide cavities lined with endothelium - sural sinuses. The above muscles are innervated from the tibial nerve (L3-4).
Chronic venous insufficiency.
Today, in the genesis of pain in chronic venous diseases, three main components are distinguished: distensional, ischemic and inflammatory.
The distension component occurs due to overstretching of the venous wall by excess blood when the mechanisms of its outflow are disrupted. Such disorders may be a consequence of dysfunction of the muscular-venous pump, which plays a leading role in ensuring venous outflow in the vertical position of the body. Stagnation of blood in the veins of the leg can occur as a result of decreased activity of the calf muscles, for example, due to prolonged stay in a stationary vertical or sitting position, as a result of damage to the valve apparatus of the superficial (varicose veins) or deep (post-thrombotic syndrome) veins, which is accompanied by a disruption of the normal centripetal movement of blood and its throwing into the distal sections with each muscle contraction (reflux), as well as with damage to the corresponding muscles and adjacent joints. Such pain often occurs after prolonged static loads and is easily relieved by night rest and/or by placing the limbs in an elevated position.
The inflammatory component is a reflection of the currently generally accepted concept of leukocyte aggression as a leading component in the pathogenesis of chronic venous diseases. Its essence lies in the fact that when the speed of venous outflow decreases and signs of venous stasis appear in the veins of the leg, leukocyte-endothelial interaction occurs with the expression of corresponding adhesive molecules on the cell surface, which leads to the migration of white blood cells into the thickness of the vascular wall and their degranulation. Released oxygen free radicals, proteolytic enzymes and cytokines not only have a damaging effect on the structural components of the venous wall, primarily the collagen framework, but also activate non-myelin C-nociceptors, which are responsible for transmitting the pain impulse. Thus, the inflammatory component of venous pain reflects not only stagnation of blood in the veins of the leg, but also the process of active development of chronic venous diseases, which can ultimately lead to the appearance of varicose veins. The addition of an inflammatory component makes venous pain more persistent and not relieved by elevated position of the limb and night rest.
The ischemic component is associated with severe inflammatory changes in the venous wall with desolation of the vasa vasorum, which leads to serious morphological restructuring of the affected veins. It should be assumed that the ischemic component occurs in severe forms of chronic venous diseases and can cause constant pain in the varicose nodes themselves.
Classic pain in venous insufficiency is dull, arching in nature, intensifies after a long stay in a standing or sitting position, decreases or disappears completely after an overnight rest or placing the limb in an elevated position. Often the pain is accompanied by transient swelling of the soft tissues in the lower third of the leg and cramps of the calf muscle at night.
Acute venous insufficiency – deep vein thrombosis of the leg. As a result of a sudden difficulty in venous outflow from the lower extremities and the development of acute venous congestion, very intense constant bursting pain in the calf muscle can be observed, slightly decreasing when the limb is elevated, accompanied by an increase in the volume of the muscle and its thickening, cyanosis of the skin and an increase in the subcutaneous vascular pattern. The severity of symptoms will depend on the location of the thrombosis - the more veins are involved in the process, the more acute the manifestations will be. With isolated thrombosis of the sural sinuses, moderate intensity, clearly localized pain may be observed, intensifying with plantar flexion of the ankle joint and with pressure on the site of the sinus projection on the skin.
Chronic arterial insufficiency develops as a result of occlusion of the arteries by an atherosclerotic or autoimmune-inflammatory process. In such cases, the muscles experience oxygen starvation and switch to the anaerobic metabolic pathway, which leads to the accumulation of acidic products that irritate pain receptors. In case of arterial insufficiency, pain in the calf muscles is observed when walking and forces the person to stop (intermittent claudication syndrome); in the initial stages of the process, pain does not bother them at rest. The pain is accompanied by coldness of the extremities, chilliness, the skin becomes pale, flaky, easily vulnerable, and hair loss. As the disease progresses, the muscles and subcutaneous tissue become thinner.
Acute arterial insufficiency - sudden blockage of the arteries due to thrombosis or embolism leads to acute ischemia of the limb. In this case, pain in the calf muscle will be observed at rest, be intense, accompanied by disturbances in sensitivity and motor function, up to the development of paralysis and muscle contracture.
Osteochondrosis of the lumbar spine (radicular syndrome) is the second most common cause of pain in the calf muscles. It is based on compression of the spinal nerve root at its exit from the spinal canal. As a result, projected pain occurs in the place where the nerve fibers go - including in the calf area. In this case, pain can be associated both with compression of the nerves and the generation of pain impulses in them, and with tonic muscle contraction and the subsequent development of fibro-dystrophic changes in muscle tissue. With radicular syndrome, pain is associated with certain movements and changes in body position (for example, bending the torso forward, to the sides, flexing a limb at the hip joint). As a rule, pain intensifies with prolonged stay in the provoking position and decreases after warm-up, physical therapy, massage, and thermal effects. With muscular-tonic syndrome, it is possible to detect areas of increased tone in the water of dense, painful foci in the jejunum of the muscle. Over time, the muscle may become diffusely denser due to the development of fibrotic changes in it. Subsequently, due to a violation of the autonomic innervation, a congestive (vasodilation) or ischemic (vasoconstriction) component of the pain syndrome may occur.
Peripheral polyneuropathy can be a complication of diabetes mellitus, a consequence of the toxic effects of ethyl alcohol on the body, etc. Diabetic polyneuropathy is characterized by a combination of night or morning pain at rest, localized in the distal parts of the lower extremities, with crawling sensations, burning, numbness, muscle weakness and decreased skin and (primarily) vibration sensitivity. In this case, the pain can be very intense. Damage to the autonomic nerves can lead to trophic disorders and the addition of the vascular component of the pain syndrome. Neuritis of the tibial nerve is characterized by paroxysmal pain that occurs along the nerve fibers. In this case, in the intervals between attacks, pain is completely absent.
The pathology of the knee joints - primarily osteoarthritis - is characterized by pain in the periarticular area during exercise. The pain is localized mainly in the area of the anterior and inner surfaces of the knee joint, and intensifies with prolonged stay in an upright position of the body, with long walking. Particularly characteristic is increased pain when climbing and especially descending stairs. In the initial stages of the disease, the pain completely disappears with rest (there is no need to elevate the limb). With the development of active inflammation, pain may appear at the beginning of movement and morning stiffness in the joints. During the development of the disease, it is possible that a muscular-tonic component of the pain syndrome may occur, in which the calf muscle is in constant tension and becomes dense and painful on palpation. When effusion accumulates in the joint cavity, limited accumulations can form in the inversions of the joint capsule - Becker cysts, which can aggravate the pain syndrome, compress nerves and veins with the development of a neuropathic and vascular component.
Dermatomyositis, polymyositis is an autoimmune inflammation of muscle tissue, characterized by constant dull persistent pain, aggravated by movements in the ankle joint, combined with muscle weakness and symptoms of intoxication. The muscles become swollen, painful on palpation; over time, they may become thickened, heaviness, nodularity, fibrosis, the formation of calcifications, up to complete atrophy. In autoimmune diseases, as a rule, lesions of other organs and systems, primarily the skin, are detected: erythema and swelling of the periorbital area, scaly erythema of the fingers and hands, redness of the periungual ridges, foci of hyperpigmentation-depigmentation of the skin - with dermatomyositis; swelling-induration-atrophy of the skin in scleroderma, erythema on the face, damage to the kidneys, heart in lupus, etc. Meanwhile, damage to the calf muscles in autoimmune myositis is uncommon.
Myositis can also be a manifestation of cancer, parasitic diseases (trichinosis, toxoplasmosis, cysticercosis) or be a complication of a cold, injury or overstrain of the calf muscle.
Fibromyalgia , a chronic autoimmune disease of muscle tissue, is rarely accompanied by isolated pain in the calf muscles. Intense constant pain and severe muscle weakness in the proximal muscles of the limb girdles are more often observed. There is also prolonged morning stiffness and pain in specific points upon palpation.
Overstrain, sprain, or muscle rupture can be accompanied by severe intense pain in the damaged area, which sharply intensifies when attempting to move. Inflammatory phenomena (myositis) may occur.
Gynecologists in Kazan use the following methods of treating gynecological diseases:
- Drug treatment . Prescribed in accordance with test results.
- Local treatment . Sanitation of the vagina followed by application of a tampon with a medicinal drug, incl. Ultrasonic sanitation with the Gineton apparatus.
- Physiotherapy . Modern Androgyn and Mustang equipment is used, which are successfully used in the complex treatment of inflammatory diseases, hormonal disorders, as well as recovery in the postoperative period.
- Pharmacopuncture . Introduction to acupuncture points of medicinal substances that are indicated for various diseases (inflammatory, hormonal disorders, etc.).
- Ozone therapy
. Intravaginal and intravenous administration of drugs enriched with ozone contributes to the development of a powerful antioxidant effect, which can successfully cure inflammatory diseases, improve the immune system and reactive capabilities of the body. - Hirudotherapy . Widely used in the treatment of diseases such as endometriosis of the uterus and ovaries, inflammatory diseases, hormonal dysfunctions, infertility, etc.