Heart pain bothers every second person. They can be caused by various reasons and factors. For example, heredity, stress and emotional stress, physical stress, pressure changes. Pain in the heart area when taking a deep breath has also become a common problem today. This symptom bothers the patient, makes him worry and disrupts the normal functioning of the entire body.
Pain in the heart when inhaling can have different intensity, character and frequency. Most often, patients notice a cutting, pulling and sharp character, which continues with short pauses. Why does my heart hurt when I inhale? To answer this question, you should visit a doctor and conduct a full diagnosis of the body. Often such symptoms indicate the development of diseases of other organs. We recommend having a comprehensive examination at the KDS Clinic.
Heart hurts: types of pain
Pain in the heart area is not always the same.
They depend on the cause that causes them, as well as on the individual characteristics of the person. According to statistics, in 2021, more than 11.4 thousand new cases of only cardiac causes of chest pain were recorded in the Russian Federation, not counting diseases of other organs and systems.
How to understand what causes chest pain
The nature of the symptoms can sometimes indicate the cause of the pain. However, it is always better to consult your doctor. You can also take a short quiz to help you better understand the problem.
Sharp pain
Sharp, sudden pain in the heart most often occurs after exposure to a trigger, such as physical activity or emotional shock. Its duration depends on the provoking factor and can vary from 5-15 minutes during an attack of angina pectoris, to several hours during intercostal neuralgia. As a rule, such pain then completely disappears.
Acute pain
Acute pain in the heart includes strong, burning pain that occurs at rest or after exposure to a trigger. As a rule, a person becomes restless and a feeling of fear arises. The most common causes of acute pain in the heart are myocardial infarction and pulmonary embolism.
Stitching pain
Stitching pain behind the sternum, in contrast to sharp and acute pain, is less often accompanied by a significant disturbance in the general condition of a person. However, most often, it is also a sign of damage to the cardiovascular system, including: attacks of stable angina, inflammation of the heart and its membranes (myocarditis, pericarditis, endocarditis), valve defects, as well as psychogenic cardialgia.
Blunt pain
Dull pain in the cardiac region persists for a long time and allows you to perform everyday activities. When exposed to physical activity, it can worsen, become sharp or stabbing. The main causes are chronic heart diseases (for example, cardiomyopathies and heart failure that occur against the background of arterial hypertension), damage to the intercostal nerves and the spinal column in the thoracic region.
Pain when moving
A separate option is pain that occurs during movement (for example, bending the body to the sides or lifting weights) and disappears at rest. As a rule, it is rarely associated with other symptoms and indicates pathology of the musculoskeletal system in the thoracic region.
Pain when taking a deep breath
A type of pain syndrome in which discomfort and pain arise or worsen at the moment of deep inspiration. Most often it is associated with lesions of the bone frame of the chest and peripheral nerves in this area (for example, rib fractures and trauma to the intercostal nerves), as well as diseases of the respiratory system, including pulmonary embolism (PE).
Chest pain: is it always the heart?
It can be a sign of life-threatening conditions, so it is important to know its main characteristics in order to promptly seek medical help. Pain in the heart area. What is it like? Is it always an indicator of heart pathology?
Natalya Aleksandrovna Shelest, a cardiologist at Clinic Expert Irkutsk, talks about the characteristics of pain in the heart area and the possible causes of their occurrence.
— Natalya Alexandrovna, is chest pain always a sign of cardiac pathology?
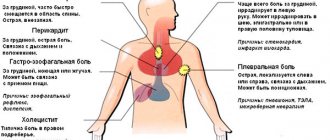
- No not always. Chest pain, along with diseases of the cardiovascular system, can also manifest as diseases of the bones, joints, muscles (Tietze syndrome, anterior scalene muscle syndrome, fibromyositis, dorsopathy), changes in the lungs and pleura (pleurisy, spontaneous pneumothorax, pulmonary infarction, tumors ), digestive tract organs (esophagitis, cardiospasm, diaphragmatic hernia, gastric and duodenal ulcers, cholecystitis), some neurological disorders (herpes zoster, neurocirculatory dystonia), breast diseases.
Among the pathologies that cause chest pain, there are both life-threatening ones that require immediate intervention (in particular, myocardial infarction, dissecting aortic aneurysm, thromboembolism of the pulmonary artery and its branches, pneumothorax), and less serious pathologies - for example, anterior chest wall syndrome , anxiety-depressive state. They, of course, also require correction, but they are not classified as emergency conditions.
— For what reasons can true pain in the heart appear?
— The cause of such pain can be increased blood pressure, increased heart rate, heart rhythm disturbances, and excessive physical and emotional stress. Alcohol abuse, smoking, large meals, and drug use can also cause heart pain.
— If a patient complains of pain in the heart when taking a deep breath, what could this mean?
— First of all, about diseases of the musculoskeletal system - intercostal neuralgia, fibromyalgia, inflammation of the sternocostal joints (Tietze syndrome), chest injuries. The appearance of pain in the heart area in these pathologies is caused by irritation or pinching of the intercostal nerves, excursion (movement) of the chest as a result of the act of inhalation and exhalation, and changes in body position.
A number of pulmonary diseases, such as pneumothorax, pleurisy, pneumonia, can also be accompanied by pain when inhaling; often additional symptoms are fever, shortness of breath and tachycardia.
— What if pain in the heart appears at rest?
— In this case, there is a high probability of developing serious pathology, in particular, dissecting aortic aneurysm, pulmonary embolism, cardiac tamponade.
Sometimes banal muscle pain in the chest can also bother a person at rest due to excessive static loads or incorrect position of the torso.
— Which doctor should you consult for pain in the heart area?
— If pain in the heart occurs for the first time, taking you by surprise, and is accompanied by a deterioration in health, a person should immediately contact any doctor nearby and explain what is bothering him. Regardless of qualifications and specialization, each doctor is able to figure out what to do in a particular case, provide first aid if necessary and refer to the right specialist.
If the patient can get to the clinic, he should contact a therapist. He will decide on the necessary stages of medical care, including consultation with specialized specialists - a cardiologist, gastroenterologist, neurologist, surgeon and other doctors.
— What characteristics of chest pain require emergency medical care?
— Chest pain should always be treated with caution. It is important not to miss conditions such as acute coronary syndrome, an attack of angina pectoris (popularly “angina pectoris”). They are characterized by paroxysmal compressive, bursting, pressing, burning pain behind the sternum and/or in the left half of the chest (precordial region), can spread to the axillary and subscapular region on the left, to the left arm and shoulder, to the left half of the neck and lower jaw, lasting no more than 10 minutes, may be accompanied by a feeling of lack of air, shortness of breath. It should be remembered that most often these symptoms appear against the background or immediately after physical or emotional stress. There is a rapid effect from taking nitroglycerin within 5 minutes.
If these pains last more than 20 minutes and intensify with renewed exercise, you should definitely call an ambulance. A dangerous condition is also considered a combination of these pains with a decrease in blood pressure, a decrease (less than 50 beats per minute) or an increase (more than 120 beats per minute) in the heart rate, with interruptions in heart rhythm, profuse cold sweating, pallor of the skin, severe weakness, nausea, lightheadedness, or even loss of consciousness. If these symptoms are present, the patient needs immediate medical attention.
— How is diagnosis done for heart pain?
- First of all, we evaluate vital functions - we determine whether the patient is conscious, what are the indicators of breathing, hemodynamics (blood circulation). If there are signs of breathing problems, very low or high blood pressure, or heart rhythm disturbances, then emergency help is needed: calling an ambulance and urgent hospitalization.
The second stage of diagnosis is to identify risk factors for coronary heart disease. If there is angina-type pain, the patient is given a nitroglycerin tablet under the tongue, an electrocardiogram (ECG) is taken, and the clinical effect of the drug taken is assessed. If there is a suspicion of pulmonary embolism, pneumothorax, dissecting aneurysm, it is necessary to take an ECG, perform echocardiography, determine markers of myocardial damage, take a chest X-ray, and assess blood oxygen saturation.
At the next stage of diagnosis (after excluding life-threatening pathologies), they move on to searching for other causes that can cause pain in the heart area. In this case, the complaints are detailed, a more thorough examination is carried out, an algorithm for laboratory and instrumental research is developed: blood tests, Holter ECG, 24-hour blood pressure (BP) monitoring, radiography of the chest and spine, ultrasound of the abdominal organs, fibrogastroduodenoscopy, if necessary CT scan.
— Natalya Alexandrovna, tell our readers about the tactics of treating pain in the heart area.
— Pain in the heart area can occur with a number of pathologies, both cardiac and non-heart related. Therefore, therapeutic measures will depend on the background of what disease these pains are observed.
If pressing, bursting, burning pain in the chest appears, arising from physical or emotional overload, or at rest (which happens much less frequently), it is necessary to stop any load, take a sitting position with your legs down (to reduce the venous return of blood to the heart) and call an ambulance.
You can make an appointment with specialists at Clinic Expert Irkutsk here
The editors recommend:
Help your heart beat. How did the history of the pacemaker begin? Founder of electrocardiography. Who was Willem Einthoven?
For reference:
Shelest Natalya Alexandrovna
In 2000, she graduated from Irkutsk State Medical University with a degree in General Medicine.
In 2001, she completed her internship at the Irkutsk Institute for Advanced Training of Physicians in Therapy.
In 2002, she received a certificate of professional retraining in cardiology.
He holds the position of cardiologist at Clinic Expert Irkutsk. Receives at the address: st. Kozhova, 9a.
THERE ARE CONTRAINDICATIONS. SPECIALIST CONSULTATION IS REQUIRED
How does pain manifest when inhaling?
This can range from mild discomfort to severe pain localized behind the sternum (Fig. 1). As a concomitant symptom, shortness of breath often appears - the inability to take a normal breath and/or exhale. Horizontal position of the body, playing sports or emotional stress can aggravate pain and shortness of breath, causing a feeling of lack of air.
Figure 1. Chest pain when inhaling. Source: MedPortal
Causes of the combination of pain and shortness of breath
Many factors affect your heart rate, breathing rate, and blood pressure readings. The main participants in regulation are the sympathetic and parasympathetic nervous systems, endocrine glands, and vascular receptors. A disruption in the functioning of one of these structures is indicated by increased blood pressure, symptoms of cardialgia and difficulty breathing. If you are worried about aching pain in the heart and there is not enough air, doctors understand the cause, since the situation can indicate many diseases. Patients with chronic cardiovascular pathology (diabetes, hypertension, coronary artery disease) should be more attentive to their health status when such signs appear. In such people, stabbing pain in the heart and shortness of breath may be associated with the following diseases:
- acute coronary syndrome, heart attack;
- inflammation of one of the cardiac membranes of the heart, pericardium, myocardium or endocardium;
- cardiomyopathy with severe hypertrophy of the heart;
- spasm of the coronary vessels against the background of ischemic disease, acute attack of circulatory failure;
- acute attack of angina after walking;
- a sharp increase in blood pressure, hypertension;
- complicated hypertensive crisis;
- pathology of the heart valve apparatus;
- bronchial asthma, severe broncho-obstructive syndrome;
- severe pneumonia, inflammation of the pleura of the lungs against the background of fever;
- pathology of the autonomic nervous system, neurocirculatory dystonia, VSD.
Breathing problems occur in patients with psychosomatic disorders and vegetative-vascular dystonia.
People who drink alcohol or use stimulants are especially susceptible to panic attacks. With this pathology, difficulty breathing is not accompanied by pain in the heart. However, a feeling of sudden fear causes neurotic shortness of breath, which occurs as a result of frequent deep breathing, hypercapnia and the release of adrenaline into the blood. In this case, the concern is:
- increasing anxiety and feeling of fear;
- convulsive and rapid breathing;
- feeling of suffocation;
- increasing shortness of breath and feeling of lack of air with every breath, cough;
- dizziness and weakness due to frequent inhalations and exhalations;
- sweating of the palms of the hands, face, back;
- inability to concentrate;
- increased heart rate and pulse;
- severe fatigue after an attack.
Cardialgia and shortness of breath appear against the background of increased blood pressure. Complaints of nausea or vomiting, heart pain and lack of air indicate a hypertensive crisis. Pain and a feeling of lack of oxygen intensify due to a sharp spasm of blood vessels, impaired cerebral circulation, and deterioration of general hemodynamics. The most dangerous is a sharp increase in blood pressure for pregnant women, since the risk of placental abruption, cerebral hemorrhage, and stroke increases significantly.
Causes of pain when inhaling
Normally, at the moment of inhalation, the volume of the thoracic cavity increases due to relaxation of the diaphragm and contraction of the intercostal muscles, which lift the ribs upward. This reduces the pressure in the lungs and fills them with air.
Therefore, often the appearance of pain in the heart area when inhaling may in no way be associated with cardiac problems and requires a thorough diagnosis of the bone frame of the chest and the respiratory system.
Cardiac causes of pain in the heart area when inhaling also cannot be excluded, since they are extremely common among the population.
According to statistics, about 57% of the total number of deaths is associated with diseases of the cardiovascular system, and the total number of deaths due to heart problems reaches 17.5 million cases annually.
You cannot ignore pain in the heart area, no matter what it is. Especially if the last preventative visit to your family doctor or general practitioner was a very long time ago, and also if there are other cardiovascular risk factors.
Important! Conditions that increase the risk of developing myocardial infarction and other cardiovascular diseases include:
- Arterial hypertension.
- Overweight and obesity.
- High levels of lipids and triglycerides in the blood.
- Physical inactivity is a lack of physical activity.
- Smoking and alcohol abuse.
- Diabetes.
- Chronic stress and lack of sleep.
- The presence of myocardial infarction at a young age in close blood relatives.
In clinical practice, the SCORE scale is also used to calculate the risk of cardiovascular pathologies. To quickly calculate your risk of heart disease in 10 years, use the calculator.
How to determine the source of discomfort
To determine the diagnosis, evaluate:
- pain intensity;
- localization, irradiation;
- duration of the attack;
- time of occurrence, frequency;
- provoking factors (changes in posture, movements, physical work);
- which eases the pain.
Additional symptoms indicating non-cardiac causes of pain:
- elevated temperature;
- cough, hemoptysis;
- progressive shortness of breath;
- digestive disorders;
- profuse sweating;
- emotional instability;
- focal neurological symptoms.
Differences between cardialgia caused by heart disease and neurocirculatory dystonia:
| Sign | Angina pectoris | NDC |
| Age | From 30 years (for men), from 50 (for women) | Often from 12 to 30 years |
| Risk factors for coronary heart disease | Present | No |
| Nature of pain | Mainly pressing, squeezing | Sharp, stabbing, cutting, pulsating, dull |
| Localization | Deep in the chest | In the area of the heart, left half of the chest |
| Irradiation | In the arms, lower jaw, back, shoulder blade on the left | No |
| What causes pain | Physical activity, increased blood pressure or heart rate | Physical, emotional stress, body turns, deep breathing, fatigue, anxiety, depression |
| Connection with loads | Occurs at peak voltage | Not associated with stress, physical work distracts or relieves pain |
| Duration | From 2 to 20 minutes | From a few seconds to days |
| What relieves the symptom | "Nitroglycerine" | "Valerian", "Validol" |
| ECG changes | Transient ST segment depression and/or negative T wave | Not typical |
Source clarification algorithm:
| Provoked by physical activity | Angina pectoris, myocardial infarction |
| Accompanies meals with additional symptoms of damage to the digestive system | Diaphragmatic hernia, biliary colic, cardiospasm, diverticulum, dyskinesia of the gallbladder |
| Intensifies with deep inspiration and independent movements of the upper body | Pericarditis, pulmonary pathology, pleurisy |
| Increases with palpation of the chest | Intercostal neuralgia, trauma, spinal osteochondrosis |
| Other options | Aortic arch aneurysm, neurocirculatory dystonia, myocarditis, valve defects, cardiomyopathy |
In addition to examining and finding out the history of the disease, to determine the final diagnosis, the doctor prescribes:
- To confirm/exclude ischemic heart disease and angina:
- ECG;
- echocardiography;
- load tests;
- coronary angiography.
- X-ray of the chest organs;
- MRI of the spine;
- echocardiography;
- Ultrasound of the abdominal organs;
- FEGDS;
- study of gastric juice acidity;
- detailed blood test;
- rheumatic tests;
- Ultrasound of the thyroid gland, thyroid hormones;
- consultation with a neurologist.
When inhaling, pain in the heart area is associated with diseases of the spine, their features:
- exacerbations and remissions of cardialgia are identical to the course of osteochondrosis;
- symptom reduction from nonsteroidal anti-inflammatory drugs, muscle relaxants, and physical therapy;
- the occurrence of pain after stress on the back;
- lack of effect from nitrates;
- increased symptoms when coughing, deep breathing, turning the body.
Causes of pain depending on sensations
Diseases are rarely accompanied by only one symptom.
More often, other signs and sensations also occur (Table 1), potentially indicating damage to a particular organ. Table 1. Symptoms accompanying the most common causes of chest pain when inhaling
| Feel | Disease |
| A feeling of acute, burning pain in the heart area, which lasts from 5 to 15 minutes and is relieved by taking nitroglycerin under the tongue. May be accompanied by fear of death. | Angina pectoris |
| Symptoms are similar to angina pectoris. But, unlike the previous condition, pain in the heart area persists for more than 15 minutes, and taking nitroglycerin has no effect on it. | Myocardial infarction |
| Mild pain is accompanied by a feeling of strong, rapid heartbeat. The pulse may be more than 100 beats/min and may not correspond to the heart rate. Dizziness, general weakness, and lightheadedness also occur. | Arrhythmias |
| Sharp or dull pain that occurs immediately after an injury or a short time after it. Intensifies with movement and deep breathing. At rest, it may weaken or disappear altogether. | Damage to intercostal muscles, ribs |
| Discomfort or pain that begins to “prick” in the chest during a stressful situation or during emotional shock. Associated phenomena - increased heart rate, increased sweating, feelings of fear or anxiety | Anxiety or panic attack |
| Increased pain with deep breathing, cough with mucous or purulent sputum, increased body temperature to 38-39℃ | Pneumonia and other infectious diseases of the respiratory system |
| Chest pain that gets worse when you inhale. Inhalation is very difficult. The condition is often triggered by inhaling dust, pollen, or missing a dose of medication used to prevent attacks. | Attack of bronchial asthma |
| The appearance of pain is preceded by tingling and itching. Soon after the pain appears on the skin along the costal arch, rashes appear in the form of spots, and then blisters, which open and leave behind crusts | Herpes zoster |
| Stitching pain behind the sternum, worse when inhaling. Accompanied by shortness of breath, cough, drop in blood pressure, increased heart rate, fear | Pulmonary embolism |
Common reasons
Any pain in the pericardial region is called cardialgia and is associated with problems:
- of cardio-vascular system;
- lungs and pleura;
- mediastinum;
- esophagus;
- chest wall;
- spine;
- nervous system;
- diaphragms;
- digestive organs;
- for viral infections.
Such a variety of causes significantly complicates differential diagnosis and establishment of the root cause of pain.
Heart diseases
The main causes of heart pain associated with cardiovascular pathology:
- Ischemic (myocardial malnutrition): Coronary heart disease (CHD): Acute coronary syndrome (with/without ST segment elevation). The main difference from angina pectoris is progressive shortness of breath, rapid heartbeat, a sharp deterioration in general condition, lack of effect from Nitroglycerin and a continuing attack at rest for more than 20 minutes.
- Angina pectoris is attacks of pain in the heart after emotional or physical stress of varying nature and intensity. Cardialgia goes away after taking Nitroglycerin tablets and being completely at rest.
- Valvular heart defects (often aortic stenosis) - attacks of pain are identical to those with ischemic heart disease (coronary vessels extend below the narrowing).
- Hypertrophic cardiomyopathy is a disease of unknown etiology in which the myocardial mass progressively increases, blocking the exit of blood from the left ventricle.
- Pericarditis is an inflammation of the sac surrounding the heart (with or without fluid accumulation in it). The pain is long-lasting, constant, and intensifies in a horizontal position on the back, taking a deep breath.
- Myocarditis is an inflammatory disease of the heart muscle that occurs as a result of a viral or bacterial infection, which manifests itself as prolonged aching pain in the heart area without a specific localization and is accompanied by arrhythmias.
- Pulmonary embolism is a rapidly occurring blockage of the lumen of a vessel by a thrombus. The main symptoms of BODY are chest pain and shortness of breath. They appear suddenly and grow progressively. Additionally, a drop in blood pressure, cyanosis, cough, and impaired consciousness are observed. The severity of symptoms depends on the size of the clot and the level of occlusion. Often, patients with TELA are diagnosed with diseases of the veins of the lower extremities.
- Dissecting aortic aneurysm is a life-threatening condition that develops in patients with severe hypertension and atherosclerosis. Pain sensations are identical to those in acute coronary syndrome.
- Alcoholic cardiomyopathy.
Extracardiac pathologies
Conditions that cause heart pain when taking a deep breath:
- Lung diseases:
- Pneumonia is an inflammatory disease caused by a virus or bacteria. Accompanied by intoxication, cough, pain when breathing deeply.
- Lung cancer - pain when breathing with shortness of breath, cough, weakness, low-grade fever, weight loss.
- Pleurisy is an inflammation of the layers that envelop the lungs. It manifests itself as sharp, dagger-like stabbing pains in the chest when breathing, coughing, and high fever. Lying on the sore side helps relieve the condition.
- Spontaneous pneumothorax is the collapse of the lungs due to damage and their exclusion from the breathing process. Develops in patients with long-term COPD, emphysema, cancer, tuberculosis.
- Mesothelioma is a tumor lesion of the layers of the pleura, which have many painful endings, causing pain from friction when breathing.
- cancer;
- diffuse spasm of the esophagus;
- diverticula;
- diaphragmatic hernia.
- biliary colic;
- chronic cholecystitis;
- biliary dyskinesia.
- Neurocirculatory dystonia is a disorder of the autonomic innervation of the cardiovascular system, occurring mainly in children and adolescents. In addition to chest pain provoked by stress and hormonal surges, such patients experience increased rhythm, emotional lability, headaches, nervousness, and low tolerance to physical activity.
- Panic attack.
- Psychogenic cardialgia.
- Depression.
- Hyperventilation.
- Spondylosis is a spiky growth of the edges of the vertebral body, which in a certain position puts pressure on the spinal roots and causes pain.
- Intercostal neuralgia is a disease caused by irritation or compression of the nerve of the same name. The disease is manifested by attacks of stabbing pain in the chest during deep breathing, limiting the ventilation of the lung tissue. An attack is provoked by sudden movements, coughing, sneezing, and uncomfortable posture.
- Left rib injury.
- Hyperthyroidism.
- Herpes zoster is a viral infection of the endings of the intercostal nerve, which is accompanied by intense stabbing sensations (heart pain when inhaling), aggravated by movement, touching and deep breathing.
Feelings associated with heart disease
More often than others, pain that occurs in the heart area when inhaling is provoked by the following diseases of the cardiovascular system:
- Angina pectoris.
- Myocardial infarction.
- Pulmonary embolism.
Cardiological causes of heart pain are extremely varied and quite often nonspecific. However, there are a number of features that indicate a connection with heart disease.
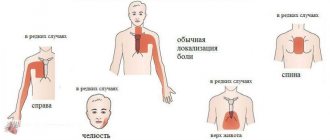
For example, with myocardial infarction (Fig. 2) and angina pectoris, pain often radiates (“gives”) to the area of the left shoulder and shoulder blade, neck and lower jaw. As a rule, it is associated with exposure to triggers - physical activity, smoking, errors in taking necessary medications. In this case, there is often no connection with respiratory movements.
Also, with a heart attack, severe weakness, shortness of breath, a characteristic “fear of death” occurs, and cold, sticky sweat appears on the forehead. Other possible signs of this pathology are: heart rhythm disturbances, dizziness, nausea.
Figure 2. Symptoms of myocardial infarction. Source: MedPortal
In general, cardiac pain is often accompanied by fluctuations in blood pressure, both towards hypertension (above 140/90 mmHg) and hypotension (below 90/60 mmHg). Also, a clear marker of pain of cardiac origin is a violation of the rhythm of heart contractions and “pulse deficiency” - a phenomenon in which the heart rate does not correspond to the pulse rate in the peripheral arteries.
Cardiac problems are often combined with heart failure, which is accompanied by symmetrical swelling of the extremities and acrocyanosis - bluishness of the skin in areas of the body distant from the heart: fingers and toes, lips, ears, etc.
It is important to understand that cardiac diseases can “masquerade” as other pathologies, which makes them quite difficult to recognize. For example, with myocardial infarction with a focus of ischemia in the region of the posterior-inferior part of the heart, pain may occur in the center of the upper abdomen.
Difficulties in diagnosis are added by concomitant diseases, for example, uncontrolled diabetes mellitus, in which pain in the heart, even with the same myocardial infarction, may be absent due to diabetic polyneuropathy (a complication of diabetes mellitus in which damage to peripheral nerves occurs and can be accompanied by both pain and loss sensitivity).
What conditions can cause pain?
The chest area contains internal organs such as the lungs, trachea, pleura, heart, esophagus and diaphragm. The disease of any of them can cause pain in a person. The most common conditions that cause pain when breathing are:
- heart pathologies;
- injuries accompanied by rib fractures;
- disease of the pectoral cartilage - costochondritis;
- damage to intercostal muscle fibers;
- inflammatory process of the pleura;
- pneumothorax;
- osteochondrosis;
- intercostal neuralgia;
- shingles;
- bronchitis or pneumonia.
Each disease has its own symptoms, one of which may be pain in the heart when inhaling.
Sensations not associated with heart pathologies
The most common causes of pain in the heart area when inhaling, not associated with cardiac diseases, are:
- Pneumonia is inflammation of the lungs.
- Pleurisy is inflammation of the pleura, which can also lead to the accumulation of fluid in the chest cavity (hydrothorax).
- Damage to the ribs.
- Injuries of intercostal nerves.
- Gastroesophageal reflux disease and other lesions of the esophagus or upper stomach.
- Psychosomatic reactions.
Pathologies of the lungs and respiratory tract (Fig. 3) are accompanied by pain spreading over the entire surface of the chest, intensifying with inhalation and/or exhalation. The cough that occurs in this case is often wet and leads to expectoration of mucous or purulent sputum. An increase in body temperature to 39℃ is also typical.
Figure 3. Causes of pleural chest pain. Source: MedPortal
Rib lesions are always associated with previous chest injuries. The pain is directly related to the respiratory act and its depth. There may be swelling and bleeding on the skin at the site of the rib injury.
Pathologies of the nervous system, in particular the intercostal nerves and spinal roots, are always associated with chest movements and physical activity. In this case, pain often has a “girdling character” and is limited to 1-3 intercostal spaces. With infectious lesions of the nerve trunks, an increase in body temperature is observed, and a rash appears on the skin.
Chest pain caused by diseases of the gastrointestinal tract is directly related to food intake. They are often accompanied by “sour” or “rotten” belching, diarrhea or constipation.
With a psychogenic origin of chest pain, the provoking factor is always stress or emotional stress, and any objective changes, as a rule, are absent. At the same time, stabilizing the emotional state, including with the help of sedatives, brings relief.
Non-cardiac pathologies
In addition to diseases of the heart and blood vessels, pain in the chest when inhaling can occur due to other pathological conditions. These are problems with the respiratory system, esophagus, thoracic spine and some other diseases. Let's take a closer look at them.
Osteochondrosis
Osteochondrosis is a disease that occurs mainly in patients after 35–40 years of age, accompanied by displacement and dissection of intervertebral discs, pinching of nerve fibers in this area. The risk group for the disease includes people who lead a sedentary lifestyle or, conversely, regularly perform heavy physical work, as well as patients whose medical history is burdened by a genetic predisposition to the disease. In addition, osteochondrosis is caused by injuries, infectious diseases and some other reasons.
Signs of pathology:
- pain in the sternum when inhaling, very similar to heart pain;
- feeling of stiffness;
- neuralgic disorders - numbness of the limbs, spots before the eyes, blurred vision and hearing, tinnitus.
Important! Pain when inhaling in the region of the heart is most often caused by osteochondrosis of the thoracic spine.
Osteochondrosis of the thoracic spine is a common cause of pain in the sternum
Rib fracture
In the area of the sternum there are paired ribs. Injuries in this area can cause a rib fracture, which is characterized by the following symptoms in the patient:
- acute stabbing pain in the heart area when inhaling (fracture on the left side);
- the patient takes a forced position of the body;
- shallow breathing with intermittent breaths;
- chest deformation;
- a characteristic crunch due to bone friction (with multiple fractures).
The most dangerous is considered to be a fracture that damages internal organs (heart, lungs, aorta). The condition requires immediate medical intervention, as in some situations a person can lose his life in a matter of minutes.
Costochondritis
A pathological condition caused by inflammation of the cartilage connecting the ribs and sternum is costochondritis. Another name for the disease is costosternal syndrome. The disease develops due to damage to the cartilage by infection, as well as as a result of strong physical effort or injury. Clinical manifestations include:
- pain in the left side of the sternum, which intensifies when inhaling or coughing;
- shortness of breath;
- incomplete inspiration;
- general deterioration of health;
- weakness, apathy.
Treatment is carried out with the help of non-steroidal anti-inflammatory drugs, analgesics, and physical therapy.
Rupture or strain of intercostal muscles
A sprain or complete tear of the intercostal muscle occurs due to injuries in this area. When the fibers break, a person hears a characteristic click and feels a sharp pain. Stretching is accompanied by less obvious signs. The patient may experience discomfort and pain when inhaling air. If muscle damage occurs on the left, many patients confuse these sensations with pain in the heart. The clinical picture is complemented by the following signs:
- muscle deformation;
- formation of edema and hematoma;
- an increase in local temperature.
Rupture of muscle fibers causes severe pain
If the pain is moderate, indicating a minor sprain, apply a cold compress to the injured area for 10–15 minutes. If a muscle ruptures, you must go to the hospital.
Important! It can be quite difficult to independently understand the extent of muscle damage, so it is better to consult a specialist.
Inflammation of the pleura
The thin serous membrane that lines the space between the lungs and the chest is called the pleura. When this area is damaged by viral, bacterial, parasitic infections or fungal microorganisms, an inflammatory process of the pleura develops. In addition, the disease can be caused by reasons not related to the spread of infection. These include myocardial infarction, vascular diseases, tumors, sternum injuries and more.
Symptoms of the disease:
- pain when inhaling;
- dry cough;
- increased body temperature;
- weakness;
- swelling of the face and neck.
Treatment of the disease depends on the primary disease that provoked pleurisy. Medicines include corticosteroids, antibacterial drugs, non-steroidal anti-inflammatory drugs, and diuretics. During treatment, the patient needs a correct daily routine and nutrition.
Intercostal neuralgia
Stitching, aching, pressing pain, which is periodic or constant, often indicates the development of compression or irritation of the nerve fibers located in the ribs. Neuralgia occurs, as a rule, with osteochondrosis, ankylosing spondylitis, intervertebral hernias, sternum injuries and other conditions.
Intercostal neuralgia has a very similar course to many other diseases
The patient's clinical picture is accompanied by pain in the sternum during inhalation, turning, and physical activity. Discomfort during palpation increases. Often the symptoms of intercostal neuralgia are confused with heart pathologies, pleurisy, hepatic colic, tumors and other conditions.
Pneumothorax
Pneumothorax is the process of excessive accumulation of air between the pleural sheets, which entails dysfunction of the respiratory and cardiovascular systems. Pathology occurs due to mechanical damage to the pleura or against the background of diseases of organs located in the chest area. Mechanical pneumothorax often occurs due to severe coughing, sternum trauma, and physical exertion.
Characteristic signs of the disease:
- acute pain at the beginning of the attack;
- discomfort when inhaling;
- forced position of the patient's body;
- shortness of breath, difficulty breathing.
Medical assistance for this condition should be immediate. Treatment is carried out in a hospital setting by evacuating excess air surgically.
Bronchitis
Disease of the bronchi of a diffuse inflammatory nature, provoked by various factors, is called bronchitis. There is a chronic or acute form of the disease. Among the signs accompanying this condition are:
- severe cough, nasal congestion;
- pain when inhaling and exhaling, very often reminiscent of pain in the heart;
- increased body temperature;
- sputum separation;
- weakness;
- increased sweating.
Pain when inhaling into the heart often occurs with bronchitis
There are acute and chronic forms of bronchitis. The causes of the pathology lie in infectious and toxic damage to the bronchi. Most often, the disease occurs against the background of influenza, acute respiratory infections and ARVI, as well as among patients whose work activity is associated with regular damage to the bronchi by harmful chemicals.
Pneumonia
Pneumonia or pneumonia is a lesion of the lung tissue that occurs more often when the respiratory organs are damaged by a viral, bacterial or fungal infection. Most often, pneumonia occurs due to the influence of streptococci, staphylococci, chlamydia and other pathogens.
Characteristic manifestations:
- pain when trying to breathe air;
- severe dry cough;
- sweating;
- dyspnea;
- increase in body temperature to 39–40 degrees;
- weakness, loss of appetite;
- less likely to faint.
Treatment of the disease is carried out in a hospital setting under the close supervision of medical personnel. Lack of timely treatment often ends in death.
When should you see a doctor?
Pain in the heart area is a dangerous symptom that always requires additional diagnostics and a search for its causes. It is important to understand that diseases of all organs and systems require appropriate attention and treatment. But in some cases, you can independently determine the danger of a developing condition.
For the first time in life, an acute attack of pain in the heart area always requires contacting emergency medical services. The same applies to people with previously diagnosed angina pectoris (a form of angina in which pain occurs only against the background of a trigger and is eliminated by taking nitroglycerin) if taking a previously effective dose of nitrates did not relieve the pain within 15 minutes of taking the drug.
The absence of a serious danger may be indicated by pain or discomfort behind the sternum, which occurs immediately after a sharp turn or tilt of the body, eating or taking a horizontal position after eating. This also includes short-term attacks of mild pain that occur against the background of strong experiences or stressful situations. In such cases, a scheduled visit to the doctor is recommended.
Important! Regardless of the characteristics of the pain, the presence or absence of radiation, other symptoms or provoking factors, diagnosis is necessary. Only a doctor's examination, laboratory tests, ECG and other studies can help accurately determine the origin of pain and exclude life-threatening conditions.
Causes of pain
The feeling of pain in the left side of the chest has a different character. A person may experience sharp and aching pain, periodic and constant, pressing and stabbing. Among the reasons for their appearance are:
- precordial syndrome;
- pinched or irritated intercostal nerves;
- presence of air in the chest;
- dry pleurisy or pericarditis;
- bruises and chest injuries;
- heart pathologies;
- neurotic conditions.
The severity of the condition and its treatment depend on the type of problem. Consultations with a cardiologist, pulmonologist or neurologist may be necessary. We will talk about the features of each pathology further.
Heart diseases
The first thing that is suspected when pain in the chest area appears is heart disease. They can be distinguished from non-cardiac diseases by the following characteristics:
- pain occurs periodically, the duration of each attack is 10-15 minutes;
- More often, heart pathologies cause burning and pressing pain;
- attacks are triggered by stress and physical activity;
- stabbing pain can radiate to the arm, shoulder blade or neck on the left side.
Chest discomfort during breathing occurs due to cardiac pathologies:
- Pericarditis
- inflammation of the outer lining of the heart muscle, develops for various reasons. It is characterized by the accumulation of fluid in the pericardial cavity and disturbances in the functioning of the cardiac system. The pain is dull and pressing, worsens with swallowing, coughing and deep breathing. Additional symptoms include: a feeling of lack of air, loss of strength, poor appetite, increased body temperature, sweating. - Angina pectoris
- a common symptom of dysfunction of the cardiovascular system. Manifests itself in a feeling of discomfort, compression behind the sternum. The attacks appear intermittently and last from 10 to 15 minutes. - Heart attack
- a condition requiring immediate medical attention. The patient feels that something is pressing inside, the pain is transmitted to the left arm, neck, and shoulder blade. Nausea and heartburn, chills, and possible fainting also appear.
If a set of symptoms of heart disease appears, you must immediately seek help; delay can be life-threatening.
Causes of traumatic nature
Any injuries to the chest and ribs can cause sharp stabbing pain. A bruise and fracture of the bones of the chest are characterized by the appearance of a pain symptom not only when inhaling and exhaling, but also when changing the position of the body. Sometimes mechanical impact on the sternum causes traumatic pneumothorax.
Stitching in the heart area, what to do if it is pneumothorax? The diagnosis is characterized by the accumulation of air in the outer lining of the lung. It may be intact or a similar phenomenon is caused by a violation of the structure of the lung tissue, then they speak of spontaneous pneumothorax. Symptoms of the condition include:
- stabbing, sharp pain, radiating to the arm and neck on the left;
- discomfort increases with physical activity, coughing, laughing, taking a deep breath or diving under water;
- at rest, the pain subsides after a few hours;
- Additional signs include: pale complexion, shortness of breath, panic attacks, and sometimes a dry cough.
The risk group for spontaneous pneumothorax includes adult men under 40 years of age. Sudden changes in pressure, such as flying at high altitude, can cause disruption of the integrity of internal tissue. Only specialists treat the disease.
Pneumothorax can be a consequence of other diseases - tuberculosis, pneumonia, lung tumors.
Dry pleurisy - pathologies of the respiratory system
Often the cause of chest pain is pathology of the respiratory system. The pleura covers the lungs and chest cavity; any inflammatory lesions of this membrane are called pleurisy.
Features of dry pleurisy include:
- the left or right half of the chest constantly hurts;
- symptoms intensify with deep inspiration and coughing; immobilization of the affected side alleviates the condition;
- symptoms of general malaise are noted: temperature ranges from 36.6 to 39? C, chills and fever appear, appetite decreases, the patient feels weak;
- inflammation takes a long time, from 1 to 3 weeks, without proper treatment it develops into a chronic form.
The nature of pleurisy may lie in diseases of the lungs or nearby organs. In the first case, it is tuberculosis, pneumonia or pulmonary abscess. In the second - subphrenic abscess, infectious diseases of the abdominal cavity, pancreatitis and rheumatism.
Intercostal neuralgia
Intercostal neuralgia is of two types. In the first case, inflammation or pinching of the spinal nerve root occurs, in the second - the nerves in the intercostal space. The main symptom of neuralgia is pain localized in the chest; it can radiate to the lower back, neck or under the shoulder blade.
The pain is strong and burning. It gets worse with deep breathing, physical activity, sneezing, coughing, or sudden movements of the body if there is pressure on the nerve. Other signs of the disease include:
- involuntary muscle contraction;
- changes in skin color and sensitivity in the area of nerve damage;
- the pain may be accompanied by numbness in an area of the body, or the patient feels that this area is burning, stabbing, like needles.
Neuralgia is often confused with cardiac pathologies; it differs in the nature of the pain and its intensification when inhaling and exhaling.
Among the reasons for pinching or inflammation of the nerve root are:
- osteochondrosis;
- Bekhterev's disease;
- spondylitis;
- chest injuries;
- prolonged stress;
- excessive physical activity;
- infectious diseases;
- severe hypothermia;
- changes in hormonal levels;
- spinal injuries or diseases;
- allergic reactions;
- tone of one or more back muscles.
After the examination, the doctor will give recommendations on how to relieve pain, and then determine the nature of the pinched nerve. The diagnosis is not life-threatening, but you can get rid of it only after eliminating the cause.
Neuroses and precordial syndrome
Neurotic conditions can cause sensations of stabbing pain in the heart area. Usually in such cases, patients think about a serious illness; all their sensations are psychosomatic in nature. The patient may also complain of:
- feeling of a lump in the throat;
- that it is difficult to breathe;
- cardiopalmus;
- nausea;
- stomach ache.
Sensitive people and those who are under constant stress are susceptible to such conditions. Another selective symptom is precordial. The causes of the condition are still not fully understood, but it has its own characteristic features:
- sudden sharp pain in the chest area;
- the duration of the attack is from 0.5 - 3 minutes;
- pain occurs even at rest;
- breathing deeply is difficult;
- The frequency of attacks is always different, sometimes there are several attacks per day.
According to doctors, this syndrome occurs in people under 20 years of age and goes away with age.
What to do before the ambulance arrives?
If myocardial infarction or pulmonary embolism develops, proper treatment can only be carried out in a hospital setting.
Even before the ambulance arrives, you should:
- Take one tablet of aspirin, nitroglycerin. Aspirin reduces blood clotting, nitroglycerin improves blood supply to the myocardium.
- Make breathing as easy as possible. It is important to provide fresh air. To do this, you need to open a window in the room and remove clothes that are constricting your chest, for example, unbutton the buttons of a shirt.
- Take a comfortable position. A semi-sitting pose can make breathing easier, which you can take by placing several pillows under your head and shoulders. Another option is a sitting position with your elbows resting on your knees or a table with your torso slightly tilted forward. (Fig. 4).
- Try to calm down and not panic. During stress, the heart rate, respiratory movements and the heart's need for oxygen increase. All this aggravates the course of myocardial infarction and pulmonary embolism and worsens the prognosis.
Figure 4. Poses that make breathing easier. Source: MedPortal
Treatment
Since chest pain during inspiration can be caused by pathologies of different organs and systems, their treatment tactics will vary significantly.
Myocardial infarction and pulmonary embolism can be treated with thrombolysis - intravenous administration of drugs that can “dissolve” blood clots. However, such procedures are effective in the first 4-6 hours from the moment pain appears. At a later date, other treatment methods are used.
Other cardiac causes may require normalization of blood pressure, heart rate with the help of appropriate medications, restoration of heart valve function by replacing them, etc.
Infectious lesions of the lungs, accompanied by pain in the heart area, may require the use of antibacterial or antiviral agents. For bronchial asthma, the treatment regimen includes β2-agonists, glucocorticosteroids, etc.
Gastrointestinal pathologies can be brought under control by normalizing nutrition and physical activity; doctors advise fighting obesity and taking medications that affect the pH level of the stomach cavity.
Intercostal neuralgia is treated with analgesics, non-steroidal anti-inflammatory drugs, B vitamins and muscle relaxants.
In case of psychogenic cardialgia, it is recommended to consult a medical psychologist or psychiatrist to decide on the need to use sedatives.
Prevention
Prevention of pain in the heart area when inhaling is complex and is aimed at strengthening the entire body as a whole and the cardiovascular system in particular. First of all, this is a healthy lifestyle: a rational schedule of work and rest, proper nutrition and moderate physical activity. Cardio training and yoga help control breathing and strengthen the heart muscle.
However, if you have concomitant diseases, it is important to coordinate all your actions with your doctor. For example, the doctor will help you control the level of fat and cholesterol you consume. This is important because they are part of cell membranes, and completely avoiding their consumption can be harmful.
What to do and how to stop an attack
With shortness of breath or dyspnea, breathing is disrupted, becomes more frequent, with difficulty inhaling or exhaling, and a lack of air is often felt. There are many reasons that affect both the respiratory system and the functioning of the cardiovascular system. Do not worry if shortness of breath appears after increased exercise, physical fatigue, stress or emotional distress - this is a normal manifestation of the physiological reaction of the body of a healthy person to the body’s increased need for oxygen.
A more alarming symptom is a pain attack, cardialgia. Measures for heart pain and heavy breathing:
- Take a comfortable position, sit down and lie down.
- Don’t panic, try not to think about the bad.
- Restore your breathing by taking calm, measured inhalations and exhalations.
- If the room is stuffy, open the window and free your neck from tight clothing.
- For patients with hypertension, measure blood pressure. When the numbers increase above normal, they take antihypertensive drugs.
- If squeezing or stabbing pain in the heart bothers you for more than 10-15 minutes, call an ambulance.
- It is not recommended to take medications on your own before the ambulance arrives.
- Pregnant women who experience severe pain in the heart and difficulty breathing should immediately contact an obstetrician-gynecologist.
- Elderly patients with persistent deterioration of their condition, severe cardialgia and a feeling of lack of air should take a Nitroglycerin tablet under the tongue and call an ambulance.
- When episodes of heart pain and shortness of breath quickly pass with rest, but are repeated more and more often, go to the doctor for a routine examination.
Sources
- Trukhan D.I., Davydov E.L. “Chest pain: current issues in clinical diagnosis and treatment of angina” // Consilium Medicum – No. 17(10) – 2015.
- Yu. V. Vasiliev “Pain behind the sternum: differential diagnosis, treatment” // Cardiology - 2006.
- Ruigomez A., Rodriguez LA, Wallander MA et al “Chest pain in general practice: incidence, comorbidity and mortality” // Fam. Pract. – Vol. 23 – 2006
- A.N. Belovol, I.I. Knyazkova “Clinical approaches to the diagnosis of chest pain” // Current preparations and technologies – No2 (78) – 2011 r.
- Nilsson S., Scheike M., Engblom D. et al. “Chest pain and ischemic heart disease in primary care” // Br. J.Gen. Pract. – Vol. 53 – 2003.