Capoten is one of the most commonly prescribed drugs for high blood pressure. However, despite its widespread popularity, few people know about its features.
Therefore, when patients are prescribed these pills, they simply have a huge number of questions.
If doctors do not bother themselves with detailed answers, then their patients have to check in practice how long it takes for Capoten to start working or how effective it is as an “ambulance” in a hypertensive crisis. Let's correct this situation - answer these and other questions.
Kapoten: what is it for?
Capoten (captopril) is an ACE inhibitor. It was discovered back in the 1970s of the 20th century. A study of kidney function in the development of hypertension identified angiotensin-converting enzyme, which the kidneys produce to increase blood pressure.
The hypotensive effect of Capoten is explained by the suspension of the production of angiotensin II, which thereby minimizes its vasoconstrictive effect and also eliminates water retention in the body.
Capoten tablets
In addition, the drug reduces the synthesis of aldosterone, a hormone whose final result is an increase in systemic blood pressure. In addition, the effect of the drug also has a positive effect on the heart: preload weakens, systolic pressure in the right ventricle drops, and cardiac output increases.
With regular use, tolerance to physical and other stress increases and well-being improves. The main indication for use is problems with high blood pressure.
Capoten is recommended for use in the following diseases:
- arterial hypertension (both with moderate and significant increases). Prescribed as monotherapy or combined with various medications;
- congestive heart failure. In case of ineffective use of cardiac glycosides;
- heart attack;
- diabetic nephropathy;
- kidney pathology causing hypertension.
A full examination before starting to take the drug and, if necessary, careful medical monitoring during treatment will minimize the risks associated with its use.
In fact, these tablets can be included in the treatment plan by the attending physician in other cases if there is a concomitant appearance of hypertension against the background of the underlying disease.
CAPOTEN
special instructions
Before starting, as well as regularly during treatment with Capoten®, renal function should be monitored.
In patients with chronic heart failure, it is used under close medical supervision. When taking ACE inhibitors, a characteristic non-productive cough is observed, which stops after discontinuation of therapy with ACE inhibitors. In rare cases, when taking ACE inhibitors, a syndrome is observed that begins with the appearance of cholestatic jaundice, turning into fulminant hepatonecrosis, sometimes with a fatal outcome. The mechanism of development of this syndrome is unknown. If a patient receiving therapy with ACE inhibitors develops jaundice or there is a marked increase in the activity of liver enzymes, treatment with ACE inhibitors should be discontinued and the patient should be monitored. Some patients with kidney disease, especially those with severe renal artery stenosis, experience increases in serum urea nitrogen and creatinine concentrations after lowering blood pressure. This increase is usually reversible upon discontinuation of therapy with Capoten®. In these cases, it may be necessary to reduce the dose of Capoten® and/or discontinue the diuretic.
During long-term use of the drug Capoten®, approximately 20% of patients experience an increase in serum urea and creatinine concentrations by more than 20% compared to the norm or baseline value.
In less than 5% of patients, especially with severe nephropathy, treatment discontinuation is required due to an increase in creatinine concentration.
The use of dual blockade of the renin-angiotensin-aldosterone system (RAAS) caused by the simultaneous use of ACE inhibitors and angiotensin II receptor antagonists or aliskiren and aliskiren-containing drugs is not recommended, since it has been associated with an increased incidence of side effects such as arterial hypotension, hyperkalemia, decreased renal function (including acute renal failure). If the simultaneous use of ACE inhibitors and ARA II (dual blockade of the RAAS) is necessary, then treatment should be carried out under the supervision of a physician and with constant monitoring of renal function, electrolyte levels in the blood, and blood pressure.
The combined use of ACE inhibitors and angiotensin II receptor antagonists in patients with diabetic nephropathy is not recommended.
In patients with arterial hypertension, when using the drug Capoten®, severe arterial hypotension is observed only in rare cases; the likelihood of developing this condition increases with increased loss of fluid and salts (for example, after intensive treatment with diuretics), in patients with heart failure or on dialysis. The possibility of a sharp decrease in blood pressure can be minimized by first withdrawing (4-7 days before) the diuretic or increasing the intake of sodium chloride (about a week before starting treatment), or by prescribing the drug Capoten® at the beginning of treatment in small doses (6, 25-12.5 mg/day).
Prescribe with caution to patients on a low-salt or salt-free diet (increased risk of developing arterial hypotension) and hyperkalemia. An excessive decrease in blood pressure may occur in patients during major surgical operations, as well as when using general anesthesia agents that have a hypotensive effect. In such cases, to correct low blood pressure, measures are taken to increase the volume of circulating blood.
Excessive reduction in blood pressure due to antihypertensive medications may increase the risk of myocardial infarction or stroke in patients with coronary heart disease or cerebrovascular disease. If arterial hypotension develops, the patient should take a horizontal position with legs elevated. Intravenous administration of 0.9% sodium chloride solution may be required.
Caution should be exercised when taking ACE inhibitors in patients with mitral/aortic stenosis/hypertrophic obstructive cardiomyopathy; in case of cardiogenic shock and hemodynamically significant obstruction, use is not recommended.
Neutropenia/agranulocytosis, thrombocytopenia and anemia have been reported in patients taking ACE inhibitors. In patients with normal renal function and in the absence of other disorders, neutropenia is rare. In case of renal failure, simultaneous use of the drug Capoten® and allopurinol led to neutropenia.
The drug Capoten® should be used very carefully in patients with autoimmune connective tissue diseases, in those taking immunosuppressants, allopurinol and procainamide, especially in the presence of pre-existing renal dysfunction. Due to the fact that the majority of fatal cases of neutropenia due to ACE inhibitors developed in such patients, their blood leukocyte count should be monitored before starting treatment, in the first 3 months - every 2 weeks, then every 2 months.
In all patients, the number of leukocytes in the blood should be monitored monthly in the first 3 months after starting therapy with Capoten®, then every 2 months. If the number of leukocytes is below 4000/μl, a repeat general blood test is indicated; below 1000/μl, the drug is stopped while monitoring the patient continues. Typically, restoration of the number of neutrophils occurs within 2 weeks after discontinuation of the drug Capoten®. In 13% of cases of neutropenia, death was noted. In almost all cases, death was observed in patients with connective tissue diseases, renal or heart failure, while taking immunosuppressants, or a combination of both of these factors.
When using ACE inhibitors, proteinuria may occur, mainly in patients with impaired renal function, as well as when using high doses of drugs. In most cases, proteinuria when taking the drug Capoten® disappeared or its severity decreased within 6 months, regardless of whether the drug was stopped or not. Renal function tests (blood urea nitrogen and creatinine concentrations) in patients with proteinuria were almost always within normal limits. In patients with kidney disease, the protein content in the urine should be determined before starting treatment and periodically throughout the course of therapy. In some cases, against the background of the use of ACE inhibitors, incl. the drug Capoten®, an increase in potassium content in the blood serum is observed. The risk of developing hyperkalemia when using ACE inhibitors is increased in patients with renal failure and diabetes mellitus, as well as those taking potassium-sparing diuretics, potassium supplements, or other drugs that cause an increase in potassium levels in the blood (for example, heparin). The simultaneous use of potassium-sparing diuretics and potassium supplements should be avoided. In addition, when using ACE inhibitors simultaneously with thiazide diuretics, the risk of hypokalemia cannot be excluded, therefore, in such cases, regular monitoring of potassium levels in the blood during therapy should be carried out.
When performing hemodialysis in patients receiving ACE inhibitors, the use of high-permeability dialysis membranes (for example, AN69) should be avoided, since in such cases the risk of developing anaphylactoid reactions increases. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein removal (apheresis) with dextran sulfate. The use of either a different class of antihypertensive drugs or a different type of dialysis membrane should be considered.
In rare cases, during therapy with ACE inhibitors, life-threatening anaphylactoid reactions were observed in patients undergoing desensitization with hymenoptera venom (bees, wasps). In such patients, these reactions were prevented by temporarily stopping ACE inhibitor therapy. Particular care should be taken when desensitization is performed in such patients.
If angioedema develops, the drug is discontinued and careful medical observation is carried out until the symptoms disappear completely. Angioedema of the larynx can be fatal. If the swelling is localized on the face, special treatment is usually not required (antihistamines can be used to reduce the severity of symptoms); if the swelling spreads to the tongue, pharynx or larynx and there is a threat of developing airway obstruction, epinephrine (adrenaline) should be immediately administered subcutaneously (0.3-0.5 ml in a dilution of 1:1000). In rare cases, patients after taking ACE inhibitors experienced angioedema of the intestine, which was accompanied by abdominal pain (with or without nausea and vomiting), sometimes with normal values of C-1-esterase activity and without previous facial edema. Intestinal edema should be included in the differential diagnosis of patients with complaints of abdominal pain while taking ACE inhibitors.
In representatives of the Negroid race, cases of the development of angioedema were noted with greater frequency compared to representatives of the Caucasian race.
In patients with diabetes mellitus receiving hypoglycemic agents (oral hypoglycemic agents or insulin), glycemic levels should be carefully monitored, especially during the first month of therapy with ACE inhibitors.
ACE inhibitors are less effective in blacks than in Caucasians, which may be due to the higher prevalence of low renin activity in blacks.
During major surgery or when using general anesthesia agents that have a hypotensive effect, patients taking ACE inhibitors may experience an excessive decrease in blood pressure. And in these cases, you can increase the volume of circulating blood.
When taking the drug Capoten®, a false-positive reaction may occur when testing urine for acetone.
Reception and speed of action
Take Capoten according to the instructions and prescription of the doctor.
The tablets are swallowed whole (not crushed in any way) one hour before meals and washed down with a significant amount of water.
During the treatment course, it is recommended to take the tablets at the same time every day. Reception is prescribed 2–4 times a day.
Of course, many are interested in the question: “How long does it take for a blood pressure pill to work?” The method of administration plays a big role in the answer to this question. If you need “first aid”, then in order for the medicine to be absorbed at an accelerated rate, it is sometimes advised to place the tablet under the tongue.
In this case, Capoten quickly enters the bloodstream through the mucous membranes and begins to act faster than usual. As patients testify, when the tablet is dissolved, some relief occurs within a few minutes. The dose during resorption remains the same as during normal administration.
In general, due to the high absorption rate of the components, Capoten begins to “work” 10 minutes after entering the body and protects for 6 hours.
Often the patient feels the first signs of relief a little later than the onset of the drug’s effect.
The greatest effect is observed after 60 minutes. Patients are advised to take a relaxed position at this time and wait until the medicine has the desired effect.
A person usually feels relief within 15–20 minutes, depending on individual metabolic characteristics. Breaking and chewing also speeds up the action. If the tablet is absorbed under the tongue, the hypertensive crisis begins to weaken even faster - after 5–10 minutes.
However, you should not use this method often, because a sharp jump down is also unsafe. It should be recalled that Capoten can cause mental retardation and dizziness, so it is used with caution when it is necessary to control various mechanisms and engage in hazardous activities.
Combining any food with tablets slows down the absorption of the drug in the gastrointestinal tract by approximately 30-40%, which naturally affects the process of reducing blood pressure.
In some cases, to provide emergency care to patients, you need to use two tablets (with a mandatory break of up to 30 minutes). The blood pressure between and after taking the pills must be monitored very carefully in order to respond in time to changes in indicators.
Dosage
In order to understand how quickly Capoten lowers blood pressure, you need to remember that it is intended for long-term use. Only completing the full course guarantees the absence of sudden and dangerous rises in pressure. The treatment regimen also plays an important role.
One of the main requirements for organizing treatment is a gradual adjustment of the dose towards an increase, after the doctor determines the degree of effectiveness of the medicine.
Dosage changes occur no earlier than 14–21 days after the previous prescription. Typically, the initial dosage for hypertension is 12.5 mg twice a day, and for heart failure and myocardial infarction - 6.25 mg. To achieve a good therapeutic effect for hypertension, it is increased to 50 mg (morning and evening).
It should be recalled that you can not be afraid of arterial hypertension only if you take it regularly. Indeed, despite the possibility of using the drug during a hypertensive crisis, the therapeutic effect after a single dose will be noticeable for a short time.
If arterial hypertension is unsystematic, then the initial single dose is 6.25 mg, and the number of doses is 3 (during the day).
In the future, 25 mg is prescribed three times a day in order to keep the indicators normal. If a severe form of the disease is diagnosed, the maximum acceptable daily dose reaches 150 mg.
Patients cannot change the dosage on their own, because only a doctor can choose the correct regimen for taking Capoten, especially if we are talking about chronic diseases or there are other concomitant health problems.
Capoten
Arterial hypotension
In patients with arterial hypertension, when using captopril, severe arterial hypotension is observed only in rare cases. The likelihood of developing this condition increases with increased fluid loss and hyponatremia (for example, after intensive treatment with diuretics, restriction of sodium intake, in patients on dialysis, and in patients with diarrhea or vomiting).
Captopril should be prescribed with caution to patients on a low-salt or salt-free diet. Circulating blood volume and blood sodium levels should be adjusted before captopril is prescribed.
The possibility of a sharp decrease in blood pressure can be minimized by first withdrawing (4-7 days before) the diuretic or increasing sodium chloride intake (about a week before starting treatment), or by prescribing low doses of captopril at the beginning of treatment (6.25-12 .5 mg/day).
Renal function should be regularly monitored before and during treatment with captopril. Excessive reduction in blood pressure due to antihypertensive medications may increase the risk of myocardial infarction or stroke in patients with coronary heart disease or cerebrovascular disease. If arterial hypotension develops, the patient should take a horizontal position with legs elevated. Intravenous administration of 0.9% sodium chloride solution may be required.
In patients with CHF, a transient decrease in blood pressure by more than 20% of the initial value is observed in approximately half of the cases. The degree of reduction in blood pressure is maximum in the early stages of treatment (after taking the first few doses of captopril) and stabilizes within one to two weeks from the start of treatment. Blood pressure usually returns to baseline without a decrease in therapeutic efficacy within two months.
In patients with CHF, treatment should begin with low doses of captopril (6.25-12.5 mg/day) under medical supervision. Increasing the dose of captopril should be done with extreme caution. Transient arterial hypotension in itself is not a reason to discontinue treatment. In cases where arterial hypotension becomes stable, the dose should be reduced and/or discontinued use of the diuretic and/or captopril.
Aortic or mitral stenosis/hypertrophic obstructive cardiomyopathy
Like all drugs that have a vasodilating effect, ACE inhibitors should be used with extreme caution in patients with left ventricular outflow tract obstruction. In case of hemodynamically significant obstruction, the use of captopril is not recommended.
Renal dysfunction
Some patients with kidney disease, especially those with severe renal artery stenosis, experience increases in serum urea nitrogen and creatinine concentrations after lowering blood pressure. This increase is usually reversible when captopril therapy is discontinued. In these cases, it may be necessary to reduce the dose of captopril and/or discontinue the diuretic.
With long-term use of captopril, approximately 20% of patients experience an increase in serum urea and creatinine concentrations by more than 20% compared with normal or baseline values.
In less than 5% of patients, especially with severe nephropathy, treatment discontinuation is required due to an increase in creatinine concentration.
Renovascular hypertension
Patients with bilateral renal artery stenosis or stenosis of the artery of a solitary kidney have an increased risk of developing arterial hypotension and renal failure when using ACE inhibitors. Renal failure may initially manifest itself as only slight changes in plasma creatinine levels. The use of captopril in such patients is not recommended.
Kidney transplant
There is no experience with the use of captopril in patients who have recently undergone kidney transplantation. Therefore, the use of captopril in such patients is not recommended.
Proteinuria
When using captopril, 0.7% of patients had proteinuria more than 1000 mg per day. In 90% of cases, proteinuria occurred in patients with impaired renal function, as well as when using high doses of captopril (more than 150 mg per day). Approximately 20% of patients with proteinuria developed nephrotic syndrome. In most cases, proteinuria disappeared or decreased in severity after taking captopril within 6 months, regardless of whether the drug was stopped or not. Renal function tests (blood urea nitrogen and creatinine concentrations) in patients with proteinuria were almost always within normal limits. In patients with kidney disease, the protein content in the urine should be determined before starting treatment and periodically throughout the course of therapy.
Liver dysfunction
In rare cases, the use of ACE inhibitors has been accompanied by the development of a syndrome that begins with the appearance of cholestatic jaundice or hepatitis and progresses to fulminant liver necrosis, sometimes with death. The mechanism of development of this syndrome is unknown. If a patient receiving ACE inhibitor therapy develops jaundice or a significant increase in liver enzyme activity, captopril treatment should be discontinued and appropriate adjuvant therapy should be instituted. The patient should be under appropriate supervision.
Neutropenia/agranulocytosis/thrombocytopenia/anemia
Cases of neutropenia/agranulocytosis, thrombocytopenia and anemia have been reported in patients taking ACE inhibitors. Neutropenia is rare in patients with normal renal function and no other abnormalities. In renal failure, simultaneous administration of captopril and allopurinol led to neutropenia.
Captopril should be used with extreme caution in patients with systemic connective tissue diseases (systemic lupus erythematosus, scleroderma, etc.) taking immunosuppressants, allopurinol or procainamide, or a combination of these complicating factors, especially if there are pre-existing renal dysfunction.
In 13% of cases with neutropenia, death was observed. In almost all cases, death was observed in patients with connective tissue diseases, renal or heart failure, while taking immunosuppressants, or a combination of both of these factors.
Due to the fact that the majority of fatal cases of neutropenia due to ACE inhibitors developed in such patients, their white blood cell count should be monitored before starting treatment, in the first 3 months - every 2 weeks, then every 2 months. In all patients, the number of leukocytes in the blood should be monitored monthly in the first 3 months after starting captopril therapy, then every 2 months. If the number of leukocytes is below 4000/μl, a repeat general blood test is indicated; below 1000/μl, the drug is stopped while monitoring the patient continues. Typically, restoration of the number of neutrophils occurs within 2 weeks after discontinuation of captopril.
Some patients developed serious infectious diseases, which in some cases did not respond to intensive antibiotic therapy. When using captopril in patients with a high risk of neutropenia/agranulocytosis, regular monitoring of the number of leukocytes in the blood is recommended. Patients should be warned to seek immediate medical attention if any signs of an infectious disease (eg, fever, sore throat) occur.
Hypersensitivity reactions/angioedema
Rare cases of angioedema of the face, extremities, lips, tongue, vocal folds and/or larynx have been observed with the use of ACE inhibitors, including captopril. Angioedema may develop at any time during treatment.
If angioedema develops, you should immediately stop taking captopril and carefully monitor the patient's condition until symptoms disappear completely.
If the swelling is localized to the face, no special treatment is usually required (antihistamines can be used to reduce the severity of symptoms). Even in cases where only swelling of the tongue is observed without the development of respiratory distress syndrome, patients may require long-term observation, since therapy with antihistamines and corticosteroids may not be sufficient.
Angioedema, associated with swelling of the larynx and tongue, can be fatal in very rare cases. If the swelling spreads to the tongue, pharynx or larynx and there is a threat of developing airway obstruction, 0.3-0.5 ml of a 0.1% solution of epinephrine (adrenaline) should be immediately administered subcutaneously and/or ensure airway patency ( intubation or tracheostomy).
In rare cases, during therapy with ACE inhibitors, intestinal edema (angioedema of the intestines) has developed, which is manifested by abdominal pain in combination with or without nausea and vomiting, sometimes without previous angioedema of the face and with normal levels of C1-esterase. Diagnosis is made using abdominal computed tomography, ultrasound, or surgery. Symptoms disappeared after stopping the ACE inhibitors. The possibility of developing intestinal edema must be taken into account when carrying out the differential diagnosis of abdominal pain in patients taking ACE inhibitors.
Patients with a history of angioedema not associated with ACE inhibitors may be at greater risk of developing angioedema during ACE inhibitor therapy.
In representatives of the Negroid race, cases of the development of angioedema when using ACE inhibitors were observed with a higher frequency compared to representatives of other races.
An increased risk of angioedema was observed in patients concomitantly taking ACE inhibitors and drugs such as mTOR inhibitors (temsirolimus, sirolimus, everolimus), dipeptidyl peptidase type IV inhibitors (sitagliptin, saxagliptin, vildagliptin, linagliptin), estramustine, neutral endopeptidase inhibitors (racecadotril). , sacubitril) and tissue plasminogen activators.
Anaphylactoid reactions during desensitization with an allergen from Hymenoptera venom
In rare cases, during therapy with ACE inhibitors, life-threatening anaphylactoid reactions were observed in patients undergoing desensitization with an allergen from the venom of Hymenoptera. In such patients, these reactions were prevented by temporarily stopping ACE inhibitor therapy before desensitization began. The use of captopril should be avoided in patients receiving bee venom immunotherapy.
Anaphylactoid reactions during low-density lipoprotein apheresis (LDL apheresis)
Life-threatening anaphylactoid reactions have rarely been observed in patients taking ACE inhibitors during LDL apheresis using dextran sulfate. The development of these reactions can be prevented by temporarily discontinuing the ACE inhibitor before each LDL apheresis procedure.
Hemodialysis using high-flow membranes
When performing hemodialysis in patients receiving ACE inhibitors, the use of high-flow polyacrylonitrile dialysis membranes (for example, AN69®) should be avoided, since in such cases the risk of developing anaphylactoid reactions increases. In such cases, it is necessary to use a different type of dialysis membrane or use antihypertensive drugs of other classes.
Diabetes
In patients with diabetes mellitus receiving oral hypoglycemic agents or insulin while using ACE inhibitors, blood glucose concentrations should be regularly monitored.
Patients taking oral hypoglycemic agents or insulin should be informed before starting the use of ACE inhibitors of the need to regularly monitor blood glucose concentrations (hypoglycemia), especially during the first month of simultaneous use of these drugs.
Cough
When taking ACE inhibitors, a characteristic cough is often observed. As a rule, the cough is non-productive, constant and stops after discontinuation of the drug. Cough associated with the use of ACE inhibitors should be considered in the differential diagnosis of dry cough.
Surgical interventions / general anesthesia
During major surgical operations, as well as when using general anesthesia agents that have an antihypertensive effect, patients taking ACE inhibitors may experience an excessive decrease in blood pressure (since captopril blocks the formation of angiotensin II, caused by compensatory release of renin). In such cases, to correct low blood pressure, measures aimed at increasing the volume of circulating blood are used.
Hyperkalemia
In some cases, against the background of the use of ACE inhibitors, incl. captopril, an increase in serum potassium levels is observed.
Risk factors for the development of hyperkalemia are renal failure, old age (over 65 years), diabetes mellitus, some concomitant conditions (decrease in blood volume, acute heart failure in the stage of decompensation, metabolic acidosis), simultaneous use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene or amiloride), as well as potassium preparations, potassium-containing table salt substitutes and other drugs that increase the level of potassium in the blood plasma (such as heparin, tacrolimus, cyclosporine; drugs containing co-trimoxazole [trimethoprim + sulfamethoxazole]).
The use of potassium supplements, potassium-sparing diuretics, or potassium-containing table salt substitutes, especially in patients with impaired renal function, can lead to a significant increase in serum potassium levels. Hyperkalemia can cause serious heart rhythm disturbances, sometimes fatal. It is recommended to avoid the simultaneous use of potassium-sparing diuretics and potassium supplements. If it is necessary to simultaneously use captopril and the drugs listed above containing potassium or increasing the potassium content in the blood plasma, caution should be exercised and the potassium content in the blood serum should be regularly monitored.
Hypokalemia
When using ACE inhibitors simultaneously with thiazide diuretics, the risk of hypokalemia cannot be excluded. Therefore, in such cases, regular monitoring of potassium levels in the blood should be carried out during therapy.
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
The simultaneous use of drugs from different groups that act on the RAAS is not recommended (double blockade of the RAAS), since it has been associated with an increased incidence of side effects such as arterial hypotension, hyperkalemia, and decreased renal function (including acute renal failure). The simultaneous use of ACE inhibitors with medicinal products containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
In cases where the simultaneous administration of two drugs acting on the RAAS is necessary, their use should be carried out under the supervision of a physician with extreme caution and with regular monitoring of renal function, blood pressure and electrolyte levels in the blood plasma.
Lithium preparations
The simultaneous use of captopril and drugs containing lithium is not recommended due to the risk of potentiating the toxicity of the latter.
Ethnic differences
ACE inhibitors are less effective in blacks than in Caucasians, which may be due to the higher prevalence of low renin activity in blacks.
Other
When taking captopril, a false-positive urine test for acetone may occur.
Features of interaction with alcohol
It is dangerous to combine Capoten with ethanol contained in any alcoholic drink.
Since captopril, the main element of these tablets, tends to accumulate potassium in the body, the lack of which provokes disturbances in the functioning of blood vessels.
Alcohol-containing drinks activate its elimination. Therefore, treatment not only loses its meaning, but also contributes to the development of persistent hypertension.
Therefore, forget that alcohol dilates blood vessels, the opposite effect soon occurs, and no one has canceled the hangover syndrome. Sometimes the pressure does not rise regularly, and if this happens after drinking alcohol, then the tablet can be swallowed, but only as an exception and for the necessary normalization of the condition before the doctor arrives.
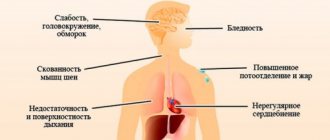
In this situation, the likelihood of such negative consequences increases: numbness and a feeling of cold in the extremities, tremors, loss of taste, as well as extremely dangerous pulmonary edema. In addition, in case of renal failure, taking these tablets is completely prohibited in any case. Another pitfall is that alcohol enhances the effect of the drug. In this case, an overdose and a hypotonic crisis occurs.
People who, for the sake of an “experiment,” try to drink alcohol to speed up the action of Capoten, risk greatly aggravating their health condition.
Indications and contraindications for therapy with Capoten
The instructions for the medication indicate the pathologies for which therapy is permitted. Capoten is used for patients:
- with hypertension;
- chronic heart dysfunction;
- AMI;
- dysfunction of the left ventricle;
- diabetic nephropathy arising against the background of type 1 diabetes mellitus.
Capoten is contraindicated:
- in case of individual intolerance to the component composition;
- registered Quincke's edema, which arose under the influence of ACE;
- kidney and liver dysfunction;
- excess potassium;
- narrowing of the lumens of arterial vessels in the kidneys, conditions after organ transplantation;
- aortic valve stenosis and changes leading to problems with the removal of blood from the left ventricle;
- when treated with Aliskiren or similar medications in patients with severe renal impairment or diabetes mellitus;
- pregnancy, breastfeeding, adolescence;
- lactase deficiency, lactose allergy.
Particular caution when taking Capoten is necessary for patients:
- with hypotension, CHF, ischemic heart disease;
- liver dysfunction, systemic connective tissue lesions;
- disorders of the kidneys, hemodialysis;
- excess potassium, diabetes;
- spontaneous allergic reactions;
- during surgical interventions, general anesthesia, and taking potassium-sparing diuretics.
Doctors' supervision is required for patients over 65 years of age, while taking lithium drugs, and for representatives of the Negroid race.
Video on the topic
Review of drugs for hypertension and cardiovascular diseases Capoten and Captopril:
Capoten is one of the most effective drugs for high blood pressure. It is popular due to its efficiency, high speed, and affordable cost. The drug has proven itself in systemic treatment, and it can also be used as an “ambulance” for hypertensive crises, since when absorbed, it begins to act within a matter of minutes.
The information on the MyMedNews.ru website is for reference and general information, collected from publicly available sources and cannot serve as a basis for making a decision on the use of medications in the course of treatment.
MyMedNews.ru
And we also have
Medicines for high blood pressure from the “by-catch” group: list of drugs and features of their use