Norm of leukocytes in the blood of children: Pexels A general blood test will help you understand whether everything is in order with the number of leukocytes in the blood in a child. Since they protect the body from infections, you should pay attention to this indicator. Experts explain that the number of leukocytes depends on the age of the child and can change under the influence of various factors.
Symptoms
Elevated leukocytes in a child’s blood have their own clinical picture.
It is worth noting that the symptoms expressed in this disorder are nonspecific and cannot accurately indicate the course of this particular disorder. In addition, external manifestations characteristic of this condition may go unnoticed, since the symptoms of the underlying disease often come to the fore.
It is very difficult to determine the increase in the number of white blood cells in the blood of an infant. This is due to the fact that infants cannot describe their condition and sensations in words.
Symptoms that develop due to the fact that the child’s white blood cells have increased include:
- constant fatigue;
- loss of appetite;
- increase in temperature indicators;
- dizziness;
- profuse sweating;
- sleep disorder;
- slight decrease in visual acuity;
- muscle and joint pain;
- weight loss;
- frequent mood changes;
- increased moodiness and tearfulness in infants;
- problems with concentration in older children;
- decreased physical activity.
Such external manifestations are common to all age categories. The only difference may be the intensity of symptoms.
Children's blood tests and vaccinations
A clinical blood test in the Russian Federation is included in the standard examination before vaccination. My opinion is that most often it is completely unnecessary if, for example, the child appears healthy and there are no complaints. Nevertheless, the analysis is carried out and the results are often interpreted completely inadequately.
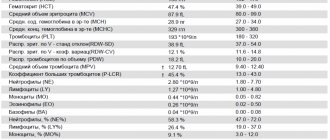
Many laboratories simply forget about the fact that the interpretation of the results of a child’s blood test has its own characteristics. And they simply write analyzes on standard forms, where “norms” are printed in a column next to the analysis results. But children’s indicators cannot be compared with these standards!
About children's hemoglobin standards
How much hassle these forms with “deviations” from the norm cause parents! How many alarming calls and letters fall upon the pediatrician! My colleagues and I are forced every day to dispel the fears of parents who are trying to independently evaluate the results of their children’s tests.
For example, hemoglobin
. In adults, its norm is from 120 to 150 g/l. For children, everything is more complicated. If immediately after birth “normal” hemoglobin is 180–220 g/l, then by 2–3 months of life its level rapidly drops to the lower limit of normal, which starts at 90 g/l. This is the so-called physiological anemia. And since this is the norm, there is no need to treat it.
Diagnosis of leukocytosis
Why does a child under one year bleed from the nose?
With leukocytosis, the number of “white” blood cells increases compared to their normal value. The increase may be slight or severe.
Thus, the level of leukocytes increases after eating or during exercise. These are physiological processes and do not pose any danger. After a short period of time, the indicators return to normal. If such growth is considered as a pathological reaction of the body, we are talking about an inflammatory process.
The famous pediatrician Komarovsky recognizes the need for a general blood test. It, first of all, allows you to determine the nature of the disease, bacterial or viral. This is the basis for subsequent treatment. If the body is attacked by bacteria, then it will be difficult to cope without antibiotics, but they have no effect on viruses. Therefore, their use does not make sense, just like the use of antiviral drugs. Immunity to them is usually developed on days 6-7, and the body copes on its own. If this does not happen and the disease develops, most likely a bacteria has joined.
Possible symptoms in a child
When a child's white blood cell count is elevated, it not only indicates that he or she is sick, but also that the immune system is active. The body's defenses began to fight pathogenic microorganisms.
- Why do women have an increase in leukocytes in the blood?
The following symptoms may indicate leukocytosis in a child:
- Increased body temperature without identifying the cause;
- Weakness and dizziness;
- Indigestion, lack of appetite, weight loss;
- Nausea, vomiting;
- Headache and migraine;
- Aches in joints and muscles;
- Sleep disorder, most often insomnia. The child becomes anxious and shudders;
- Increased sweating;
- Moodiness and irritability.
An infant will not be able to talk about his health; parents only have to guess about existing problems. What should alert you is that the baby’s behavior has changed, he is not the same as before. When this happens once, and then the baby becomes himself again, then there is no need to worry. If the condition drags on, behavior and well-being worsen, then you need to consult a pediatrician.
Upset child
We must remember! In a baby, a temperature of up to 37.5° is considered normal. At the same time, he is calm and active, no unpleasant symptoms are observed. This is often due to uncomfortable indoor conditions and too warm clothing. If the temperature is higher and the baby begins to act up, you should consult a doctor.
What is leukocytosis and leukocyte norms in children
Eating leads to a transient increase in leukocytes
Leukocytosis is an increase in the number of leukocytes in the blood. The number of white cells in the bloodstream varies throughout the day. There are a little more of them after physical activity, emotional experiences, and eating food. But significant growth indicates the presence of a pathological process in the body.
The normal level of leukocytes directly depends on the age of the child. When a baby is born, it only encounters millions of bacteria, so its immune system works especially actively. The number of protective cells during this period is high, the immune system is just being formed. Gradually, having learned to fight harmful pathogens, leukocytes decrease in number.
- Leukocytosis (increased white blood cells in the blood): normal or pathological?
In the analysis form, leukocytes are abbreviated WBC. For a more reliable study, it is recommended to know not only the total number of leukocytes, but also the percentage of their varieties in the child’s blood (leukocyte formula).
White blood cell levels in children depend on age
| Age | Leukocytes (10^9/l) | Band neutrophils (%) | Segmented neutrophils (%) | Eosinophils (%) | Basophils (%) | Lymphocytes (%) | Monocytes (%) |
| 1 day - 1 month | 8,5 — 24,5 | 1 — 17 | 45 — 80 | 0,5 — 6 | 0 — 1 | 12 — 36 | 2 — 12 |
| 1 – 6 months | 6,5 — 13,5 | 0,5 — 4 | 15 — 45 | 0,5 — 7 | 0 — 1 | 40 — 76 | 2 — 12 |
| 6 – 12 months | 5,5 — 12,5 | 0,5 — 4 | 15 — 45 | 0,5 — 7 | 0 — 1 | 42 — 74 | 2 — 12 |
| 14 years | 6 — 12 | 0,5 — 4 | 15 — 45 | 0,5 — 7 | 0 — 1 | 38 — 72 | 2 — 12 |
| 4 – 7 years | 5 — 12 | 0,5 — 5 | 25 — 60 | 0,5 — 7 | 0 — 1 | 25 — 60 | 2 — 10 |
| 7 – 12 years | 4,5 — 10 | 0,5 — 5 | 35 — 65 | 0,5 — 7 | 0 — 1 | 24 — 54 | 2 — 10 |
| 12 – 15 years | 4,3 — 9,5 | 0,5 — 6 | 40 — 65 | 0,5 — 6 | 0 — 1 | 22 — 50 | 2 — 10 |
Leukocytes or white blood: evolution of the immune system
Leukocytes are different. Some are responsible for fighting bacteria, others deal with viruses, others “specialize” in very large adversaries - for example, in plant cells (this happens more often than you think - I mean an allergy to pollen) or even in multicellular scoundrels - worms.
So looking at the total white blood cell count during an acute infection is good, but damn low. At best, the doctor will determine that there is an infection. But to understand what exactly caused this infection, you need to look at which leukocytes are elevated. This study is called the leukocyte formula.
That's what we'll talk about.
Norms
The main changes in the red blood of children occur not only up to a year, but up to a month, and this is due to the fact that during the first month of life, traces of the transition to lung breathing still remain in the child’s blood. With the immune system, everything is much more complicated - it changes continuously during the first six years of life, and extremely unevenly. So, get ready: there will be more numbers.
Leukocytes . They are WBC. Their number is measured in billions per liter of blood (which, compared to red blood cells, seems somehow frivolous). And since at birth a child moves from a sterile environment (the mother’s womb) to an extremely unsterile environment, the number of leukocytes, even normally, in children is much higher than in adults. True, it decreases with age. In a one-month-old child, the normal rate of leukocytes in the blood is from 6.5 to 13.8, at six months from 5.5 to 12.5, from one year to six years (yes, at the very time when the child most often gets sick) from 6 to 12. And only when the child’s immunity becomes strong enough to withstand numerous infections, the number of leukocytes approaches the number in adults - from 4.5 to 9 (some for some reason consider 12 to be the norm, but this is not entirely true).
Neutrophils , also known as NEU. Their number is counted not in absolute units (how many per liter of blood) but as a percentage of the total number of leukocytes. The task of these cells is to fight bacteria. It's a pretty fair fight: neutrophils simply eat the unwary bacterial cells and digest them. True, in addition to bacterial cells, neutrophils also act as a kind of cleaners - in exactly the same way they remove any cellular debris from the body, not just microbes.
There are different neutrophils: there are band neutrophils (these are a kind of juniors among the eater cells), but there are not very many of them in the blood - things like destroying infections are not a child’s task. Their number almost does not change with age: in a one-month-old, one-year-old, and even a six-year-old child, it is from 0.5 to 4.5%. Only in children over seven years of age (as, indeed, in adults) the upper limit of the norm for band neutrophils rises to 6%. The child has grown, the body has become stronger - the immune system is ready for invasion.
But the real “workhorses” of the immune system are segmented neutrophils - by the way, they are the main and almost the only protection for children under 2 years of age. In children under one year of age, the normal number is from 15 to 45%, and from one to six years of age (when work increases significantly), the number of neutrophils increases significantly - from 25 to 60%. Finally, by the age of seven, the number of segmented neutrophils reaches the adult norm. True, this norm is very vague - from 30 to 60%. That is, thirty percent is the norm, and sixty is the norm too.
Monocytes , also known as MON. These are the “younger brothers” of neutrophils . For the time being, they sit in the tissues, and only rarely emerge into the blood. Normally, their number does not exceed 2 to 12% in children under one year old or from 2 to 10% in children over one year old. Adults and children are no different in this indicator - still the same 2-10%. True, when there is a catastrophic shortage of neutrophils monocytes and the number of monocytes in the blood, although not greatly, increases.
Eosinophils , also known as EOS. It is rumored that eosinophils are responsible for allergic reactions. To put it mildly, this is not entirely true. Eosinophils do not produce class E immunoglobulins, the level of which is increased in allergy sufferers. Eosinophils , if you like, are the “highest caste” of eater cells (before this, we talked about neutrophils and monocytes as eater cells). They are able to devour everything that is not capable of consuming themselves. Even multicellular aggressors (worms) and very large foreign cells (for example, intestinal amoebas) are desperately afraid of eosinophils . The fact is that eosinophils do not swallow cells - they stick to them, inject their digestive enzymes into the cells and then suck out the contents of these cells, like a child sucking out a liter carton of juice. Just turn away - and all that remains from the package (in our case, from a small worm, for example) is an empty shell. Normally, eosinophils in the blood - from 0.5 to 6%
Lymphocytes , also known as LYM. These are the main cells of the mature immune system. Their specialization is the fight against both viruses and bacteria. But especially recklessly, lymphocytes deal either with viruses or with their own cells, which, due to the naivety of these viruses, have sheltered. Normally, the blood of a child under one year of age lymphocytes , although they work, to be honest, at half capacity. But when the baby’s immune system begins to develop (I remind you, the development of the immune system after a year and ends mainly by 6-7 years), the number of lymphocytes in the blood drops quite sharply - to 26-60%. Finally, after 7 years, lymphocytes “stop” at around 22-50%.
Basophils, BAS. Just young lymphocytes. Their number never exceeds 1%.
All. Uf-f-f-f...
Advertising
How to treat leukocytosis?
Treatment can be prescribed only after the exact cause of this phenomenon has been established, for example, physiological leukocytosis is considered to be the norm. As soon as the causative agent of the infection is detected, the following drugs may be prescribed to the small patient:
- Antiviral agents that effectively fight viruses.
- In severe cases, antibiotics may be prescribed, but they are taken only as prescribed by a doctor.
- Chemotherapy drugs that are aimed at maintaining the immune system.
Sometimes, when leukocytosis is detected in children and the blood has a viscous consistency, leukapheresis is prescribed, during which the blood is purified.
How is the analysis performed?
When testing blood for a general or, as it is also called, clinical analysis, the child should, if possible, be hungry, i.e., the procedure is done on an empty stomach. Typically, blood collection rooms in clinics are open from 8.00. until 9.30. At this time, blood levels in the body are the most optimal.
Blood must be donated on an empty stomach, because after eating, the stomach begins to work actively and the number of leukocytes may increase, and this, in turn, may give the doctor incorrect information about the child’s health status. Also, before taking the test, you should not undergo any procedures, such as x-rays, FGDS and various physiotherapeutic procedures, this can also lead to an increase in leukocytes in the blood. [adsen]
“Children’s” blood tests: how to avoid retakes
Testing a child's blood is a difficult test for parents. And not many people know that improper preparation can make all efforts in vain. Why is preparation so important? And how to avoid distorted results?
Why on an empty stomach?
In the recommendations for most blood tests you can see the word “at least 3 hours after eating.” And that's why.
1. Eating triggers many biochemical processes, including the release of immune cells. Therefore, even a routine general blood test should not be taken on a full stomach, so as not to get “falsely high” leukocytes.
Not to mention biochemical (glucose, cholesterol, total protein) and hormonal studies.
2. Eating food, especially fatty, fried and smoked food before and the day before the test, changes the physicochemical properties of the serum, in particular its transparency and optical density.
Increased whey turbidity:
- firstly, it complicates the search and binding of the desired analyte in the material, and therefore distorts the results;
- and secondly, too many lipids in the blood can provoke chylosis (turbidity of the serum), in which the determination of certain substances is impossible.
For this reason, it is recommended that absolutely all tests be taken at an interval after eating:
- for children under 2 years of age - closer to the next feeding, but not less than 2-3 hours of fasting,
- from 2 to 14 years (inclusive) – at least 6-8 hours.
How about water
Few people know, but tea, coffee or juice are food for the body, not water. And therefore, mild dehydration is quite widespread.
At the same time, even a slight deficiency of fluid in the body leads to “thickening” of the blood. This not only complicates the sampling procedure itself, but leads to distortion of some results.
So, in the same general blood test, red blood cells, hemoglobin and platelets may be elevated, which can mask a mild degree of anemia and other diseases. And in some cases, such results may require a retake or additional studies to exclude serious pathologies.
Thus, the drinking regime before tests is no less important than the food intake. Therefore, water can and should be drunk as usual, especially in hot weather and dry microclimate in the house.
Stress is no friend to analysis
We are talking primarily about the effect of stress on vascular tone and blood clotting.
For example, a strong cry from a child during blood collection not only complicates the procedure itself due to spasm of small vessels, but can also lead to the formation of clots in the material and its unsuitability for analysis.
Among other things, cortisol (the stress hormone) significantly changes many biochemical (especially glucose) parameters. Therefore, maximum psychological support for the child both at the preparation stage and during collection is as important as drinking and eating regimens.
And in order to minimize the child’s stress level, you can get tested in your usual home environment, using the service of a nurse visiting your home.