Causes, consequences
Various factors contribute to atherosclerosis of the penile vessels: reluctance to exercise, lack of exercise, deterioration in the quality of nutrition. Lack of regular sex life, excess weight, and high blood clotting play an important role. Predisposing factors are age over 50 years, a genetic tendency to develop blood circulation disorders, and previous injuries to the perineum.
Consequences of atherosclerosis of the vessels of the penis:
- lack of libido;
- atrophy of the testicular structure;
- weakening of erection, in later stages – dysfunction of varying severity;
- deformation of the reproductive organ - curvature in one direction due to uneven blood supply to the tissues;
- the appearance of benign prostatic hyperplasia;
- impotence, which, if left untreated, enters a protracted stage.
The listed consequences serve as the basis for immediate contact with a urologist.
Atherosclerosis, arterial hypertension, drugs and erectile dysfunction
Drug therapy is the cause of one in four cases of erectile dysfunction
Erectile dysfunction (ED) is the inability to achieve and/or maintain an erection sufficient for satisfying sexual activity. The term was proposed in 1988 by the US National Institutes of Health instead of the word “impotence”, and by 1992 it was adopted by international organizations of urologists and andrologists. This definition more fully and accurately characterizes the variety of expressed sexual disorders. It includes not only the inability to keep the penis erect, but also a violation of orgasm (which is the highest degree of voluptuous sensation that occurs at the moment of completion of sexual intercourse) and a weakening of libido (sexual desire).
If previously various psychological problems were considered the main cause of ED, in recent years this opinion has changed. Thanks to studies that have clarified the true mechanism of erection, it has been shown that ED in 80% of cases occurs as a complication of various somatic diseases (Carrier S. et al., 1993; Benet AE et al., 1995). The presence of ED is often associated with chronic diseases, primarily arterial hypertension (AH), diabetes mellitus and atherosclerosis (Feldman HA et al., 1994). With atherosclerosis, the walls of blood vessels lose their elasticity and narrow due to the atherosclerotic plaques covering them, which leads to the development of heart attacks and strokes. Atherosclerotic damage to the vessels of the penis prevents sufficient blood flow into the organ and causes ED. This disease is associated with approximately 40% of cases of ED in men over 50 years of age. Often, various manifestations of atherosclerosis - for example, coronary heart disease (CHD) and ED - develop in parallel. Thus, according to preliminary data from Winstrup R., the frequency of sexual intercourse in men after the onset of heart disease decreases from 6.9 + 4.3 per month to 2.8 + 2.0, and the frequency of ED increases from 20 to 65%. Moreover, there is evidence of a correlation between sexual activity and the number of affected coronary arteries (Greenstein A. et al., 1997).
High blood pressure (BP) can cause ED, regardless of whether a person suffers from atherosclerosis or not. If hypertension is not treated for a long time, the walls of blood vessels, constantly exposed to increased blood pressure, become dense and inelastic, and the vessels cannot supply the organs with the necessary amount of blood.
25% of cases of ED are in one way or another associated with taking medications (Slag MF et al., 1983; O'Keefe M. et al., 1995). These data are based on empirical observations, case reports, pre- and post-marketing studies of drugs (Goldstein I. et al., 1983). However, very few patients are aware of the possibility of impaired potency under the influence of medications. According to a public survey examining sexual activity in older men (Hamdy FC et al., 1997), 64% of men in Spain, 51% in France, and 38% in the UK are aware of the possibility of medications affecting sexual function.
However, a patient who suspects that drug treatment is causing his sexual problems may stop taking the medication or reduce the dose without telling the doctor. Thus, according to Arabidze G.G. (1999), only 30% of patients with arterial hypertension in Russia continue to take prescribed medications a year after the selection of antihypertensive therapy, and in 15% of cases the reason for refusing therapy was sexual disorders.
The main groups of drugs used in cardiology, which are believed to have a negative effect on male sexual function, are presented in the table.
ED is associated with the use of digoxin (Guay AT, 1995), antihypertensive drugs - clonidine, thiazide diuretics, β-blockers (Buffum J., 1986), antihyperlipidemic drugs, which have different effects on libido, erection and ejaculation. Drug-induced priapism, which is often followed by ED, includes approximately 30% of cases of priapism and is caused primarily by drugs that affect α-adrenergic receptors - antihypertensive drugs (mainly prazosin), as well as heparin (Baanos JE et al., 1989).
Most often, the occurrence of ED is associated with the use of various antihypertensive drugs. Thus, the Massachusetts Male Aging Study (MMAS, 1994) found that the incidence of ED among hypertensive men receiving drug therapy was 15%. Until now, however, it remains unclear whether this problem is associated with hypertension itself or with antihypertensive therapy, since not all antihypertensive drugs cause ED. In particular, to date there is no indication that calcium antagonists and ACE inhibitors can negatively affect male sexual function. Double-blind randomized study Fogari R. et al. (1998) showed that the frequency of sexual intercourse per month during atenolol therapy decreased from 7.8 to 4.5 after a month and to 4.2 after 4 months. During therapy with lisinopril, the corresponding indicators were 7.1, 4.0 and 7.7, that is, sexual activity was completely restored by the end of the four-month observation. The percentage of patients who reported sexual disorders was also significantly higher during therapy with atenolol compared with the lisinopril group (17% and 3%, respectively). As for angiotensin receptor inhibitors, a randomized double-blind crossover study by Fogari R. et al. (1999) showed that while taking valsartan, there was even a tendency to increase sexual activity in men. The study involved 94 hypertensive men aged 40–49 years with newly diagnosed arterial hypertension who had not previously been treated. After taking placebo for a month, patients received the angiotensin receptor antagonist valsartan (Diovan) or the α-, β-blocker carvedilol for 16 weeks. Then, after taking placebo for 4 weeks, patients were assigned to another study drug and followed for an additional 16 weeks. In the group of patients taking valsartan after a month, the number of sexual intercourses per week decreased from 2.1 to 1.6; at the end of 16 weeks, the sexual activity score was 2.7, and after switching to carvedilol it dropped to 0.9 by the end of the study. In the carvedilol group, the level of sexual activity decreased from 2.2 to 1.1 at the end of the first month of treatment and to 0.9 at the end of 16 weeks of observation, and after switching to valsartan it increased to 2.6.
Thus, although ED during antihypertensive therapy may occur due to a decrease in blood flow to the penis, it is unclear, however, whether this decrease is a consequence of the decrease in systemic blood pressure with effective antihypertensive therapy, the result of vascular disease, or some other unknown factor at work. side effects of the drug (Bansal S., 1988).
The latter assumption is supported by the results of a study by Muller SC et al. (1991), who assessed the presence of ED in 472 patients with hypertension. According to duplex sonography, patients receiving antihypertensive therapy showed a worse arterial response to intracavernosal papaverine administration than those who did not receive drug treatment. The vascular response to papaverine was more favorable in patients receiving a combination of a beta-blocker and a vasodilator, and the use of thiazide diuretics as monotherapy or in combination with other antihypertensive agents worsened arterial function. However, the level of blood pressure reduction did not correlate with the ability to achieve a full erection after intracavernous injection of papaverine. In the experiment Lin SN et al. (1988) injection of low doses of clonidine into the pudental artery of dogs, which were unable to affect systemic blood pressure, suppressed erection induced by electrical stimulation. The authors believe that this may be due to local narrowing of the penile arteries, mediated by the effect of clonidine on α-adrenergic receptors.
Among antihypertensive drugs, thiazide diuretics most reliably cause ED. The multicenter, randomized, placebo-controlled TAIM study (1991) showed that ED was observed in 28% of patients receiving chlorthalidone for 6 months. In a randomized placebo-controlled trial, Chang SW et al. (1991), dedicated to assessing the effect of thiazide diuretics on the quality of life in mild hypertension in men aged 35 to 70 years, after 2 months from the start of therapy, patients receiving diuretics reported significantly more sexual dysfunction compared to the control group (including decreased libido, difficulty achieving and maintaining an erection, ejaculation disorders). Statistical analysis showed that ED was not due to hypokalemia or decreased systemic blood pressure.
To date, there are many reports of the occurrence of erectile dysfunction during therapy with β-blockers. At the same time, non-selective β-blockers cause sexual dysfunction to a greater extent than selective ones, this has been proven both experimentally and during clinical observations. For example, in the experiment Smith E. et al. (1990) 30 minutes after a single subcutaneous injection of propranolol and pindolol (but not atenolol) into a male rat, a dose-dependent inhibition of male sexual behavior and ejaculation was observed in the rat. This may be due to the fact that β-adrenergic receptors cause relaxation of the corpora cavernosa (Ferini-Strambi L. et al., 1992), or to the effect of β-blockers on the level of sex hormones (Rosen RC et al., 1988). It is also possible that the influence of non-selective beta-blockers is due to their central effects. This assumption is supported by experimental data according to which the administration of propranolol and pindolol (but not atenolol and metoprolol) directly into the ventricles of the brain was accompanied by suppression of sexual activity in animals (Smith E. et al., 1996). The authors suggest that this effect may be mediated by the interaction of non-selective blockers with β1- and β2-adrenergic receptors or with serotonin receptors in the central nervous system.
According to clinical data (Due DL et al., 1986), propranolol caused sexual dysfunction in 9% of cases. Kostis JB et al. (1990), who conducted a prospective placebo-controlled study, proved that propranolol (as well as clonidine) reliably suppressed spontaneous nocturnal erections. According to Croog SH et al. (1988), in a comparative assessment of the effects of captopril, methyldopa and propranolol on sexual dysfunction during a 24-week treatment period, the highest incidence of sexual dysfunction was observed in the group of patients receiving propranolol.
Similar results were obtained when studying the effect of the cardioselective β-blocker atenolol on male sexuality. During atenolol therapy, spouses of young patients reported significantly lower sexual satisfaction compared to wives of patients receiving nifedipine (Testa MA et al., 1991). Suzuki H. et al. (1988) also reported the occurrence of sexual dysfunction during long-term (for 1 year) therapy with atenolol and noted a moderate decrease in serum testosterone levels. According to Wassertheil-Smoller S. et al. (1991), obtained during the multicenter randomized, placebo-controlled TAIM study, erection-related problems were detected in 11% of patients receiving atenolol for 6 months, which was significantly more often than in the placebo group.
In the era of evidence-based medicine, the TOMHS, a multicenter, double-blind, randomized, placebo-controlled trial that included 557 hypertensive men aged 45–69 years, certainly deserves the most attention. Patients received placebo or one of five drugs (acebutolol, amlodipine, chlorthalidone, doxazosin, or enalapril). Sexual function was assessed by interview with a physician at baseline and then annually during the study. Initially, 14.4% of men reported problems with sexual function; 12.2% of men had problems obtaining and/or maintaining an erection, which were correlated with age, systolic blood pressure and previous antihypertensive therapy. After 24 and 48 months of follow-up, the incidence of ED was 9.5% and 14.7%, respectively, and correlated with the type of antihypertensive therapy. Patients treated with chlorthalidone reported a significantly higher incidence of ED at 24 months compared with the placebo group (17.1% vs. 8.1%, P = 0.025). However, after 48 months, the incidence of ED was almost the same in both groups; the differences in the groups of patients receiving placebo and chlorthalidone were not significant. The lowest incidence of ED was observed when taking doxazosin, but even here no significant differences were obtained from the placebo group. The incidence of ED for acebutolol, amlodipine and enalapril was the same as in the placebo group. In many cases, ED did not require discontinuation of drug therapy. The disappearance of ED in men who initially suffered from it was observed in all groups, but this trend was most pronounced among patients taking doxazosin. Thus, the long-term incidence of ED in treated hypertensive patients is relatively low. ED most often occurs during therapy with chlorthalidone. According to the authors, the similar incidence of ED in the placebo group and with long-term use of the most active antihypertensive drugs allows one to reasonably argue against considering sexual problems in hypertensive men to be a consequence of drug therapy (Grimm et al., 1997).
When choosing antihypertensive therapy, it should also be taken into account that not all β-blockers can negatively affect the sexual function of men. In particular, the side effects of the lipophilic cardioselective beta-blocker bisoprolol were studied in post-marketing studies that included 152,909 patients. Side effects were detected in 11.2% of patients, but only 2.2% of patients needed to discontinue the drug, and no cases of ED were reported at all (Buchner Moll et al., 1995). The absence of a negative effect of bisoprolol on male sexuality is probably due to its high cardioselectivity, which allows the drug to be used in situations where β-blockers are usually contraindicated - with dyslipidemia, diabetes mellitus type 1 and 2, in patients with broncho-obstructive diseases and obliterating diseases of the vessels of the lower extremities. Moreover, it has been shown that the cardioselective β-blocker bisoprolol not only does not worsen the sexual function of men, but even has a beneficial effect on sexual abilities (erectile strength during sexual intercourse, satisfaction with one’s own sexuality - Broekman S. R. et al., 1992).
Due to the widespread use of lipid-lowering drugs in patients with proven coronary artery disease, reports of their inherent side effects have increasingly begun to appear; Moreover, while the effect of fibrates on male sexual function has been known for a long time, the effect of statins is only being studied. Bruckert E. et al. (1996) found that potency disorders were significantly more common among patients receiving lipid-lowering drugs (12% compared to 5.6% in the control group, P = 0.0029). Multivariate analysis showed that ED was dependent on treatment with both fibrate derivatives and statins. A report from the Australian Drug Adverse Events Committee cited 42 cases of erectile dysfunction caused by simvastatin occurring between 48 hours and 27 months after the start of treatment (Boid IW, 1996). In 35 cases, simvastatin was the only drug that patients took; in 4 patients, ED developed again when treatment was resumed. At the same time, as in the case of antihypertensive drugs, these data need careful verification, since, as previously shown, patients with coronary artery disease often develop ED without treatment.
Thus, drug therapy is responsible for every fourth case of ED. The possible effect of a drug on sexual function should be openly discussed with patients, who, in turn, should report any side effects of the drug. When prescribing drug therapy, attention should be paid to the medical history (including the presence of problems in sexual life); if there is an increased risk of developing ED, you should not prescribe drugs that are known to cause it (such as thiazides). When treating arterial hypertension in this situation, preference should be given to calcium antagonists, angiotensin-converting enzyme inhibitors and α-blockers, which have less effect on the sexual sphere (Weiss RJ, 1991), or angiotensin receptor inhibitors, which, apparently, can even slightly increase sexual activity. If it is necessary to prescribe β-blockers (arterial hypertension, coronary artery disease, rhythm disturbances), bisoprolol becomes the drug of choice in patients with an increased risk of developing ED.
A. L. Vertkin, Doctor of Medical Sciences, Professor
The influence of drug therapy on the sexual function of men
| Group of drugs | Libido | Erection | Ejaculation and orgasm |
| α-agonists (clonidine) | — | — | — |
| β-blockers (non-selective) | — | — | — |
| Diuretics (thiazides) | — | — | |
| Cardiac glycosides (digoxin) | — | — | |
| Antihyperlipidemic agents | — | — |
Return
Treatment methods
The disease is treated conservatively or surgically.
If pathology is identified at the initial stage, it is quite possible to get by only with medication and auxiliary procedures. The use of vitamins and a mixture of fatty acids is prescribed. Diet and wearing loose underwear are recommended. If the condition is complicated by prostatitis, anti-inflammatory medications are prescribed.
The operation is a necessary measure aimed at restoring blood supply to the penis to prevent its atrophy. Bypass surgery has the main indication – blocking the lumen of a blood vessel by more than 70%.
High-quality treatment in our clinic will prevent the development of atherosclerosis of the penis and the consequences of pathology. Doctors have informative diagnostic equipment at their disposal. Thanks to him, it is possible to identify a violation even at the initial stage of its development. The operating rooms are equipped with high-quality equipment, which allows the intervention to be performed without subsequent complications.
Indications for the use of ultrasound examination of the vessels of the penis
Ultrasound examination makes it possible to detect a large number of ailments not only in acute form, but also at the development stage. Ultrasound helps the doctor confirm the diagnosis and monitor the effectiveness of the prescribed treatment. Urologists and surgeons refer their patients for examination if there are complaints of discomfort in the genitourinary system and symptoms of penile dysfunction appear.
Indications for this type of ultrasound:
- Injuries and closed injuries of the genital organ.
- Open injuries (animal bites, etc.)
- Peyronie's disease.
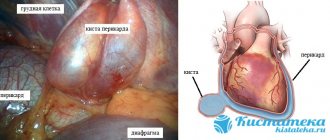
- Presence of neoplasms.
- Pathologies of the vessels of the penis.
- Pain during intercourse.
- Discomfort when urinating.
- Congenital anomalies of the organ.
- Inflammatory diseases of the penis.
In addition, scanning is prescribed for varicocele of the spermatic cord (varicose veins).
It is recommended to undergo an ultrasound scan of the vessels of the penis for preventive purposes; this makes it possible to identify various diseases at the earliest stages, when symptoms have not yet appeared.
Doctors in this field
What is erectile dysfunction
Harmony in sexual relationships among men of any age is an important part of a fulfilling life. Erectile dysfunction is an unpleasant moment that will plunge representatives of the stronger sex into despondency and deprive them of sleep. The statistics are relentless and indicate that the problem of erectile dysfunction has become much younger. Previously, it was mainly men of forty years of age and older who faced the lack of penile erection, but in the modern world, the presence of similar problems is diagnosed in young people. The causes and treatment of “male” dysfunction concern men of different ages. When blood circulation in the penis is impaired, a pathology called erectile dysfunction (ED) occurs. In this case, not only does sexual intercourse become difficult, but the possibility of conceiving a child is often excluded. Lack of erection is often confused with impotence. The presence of erectile dysfunction covers smaller problems than impotence, characterized by decreased libido and the inability to fertilize a woman's egg.
Contraindications
Doppler ultrasound is a painless and safe procedure, so there are no absolute contraindications to it. However, there are still relative contraindications (when it is necessary to postpone the procedure for some time).
Inflammation of the tissues of the penis
The introduction of drugs that stimulate erection can aggravate the existing inflammatory disease and cause severe pain to the patient.
Recent myocardial infarction
Injecting erection-stimulating drugs into the penis can lead to disruption of the blood supply to this organ.
What is examined during ultrasound examination of the vessels of the penis
During an ultrasound scan, the doctor examines the cavernous arteries, blood vessels, as well as the speed of blood inflow and outflow. Indicators must be compared with standards.
Deviations from the norms of ultrasound indicators:
- Echogenicity – decreased may indicate the development of acute cavernitis; increased echogenicity is observed in patients with cavernous fibrosis.
- The structure of the cavernous bodies must be homogeneous. Heterogeneity is characteristic of focal cavernous fibrosis.
- The tunica albuginea of the organ - thickening of the tissue indicates the development of Peyronie's disease.
- echogenicity of the walls of the cavernous arteries is usually observed in patients with diabetic vascular disease.
The diameter of the cavernous arteries is normal 0.2-1.4 mm. Narrowing of the lumen is a sign of autoimmune or atherosclerotic pathology. Diameter expansion is inherent in vascular development anomalies.
Ultrasound diagnostics is carried out so that the doctor can accurately determine the type of vascular disorder of the penis and select effective therapy.
Testing the innervation of the penis
Regardless of the causes of ED, men experiencing erectile dysfunction should definitely visit a doctor. Qualified specialists of CM “Global Clinic” have sufficient experience in this area and will find ways to eliminate the problem. A method of testing the sensitivity of the nerve endings of the penis will help determine the bulbocavernosus reflex. When the doctor presses on the head of the penis with a normal reflex, an instant contraction of the anus should occur. A medical specialist studies this process and draws conclusions about the latency of the reflex.
Symptoms
The presence of erectile dysfunction is indicated by a weakening of the ability to perform full sexual intercourse. This happens in cases where:
- the penis is not hard enough for coitus;
- erection weakens during sexual intercourse;
- it takes a long time for an erection to occur;
- change in sensations during orgasm.
The man does not immediately understand that these changes are associated with the appearance of erectile dysfunction, attributing this phenomenon to fatigue, stress, and general malaise. The roots of the problem may be much deeper. Only qualified doctors, such as those at the Global Clinic Center, can prescribe the correct course of treatment to eliminate this pathology.
Symptoms of vascular impotence
Do not forget that vascular impotence does not go away without symptoms.
Typically, with the development of vascular impotence, the patient experiences the following symptoms:
- problems with erection appear. Typically, patients complain to the doctor of strong arousal, but insufficient erection;
- rapid ejaculation occurs. Moreover, it can occur even before sexual intercourse;
- Night and morning erections completely disappear.
Remember: if one of the above symptoms occurs, a male representative should definitely consult a doctor. Initially, the doctor must conduct a diagnosis.
The patient is prescribed:
- Ultrasound Dopplerography, Dopplerography. During the examination, a special device equipped with a computer is used. The device identifies blocked, narrowed arteries that carry blood to the penis. Moreover, the examination is carried out before and after the introduction of special vasodilating substances into the corpora cavernosa. Remember: if Dopplerography of the vessels of the penis did not reveal any pathologies, the blood flow remained normal after administration of the drug, then the doctor must make sure that there is no venous leakage from the corpora cavernosa. Moreover, young and mature men face this sign of impotence.
- Cavernosography. To identify venous leakage, the patient undergoes an X-ray examination of the penis. Moreover, during the examination, a small screw-shaped needle injects a radiopaque substance into the desired location. After the examination, the patient receives an x-ray. Using it, the doctor examines the condition of the blood vessels and identifies venous leakage. And if a leak has been identified, then a vasodilator drug is injected into the patient’s cavernous bodies. Next, the doctor determines the extent of the surgical intervention and eliminates the leak.
Prevention
To prevent erection problems, it is useful for men to heed the following advice:
- Learn to eat healthy, eliminating unhealthy foods (smoked, canned, salted, alcohol) from your diet. Fruits, vegetables, dairy products, herbs, nuts, and honey should take priority place on the table.
- Say goodbye to unhealthy habits (smoking, alcohol abuse, drugs, sedentary lifestyle).
- Have a regular sex life. Full, uninterrupted intercourse with a regular partner will eliminate many of the problems leading to ED.
- Do not neglect regular visits to the urologist's office. High-level specialists work at the Global Clinic Center; timely consultation will relieve men from problems with erection.
- Monitor your general health.
Manifestations
Symptoms of the initial stage of vascular blockage and the development of vascular impotence are:
- weak unstable erection with strong sexual arousal,
- early ejaculation,
- decreased duration of spontaneous erections at night and in the morning.
Unlike psychogenic, vascular impotence does not occur immediately after a decrease in the lumen of the vessels supplying the penis. Over a long period of time, a man has misfires in bed, to which he does not attach much importance. Then the situation gradually worsens: problems with erectile function arise more and more often. In such cases, it is necessary to consult a urologist-andrologist as soon as possible.
How is ultrasound examination of the vessels of the penis performed?
During the diagnosis, the patient should lie on his back. A conductor gel is applied to the penis; it improves contact of the sensor with the skin. Moving across the skin, the equipment reads data about the structure of the penis and the condition of its arteries. The research results are visualized on the screen.
During the procedure, the doctor can introduce a pharmacological drug (like Vasoprostan or Caverject) through a special tourniquet, which will help cause an erection. If the patient is able to achieve an aroused state of the genital organ in a natural way (viewing magazines or videos of an erotic nature, manual stimulation), then the injection is not given.
In the erect state, signs of deformation of the penis, the level of filling of the cavernous bodies and the strength of blood flow are checked. After the doctor conducts Doppler mapping, the patient can use self-stimulation to get rid of the pharmacological effect; for this, he is left alone in the office. The results of scanning the blood vessels of the penis are given to the patient immediately, and he must go with them to his attending physician.
Service cost*
| NAME | PRICE (Kolomenskaya) | PRICE (Vidnoe) |
| Duplex scanning of the vessels of the scrotum and penis (on the device Voluson, Mindray, Logiq) | 2900 rubles | 2900 rubles |
We accept payment:
*Attention! The indicated prices are provided as reference information and do not constitute a public offer. Check current prices by phone and directly in clinics.