Pain in the heart area: causes
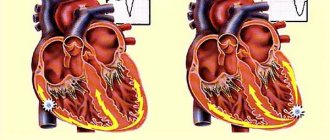
Acute coronary syndrome with pain in the heart area is the most dangerous condition. It occurs when a sudden blockage or narrowing of a coronary artery significantly reduces or completely stops the blood supply to an area of the heart muscle (myocardium). The lack of blood supply to any tissue is called ischemia. If the supply is significantly reduced or stopped for more than a few minutes, the heart tissue dies. This is how a heart attack, or myocardial infarction (MI), develops. This is the death (necrosis) of a certain area of cardiac tissue due to ischemia.
A blood clot (or thrombus) is the most common cause of blockage of a coronary artery. Typically, the artery is already partially narrowed due to the accumulation of cholesterol and other fatty materials in the artery wall (atheroma or plaque). It may crumble or rupture, releasing substances that make platelets stickier, which encourages clot formation. In about two-thirds of people, the blood clot dissolves on its own, usually within 1-2 days. However, by this time, damage to small areas of the heart has usually occurred.
In rare cases, a heart attack occurs when a clot forms in the heart itself, breaks off, and becomes lodged in a coronary artery. Another uncommon cause is a coronary artery spasm that stops blood flow. Cramps can be caused by stress, taking certain medications, smoking, or alcohol. Sometimes the exact cause of pain in the heart area cannot be determined.
Types of pain in the heart area
Depending on the specific cause, the patient is bothered by pain in the heart area of various types. They can be isolated, but are more often accompanied by other symptoms that also need to be paid attention to. Based on the type of pain and its location, duration and accompanying complaints, one or another pathology can be suspected.
- Acute coronary syndrome occurs as a result of sudden blockage of a coronary artery (or its branch). This blockage causes unstable angina or the development of myocardial infarction, depending on the location and extent of the blockage. People with acute coronary syndrome usually experience pressure or sharp chest pain, shortness of breath, and fatigue.
- Aortic dissection. Over time, uncontrolled high blood pressure can weaken the wall of the heart's main artery (aorta). It will thin until it eventually ruptures, causing aortic dissection, which is a medical emergency. Aortic dissection usually causes sudden, severe, sharp pain in the chest, neck, throat, or jaw and often a feeling of pressure in the chest that radiates backwards.
- Heart valve damage. The heart has four chambers. The upper and lower chambers are connected by valves with gates that open and close to allow blood to flow in only one direction. If the valves are affected, the flaps become hardened, fused, or leak and do not function properly. The consequences of these valve problems can cause chest pain in the heart area.
- Myocarditis and pericarditis. Chest pain can also be caused by irritation and swelling of the heart (myocarditis) or its outer lining (pericarditis). Inflammation can be caused by infection or as a consequence of a heart attack or heart surgery. Pain from myocarditis or pericarditis is usually sharp, burning and localized in the center of the chest, in the sternum. Typical pain in the heart area when inhaling, against a background of coughing, or when moving. Sometimes it decreases if the patient sits or leans forward.
- Hypertrophic cardiomyopathy (HCM). This is a thickening of part of the heart. When a person has this condition, the heart has to work harder to pump blood in and out of the heart, which can cause dull or aching pain in the chest. They can intensify with stress.
Symptoms of CVD
Cardiovascular diseases are numerous, have different origins and mechanisms of development. The main causes of cardiac pathologies are infectious and inflammatory processes, congenital developmental defects, damaging environmental factors (intoxication, hypothermia), metabolic disorders, and autoimmune reactions.
A peculiarity of the development of cardiovascular diseases is that they can occur hidden for a long time. Early signs of CVD, such as unmotivated weakness, fatigue, heaviness in the legs at the end of the working day, discomfort and discomfort in the chest, are not considered by people as symptoms of the disease that are worth paying attention to. Poor sleep, nausea not associated with food intake, clammy sweat, exercise intolerance, and headaches may indicate the appearance of heart problems.
Common cardiovascular diseases include:
- Atherosclerosis.
- Hypertonic disease.
- Cardiac ischemia.
- Inflammatory heart diseases.
- Violations of excitability and automatism of the myocardium.
- Heart defects.
Other causes of chest pain
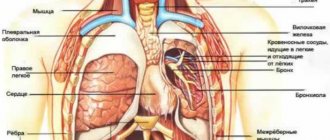
Pain in the heart area at rest is possible, which is of extracardiac origin, but simulates cardiac pathology. These may be problems with the lungs (thromboembolism of the branches of the pulmonary artery, pneumonia, cancer) or damage to the intercostal muscles, costal cartilages (costochondritis), osteochondrosis. Then there will be pain in the ribs, especially when breathing deeply, aching or stabbing pain, malaise or weakness. With thromboembolism, breathing problems, severe shortness of breath, increasing dizziness, and a feeling of lack of air occur.
It is not easy to recognize these pathologies, therefore, if any pain appears in the chest area, especially in the left shoulder blade, in the chest area, above the heart area, you should immediately call an ambulance or consult a doctor.
Symptoms for which you need to call an ambulance
The manifestations of different types of acute coronary syndrome are similar, and it is often impossible to distinguish between angina and heart attack based on symptoms alone.
The symptoms of angina are quite typical. People usually experience an attack of pressing, squeezing pain under the shoulder blade or behind the sternum. People often interpret this sensation as discomfort or heaviness rather than pain. Discomfort may also occur in the shoulder or on the inside of either arm, spreading through the back into the throat, jaw or teeth. However, in people with unstable angina the picture changes. Attacks of pain occur more frequently or more severely, or attacks occur at rest or after light physical activity. About two out of three people who have a heart attack experience unstable angina, shortness of breath or fatigue in the days or weeks before. This change in chest pain patterns can lead to a heart attack.
With a heart attack, the most recognizable symptom is usually pain in the middle of the chest, which may spread to the back, jaw, or left arm. Less commonly, the pain spreads to the right arm. The pain of a heart attack is similar to that of angina, but is usually more severe, lasts longer, and is not relieved by rest or nitroglycerin. Less commonly, the pain is felt in the abdomen, where it may be mistaken for indigestion, especially because burping may provide partial or temporary relief.
For unknown reasons, women often experience atypical symptoms that are less likely to be accurately diagnosed as a heart problem. About a third of people who have had a heart attack do not experience chest pain. Typically these include women, people over 75, those with heart failure or diabetes, and those who have had a stroke.
Other symptoms of an attack include feeling lightheaded or faint, sudden heavy sweating, nausea, shortness of breath, and fast heartbeat (tachycardia).
During a heart attack, a person may become restless, anxious, sweat profusely, and may experience a feeling of impending doom. Lips, hands or feet may turn slightly blue. During the first hours of a heart attack, a heart murmur and abnormal heart sounds can be heard with a stethoscope.
Case from practice
A woman came to the appointment with complaints that her heart was aching and pain was radiating to her back. She had a history of small focal infarction. Currently, the unpleasant sensations continue for two weeks, they subside and resume. Deterioration occurs after physical activity and changes in body position. Nitroglycerin and Validol do not help. No abnormalities were found on the ECG; the study was carried out at the height of the attack. X-ray and CT scan of the thoracic region revealed the initial stages of a hernia in 3-4 vertebrae. Prescribed: Movalis, Dolobene-gel, electrophoresis with Novocaine. A week later, the condition returned to normal; a complex of exercise therapy and massage were recommended.
How is diagnosis carried out in patients who often experience heart pain?
An ECG is the most important initial diagnostic procedure for frequent chest pain. Abnormalities detected by an ECG help doctors determine the type of treatment needed. Abnormalities on the ECG also help determine where the heart muscle has been damaged. If several ECGs recorded over a period of several hours are completely normal, doctors consider a heart attack unlikely.
Measuring levels of certain substances (called cardiac markers) in the blood also helps doctors diagnose abnormalities. These substances are usually found in the heart muscle, but only enter the bloodstream when it is damaged or dead. The most commonly measured are heart muscle proteins called troponin I and troponin T, and an enzyme called creatine kinase. Blood levels rise within 6 hours of a heart attack and remain elevated for several days. Levels of cardiac markers are usually measured upon admission to the hospital and at 6 to 12 hour intervals over the next 24 hours.
When ECG and cardiac markers do not provide sufficient information, echocardiography can be performed. It may show decreased mobility of part of the left ventricular wall. This suggests damage due to a heart attack. Other tests are used to determine whether a person needs additional treatment or is likely to have heart problems. For example, a person may have to wear a Holter monitor, which records the heart's electrical activity over a 24-hour period. This procedure allows doctors to determine whether a person has an abnormal heart rhythm (arrhythmia) or episodes of poor blood flow without symptoms (silent ischemia).
An exercise test (electrocardiography done during exercise) before or shortly after discharge can help determine how well a person is doing after the attack and whether ischemia continues.
During an exercise tolerance test (stress test), a person walks on a treadmill at an accelerating pace. A blood pressure cuff monitors your blood pressure throughout the procedure. The video monitor displays the pulse and ECG. The results help determine the presence of coronary heart disease.
How to help a patient
When a person’s heart aches, you can help him in the following way:
- give a tablet of “Nitroglycerin”, “Corvalol”, “Validol”;
- lay down or sit in a comfortable position;
- open access to air (if the attack occurred indoors);
- release from constricting parts of clothing;
- if anxiety is expressed, take a sedative (Persen, Phenibut);
- call a doctor.
When the ambulance arrives, you should describe in detail your sensations, the reasons for their occurrence and list the medications taken.