It is necessary to register for pregnancy, as this allows for timely diagnosis of:
- Pathologies of fetal development;
- Chronic diseases in the mother that can affect the course and outcome of pregnancy;
- Acute pathologies in the mother that occur during pregnancy, affecting the growth and development of the fetus and the health of the mother.
Pregnancy is a complex restructuring of the body; diseases in the mother are not always known if the examination is not completed before conception.
What happens to the body during the 1st trimester of pregnancy
The 1st trimester is considered from the moment of conception to 12 weeks of pregnancy.
Direct fertilization of the egg occurs in the abdominal cavity. After fertilization, the egg is located in the abdominal cavity and is actively fragmented into smaller cells and becomes similar to a raspberry or mulberry, such an embryo is called a morula. It is then captured by the villi of the fallopian tubes and moves into the uterine cavity. On the 7th day, the embryo attaches to the wall of the uterus. The fertilized egg begins to form, consisting of amniotic fluid and the yolk sac, from which the embryo will form. At 7-8 weeks, a fertilized sac and placenta are formed from the fertilized egg. From 8 to 12 weeks the placenta is finally formed (later on it only develops), it becomes visible on ultrasound. At week 12, the embryo looks like a full-fledged child measuring about 9 cm, its limbs, head and main internal organs are formed.
Mother's changes. Ideally, a woman does not feel pregnancy at all. The only sign is an enlargement of the mammary glands, due to the development of glandular tissue under the influence of hormones. The belly practically does not increase.
During pregnancy, many women experience so-called “toxicosis” - nausea and/or vomiting. This is due to an increase in the level of estrogen (in particular progesterone) and hCG (chronic gonadotropin). Moreover, these symptoms can complicate the life of a pregnant woman not only in the morning, but at any time of the day. Sometimes nausea or vomiting may persist throughout pregnancy.
There is such a serious complication as excessive (uncontrollable) vomiting in pregnant women, which leads to dehydration of the mother, disruption of the body's electrolyte balance, disruption of the liver and kidneys and encephalopathy, requiring hospitalization and treatment in a hospital.
It is best to eat according to your appetite. Food should not cause negative reactions, eat in small portions, pay attention to what food provokes nausea and try not to eat it for a while, listen to your body, usually the woman herself feels what she would like to eat. Don't forget that food should not only be desirable and tasty, but also healthy. It would be ideal to eat according to the “Harvard Healthy Eating Plate” method, when ½ of the plate’s volume is occupied by vegetables, ¼ by proteins (including plant-based), ¼ by complex carbohydrates (grains, potatoes, cereals, etc.).
Your body will also begin to change. And the first thing you will feel will be engorgement and increased sensitivity of the mammary glands, the nipples will swell a little and increase in size. It is important to wear comfortable, comfortable underwear and clothing to minimize discomfort. Sometimes there is pain in the nipples; your gynecologist may recommend ointments for this case.
We all remember that a pregnant woman becomes more vulnerable, whiny and even sometimes capricious. This is also associated with an increase in estrogen levels and requires patience and understanding on the part of family and partners. A calm environment at home and, if possible, at work is important. You can use relaxation methods such as walking, listening to your favorite music, aromatherapy if there are no reactions to odors. Think about what could bring back balance and calm to you?
The main pregnancy hormone, progesterone, causes fluid retention in the body. At the same time, the growing uterus puts pressure on the bladder and a frequent urge to urinate appears. This is normal, it is important to plan your day so that you always have the opportunity to visit the toilet.
Progesterone also reduces the tone of blood vessels, which can lead to dizziness. You can minimize these unpleasant sensations by changing your body position smoothly; do not stand up or sit down abruptly. Another reason for frequent dizziness may be a decrease in the level of magnesium in the blood; your doctor will help you figure this out.
Pregnant women often have an increased need for sleep, which is explained by the same effect of hormones, as well as the need for additional rest for the body, because there is a lot of work to carry, give birth and then feed the baby.
Under the influence of progesterone, the smooth muscles of the entire body relax (uterus, intestines, blood vessels, bile ducts and pancreatic ducts, etc.), the work of internal organs slows down, which in turn leads to constipation and heartburn. In addition to medication correction (prescribed by a doctor), split meals in small portions, foods rich in fiber (our favorite vegetables), sufficient fluid intake, feasible physical activity (physical therapy, walking, swimming, yoga, Pilates, etc.) help.
Unfortunately, sometimes pregnancy is overshadowed by pathology; let's talk about the most common problems in the first trimester of pregnancy.
With severe COVID-19 in pregnant women, the number of thromboembolic complications increases significantly. This is due, on the one hand, to physiological changes in the hemostasis system towards hypercoagulation - a gradual, as the duration of pregnancy increases, an increase in the plasma level of fibrinogen, factors VII, von Willibrand, VIII, and the concentration of D-dimers; antithrombin III decreases slightly, fibrinolytic activity decreases.
On the other hand, SARS-CoV-2 infection also causes a number of pathophysiological reactions that significantly affect the hemostatic system. Thrombosis in patients with COVID-19 is triggered mainly by the extrinsic pathway of activation of the blood coagulation process (through the combination of tissue factor with factor VII).
Olga Svetlitskaya, Associate Professor of the Department of Anesthesiology and Reanimatology of BelMAPO, Candidate of Medical Sciences. Sciences. Damage to the alveolar-capillary barrier
The SARS-CoV-2 virus penetrates the lung tissue by binding to the ACE2 receptor, which is expressed in large quantities on the surface of type 2 pneumocytes and endothelial cells lining the capillary bed.
From the moment the virus enters and begins replication, the cell ceases to perform its inherent functions, begins to produce proteins characteristic of the virus, with the formation of new virions, and then is destroyed. Alveolar macrophages and monocytes circulating in the capillary bed of the lung tissue react to this. They begin to produce large quantities of interleukins IL-1, IL-6 and other pro-inflammatory cytokines.
The more virions multiply, the more type 2 pneumocytes and endothelial cells are destroyed, and the more serious the disruption of the alveolar-capillary barrier, which is clinically manifested by a decrease in saturation. The increase in the production of proinflammatory cytokines by macrophages and monocytes significantly affects the activation of the hemostatic system.
The interleukins produced, in particular IL-1 and IL-6, increase the synthesis of tissue factor on the surface of endothelial cells that are not yet damaged by SARS-CoV-2. In addition, IL-6 blocks the synthesis of tissue factor pathway inhibitor. The accumulation of tissue factor globally activates the process of blood coagulation throughout the vascular bed.
Massive platelet aggregation begins in the lumen of the pulmonary capillaries and the formation of clots. The narrower the lumen of the vessel, the less likely the formation of full-fledged blood clots in it; platelet sludge is more often observed in them. TNF-a (tumor necrosis factor alpha) blocks fibrinolysis.
Thus, with COVID-19, just as with septic conditions, two serious pathophysiological processes occur in parallel in the hemostatic system: global activation of thrombus formation against the background of suppression of fibrinolysis.
Difficulties of anticoagulant therapy for COVID-19
All patients, including pregnant women, should receive prophylactic and therapeutic doses of LMWH calculated for their actual body weight.
It is unacceptable to select the dose of heparin by eye, because this can lead to complications. All patients with COVID-10 upon admission should be weighed at the ED level and weight and height clearly recorded in the medical record.
What to do if it is not possible to determine the level of D-dimers?
Firstly, we must remember that the study of D-dimer levels, which is widely practiced among the general population of patients with COVID-19, in pregnant women has low clinical significance, since the spread of D-dimer levels in normal pregnancy is significant and has not yet been achieved establish reliable reference values for D-dimers during pregnancy. Therefore, the assessment of the level of D-dimers must be carried out in dynamics, paying attention not only to the absolute level, but also to the daily increase.
In situations where for some reason it is not possible to urgently determine the level of D-dimers, the level of LDH (lactate dehydrogenase) should be assessed. A dynamic increase in LDH, especially >1,000 U/L, in a patient with COVID-19 may be an indirect laboratory sign of pulmonary embolism and/or pulmonary infarction. This test is highly sensitive, but non-specific, however, since with COVID-19 the affected area is primarily the lungs, we can assume that the disaster occurs there.
Indirectly confirm the presence of PE: ECG (signs of overload of the right parts of the heart), ultrasound of the heart (expansion of the right parts, increase in the average value of PAP) and veins of the lower extremities (presence of blood clots).
The listed indirect signs allow one to suspect PE or a high risk of PE and promptly prescribe adequate doses of heparins.
What to do if you cannot reach your target RAPTT level?
First of all, you should check the correctness of the nomogram (calculation and correction of the bolus and the administered dose of unfractionated heparin to the actual body weight). If you are sure that you did everything correctly, but the RAPTT still did not reach the target values, determine the levels of antithrombin III and/or anti-Xa activity.
Antithrombin III (AT III) and what to do if it decreases
Heparin is a cofactor of AT III; it transforms AT III into an immediate-acting anticoagulant, enhancing its effects 1,000 times or more depending on the dose and speed at which it is administered. AT III deficiency reduces the ability of heparin to inhibit coagulation factors IIa and Xa.
The average normal AT III level is 80–120%. In pregnant women, it naturally gradually decreases and by the end of the 3rd trimester normally should not decrease to less than 65%. Practice shows that 60–65% is a completely manageable situation. Lower rates (55–50% and below) should alert a specialist.
In acute inflammation, the level of AT III always increases, but with the development of thrombosis, sepsis, disseminated intravascular coagulation syndrome, and the administration of heparins, it decreases. Therefore, a decrease in AT III levels in a patient with COVID-19 is a poor prognostic sign that indicates the development of serious complications and requires action.
In case of AT III deficiency, the decision is made individually.
There are three approaches for coagulation correction of AT III level:
1.Transfer of the patient to therapeutic doses of LMWH. In conditions of AT III deficiency, we focus on factor Xa binding, given the fact that the binding of 1 unit of Xa prevents the formation of 50 units of IIa (thrombin).
2. AT III replenishment with fresh frozen plasma (FFP) or AT III concentrate. Both options are not recommended for COVID-19. Transfusion of FFP in the setting of ARDS increases the risk of further lung damage due to the possible development of TRALI syndrome (acute injury to the lung parenchyma in response to transfusion of blood and its components). The administration of AT III concentrate (in cases where its level has not decreased less than 65%) can lead to increased bleeding, which is undesirable when treating pregnant women in critical condition.
3. Transfer of patients to direct thrombin inhibitors (independent of AT III) - direct factor IIa inhibitor (dabigatran) or direct factor Xa inhibitor (rivaroxaban). This method is used in the general group of patients and is not used in pregnant women.
Determination of Anti-Xa activity (IU/ml)
Currently, the ability to determine anti-Xa activity has appeared in many hospitals, and it is important to be able to correctly interpret the results ( see Table 1 for recommended levels ).
Blood sampling for this study is carried out 3–4 hours after subcutaneous administration of LMWH. It is best to do this after 4 hours, since it is at this time interval that the maximum level of concentration of administered LMWH in the blood plasma (anti-Xa activity) is observed.
Table 1. Classic recommended levels of anti-Xa activity Taking into account the fact that hospitalization of patients with covid pneumonia is generally associated with a high risk of pulmonary embolism, the level of anti-Xa activity should be maintained within the range of 0.5–1.0 IU/ml.
The principle of dose adjustment of LMWH based on anti-Xa activity is given in Table. 2 .
Table 2. Dose adjustment of LMWH for therapeutic concentrations of 0.5–1.0 IU/ml
What to do if D-dimer levels do not decrease?
One of the most frequently asked questions: we are doing everything correctly, but the level of D-dimers was and remains high. Hospitals fall into this trap when laboratories give a D-dimer response of “greater than some value,” for example, “>5,000 ng/ml.”
In this case, you need to contact the laboratory and, if possible, clarify the actual level of D-dimers at the time the patient was admitted to intensive care. It is quite possible that it was 7,000, 10,000 or even 20,000 ng/ml and is slowly decreasing with treatment.
Also, to correctly assess the situation, you should perform: monitoring the level of AT III and/or anti-Xa activity; Ultrasound of the heart with calculation of mean PAP; Ultrasound of the veins of the lower extremities (looking for blood clots).
As UFH is titrated, the blood clots gradually loosen and disintegrate, maintaining an elevated level of D-dimers. Therefore, if a pregnant woman has thrombosis of the veins of the lower extremities, it is necessary to periodically repeat an ultrasound and check the length of the blood clot. If it decreases, then everything is fine.
We must not forget that sometimes the source of elevated levels of D-dimers can be a hematoma that slowly goes away, sometimes over several weeks.
What should I do if my D-dimer levels start to rise again?
In a situation of sudden growth, it is necessary to carry out diagnostic measures:
- control of thrombus formation: ultrasound of the vessels of the lower extremities, ultrasound of the heart (dilation of the right cavities of the heart + average value of PAP);
- monitoring the severity of the inflammatory syndrome (the most accessible way is to determine C-reactive protein (CRP)).
An increase in the level of CRP over time indicates the acute phase of inflammation. Under the influence of IL-1, IL-6 and TNF-a, the synthesis of CRP increases after 6 hours, reaching its maximum concentration after 24–48 hours.
If during treatment there is a sharp rise in the level of D-dimers, in parallel the level of CRP begins to increase, correlating with an increase in the level of LDH, this indicates the fact of a catastrophe in the pulmonary vessels.
How to understand whether there is a pulmonary embolism in the absence of CT angiography?
An increased level of D-dimers by itself in this situation does not confirm PE, but the dynamics of this indicator is important. Clinical signs of pulmonary embolism should be assessed, in particular perfusion respiratory failure (decreased peripheral saturation <90%, compensatory tachypnea, tachycardia, hypotension, etc.).
Apply instrumental research methods available at this level of medical care: perform an ECG (overload of the right chambers of the heart), ultrasound of the heart (dilatation of the right chambers), measure the average value of PAP (with PE it can reach 35–60 or more mm Hg) , Ultrasound of the veins of the lower extremities (looking for blood clots).
What to do if the patient “bleeds” or a hematoma appears, and D-dimers are elevated?
In case of active bleeding, it is necessary to stop the administration of UFH and restore normocoagulation. If necessary, compensate for the deficiency of blood coagulation factors by transfusion of single-group fresh frozen plasma or a concentrate of prothrombin complex factors.
Further return to heparins is possible only if normocoagulation is achieved in the screening coagulogram and there are no signs of active bleeding.
The dosage of LMWH is determined individually, taking into account the cause of bleeding (diffuse bleeding, postoperative bleeding, etc.), platelet levels, dynamics and reasons for the increase in D-dimer levels.
read the material “COVID-19: features of the course and treatment in pregnant women” by following the link here.
The most common problems in the 1st trimester of pregnancy
Bleeding : due to a lack of progesterone, spasm and relaxation of the muscles of the uterus occurs and, accordingly, detachment of the ovum and bleeding (in severe cases, miscarriage). Also, with hypothyroidism, there is a violation of the implantation of the fertilized egg, which also leads to bleeding.
Thrombosis . During pregnancy, blood clotting increases (this is normal - the body is preparing for blood loss). To prevent thrombosis of the veins of the lower extremities, it is necessary to stop taking oral contraceptives 6 months before planning a pregnancy, and during pregnancy, maintain sufficient physical activity (long walks, swimming) and be observed by a doctor. If pain, swelling, or “cyanosis” occurs in the lower extremities, you should immediately consult a doctor.
Developmental anomalies and genetic pathologies . In the 1st trimester, abnormalities in the development of the fetus most often develop and manifest themselves, which can occur as a result of ionizing radiation, infectious diseases suffered during pregnancy (rubella, influenza, etc.), taking drugs prohibited during pregnancy (fluoroquinolones, macrolides, tetracyclines, tranquilizers , etc.), genetic pathologies and hereditary diseases.
Anemia . More often it happens due to iron deficiency, because. the fetus consumes a huge amount of it, taking away iron reserves from the mother, less often due to bleeding. B12 and folate deficiency anemia also occur, which is also associated with increased consumption and insufficient consumption by the mother. Anemia is dangerous due to chronic lack of oxygen, causing fetal growth restriction syndrome. In severe cases, it can lead to intrauterine fetal death.
Chronic diseases may worsen during pregnancy . This is due to the fact that the fertilized egg already carries part of the DNA that is foreign to the mother. To prevent egg rejection, the mother’s body suppresses its immunity throughout pregnancy, which affects the body as a whole. Therefore, all diseases that were not detected at the stage of preparation for pregnancy should be detected and treated. This applies mainly to infectious diseases. For example, exacerbation of chronic pyelonephritis, or herpes virus infection.
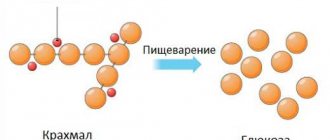
Also, during pregnancy there is a sharp restructuring of hormonal levels , which, in turn, affects somatic (non-infectious) diseases. For example, due to thickening of bile and compression of the gallbladder by the uterus, chronic cholecystitis may worsen. As the fetus develops, the islets of Langerhans (cells that produce insulin in the pancreas) sometimes do not develop quickly enough and the baby begins to consume the mother's insulin. If the mother has diabetes or impaired glucose tolerance (including hidden), both the child and the mother lack insulin, which leads to tissue damage to both the child and the mother (early aging of the placenta, delayed fetal development, premature birth, polyhydramnios, increased blood pressure in a pregnant woman, the formation of a large fetus, the risk of injury to the woman and child during childbirth and the most dangerous complication - intrauterine fetal death).
In addition, the fetal liver does not yet function as a detoxification organ, and all decay products produced by the child are forced to be processed by the mother’s liver. 2% of pregnant women develop benign cholestatic hepatosis of pregnancy - a violation of the formation and outflow of bile, which causes:
- Itchy skin, especially at night
- Digestive disorders (as bile is involved in the emulsification of fats)
- Inflammation of liver tissue due to toxic effects on cells and bile ducts