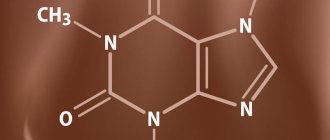
Atropine (anatropine) - what is it? Atropine is an m-anticholinergic blocker (pharmacological group), a dangerous plant alkaloid and tropine ester. The medicine atropine looks like a white powder without a distinct odor, quickly dissolves in liquids, including alcohol and water. This substance is a poison for the human body; it is naturally found in nightshades: belladonna (belladonna), datura, henbane . Atropine sulfate formula: C17H23NO3.
Atropine - indications for use
The drug is available both as a solution for intravenous administration (atropine sulfate) and in tablet form; in addition, there are also eye drops.
What is atropine used for medical purposes? Previously, it was used to treat psychosis using atropine coma; today this technique is not used in medicine. Medicines containing atropine (anticholinergics) are used for the treatment of asthma, gastrointestinal tract in gastroenterology, as well as in ophthalmology, psychiatry, pulmonology, cardiology, premedication in surgery, urology, toxicology, poisoning with organophosphorus compounds, etc. However, the drug has quite a lot of contraindications and side effects, it should not be used by those who are allergic to atropine (Atropinum Sulfuricum D5), as well as by glaucoma, liver disease, heart disease (arrhythmia, tachycardia), increased intraocular pressure, etc.
Today, a medicine called atropine and atropine-containing drugs are quite often used by drug addicts for recreational purposes not related to medical indications, to obtain a “high” and a euphoric effect. In the article you will learn everything about atropine, its action and the consequences of non-medical use.
How does atropine affect the human body?
The side effects of atropine are quite extensive, ranging from dizziness to hallucinations. Among the consequences of consuming atropine, one can identify worsening diseases of the cardiovascular system, inflammatory processes on the mucous membrane of the eyeballs (eye drops), rapid heartbeat, and lack of oxygen to the brain. If the drug is beneficial in therapeutic doses, then if used inappropriately it can lead not only to severe intoxication of the body, but also to death.
The effect of atropine on the body:
- stimulation of the central nervous system;
- hallucinations;
- psychosis;
- psychomotor agitation;
- pupil dilation;
- blockage of secretory glands;
- stomach contractions decrease;
- heartbeats increase.
After taking atropine orally, the effects occur within 30 minutes, and when administered intravenously, within a few seconds.
Atropine
special instructions
Use with caution in patients with diseases of the cardiovascular system, in which an increase in heart rate may be undesirable: atrial fibrillation, tachycardia, chronic heart failure, coronary artery disease, mitral stenosis, arterial hypertension, acute bleeding; with thyrotoxicosis (possible increased tachycardia); at elevated temperatures (may further increase due to suppression of the activity of the sweat glands); with reflux esophagitis, hiatal hernia, combined with reflux esophagitis (decreased motility of the esophagus and stomach and relaxation of the lower esophageal sphincter can slow down gastric emptying and increase gastroesophageal reflux through the sphincter with impaired function); for gastrointestinal diseases accompanied by obstruction - achalasia of the esophagus, pyloric stenosis (possibly decreased motility and tone, leading to obstruction and retention of gastric contents), intestinal atony in elderly or debilitated patients (possible development of obstruction), paralytic ileus; with an increase in intraocular pressure - closed-angle (mydriatic effect, leading to an increase in intraocular pressure, can cause an acute attack) and open-angle glaucoma (mydriatic effect can cause a slight increase in intraocular pressure; adjustment of therapy may be required); with nonspecific ulcerative colitis (high doses can inhibit intestinal motility, increasing the likelihood of paralytic intestinal obstruction, in addition, the manifestation or exacerbation of such a severe complication as toxic megacolon is possible); with dry mouth (long-term use may cause further increase in the severity of xerostomia); with liver failure (decreased metabolism) and renal failure (risk of side effects due to decreased excretion); for chronic lung diseases, especially in young children and weakened patients (a decrease in bronchial secretion can lead to thickening of secretions and the formation of plugs in the bronchi); with myasthenia gravis (the condition may worsen due to inhibition of the action of acetylcholine); prostatic hypertrophy without urinary tract obstruction, urinary retention or predisposition to it, or diseases accompanied by urinary tract obstruction (including bladder neck due to prostatic hypertrophy); with gestosis (possibly increased arterial hypertension); brain damage in children, cerebral palsy, Down's disease (reaction to anticholinergic drugs increases).
The interval between doses of atropine and antacids containing aluminum or calcium carbonate should be at least 1 hour.
With subconjunctival or parabulbar administration of atropine, the patient must be given a validol tablet under the tongue in order to reduce tachycardia.
Impact on the ability to drive vehicles and machinery
During the treatment period, the patient must be careful when driving vehicles and engaging in other potentially hazardous activities that require increased concentration, speed of psychomotor reactions and good vision.
Narcotic effect of atropine
The body's response varies greatly depending on the dose consumed. When using a small dose of the substance, a surge of strength and energy occurs, and mood improves. Taking an average dose leads to stress relief and relaxation; an overdose of the drug is fraught not only with poisoning and hallucinations, but also with death. The narcotic effect of atropine is explained by the accumulation of acetylcholine in the synoptic cleft, inhibition of parasympathetic effects and the functioning of the nervous system.
If the permissible daily dosage is exceeded, a person feels warm and relaxed, relaxed, euphoric and slightly dizzy. The narcotic effect of atropine can be compared to the use of marijuana and other cannabinoids containing THC. How a drug affects a person depends on his mood and state of mind before use. If the mood is negative, the substance will only intensify the reaction, which can lead to panic attacks and depression.
Euphoria after a few hours is replaced by the opposite effect: drowsiness, lethargy, weakness, emptiness, weakness. A person has problems with the gastrointestinal tract and a headache. The higher the dose of atropine, the stronger the symptoms of intoxication, the person begins to behave inappropriately, and psychosis occurs due to the effect of the drug on the central nervous system. They are accompanied by mydriasis, insomnia, tachycardia, pressure surges, and behavioral and mental abnormalities. This condition can last about 24 hours.
Treatment of bradycardia
The selection of therapy depends on the reasons that led to this condition. If bradycardia occurs while taking medications, the doctor will recommend stopping or replacing medications that reduce heart rate.
If the cause relates to extracardiac factors, the cardiologist may schedule a consultation with a related specialist who is responsible for the treatment of the pathology that caused the bradycardia.
In some cases, for strict medical reasons, a surgical operation is prescribed, during which a pacemaker is installed.
The emergence of addiction and its treatment
In pursuit of new unusual sensations and euphoria, as well as an attempt to get away from problems, people turn their attention to pharmaceutical drugs. This is exactly the effect that atropine gives: fogginess of consciousness, withdrawal from reality, artificial elevation of mood. Not all people know about the dangers of atropine and the consequences of its regular and excessive use. Even a person who has been prescribed a drug by doctors can become addicted to the drug. Having felt the effect of the drug, a person may become psychologically dependent on its effect.
If a drug helps an addict cope with depression, stress, internal problems and complexes, he will use it again and again, which will lead to addiction. However, no chemical substance can be used for a long time without consequences for the body. The longer the period of use, the more the addict degrades both physically and mentally. As a result of acquiring drug addiction, people only have more problems, they grow like a snowball and do not allow a person to get out of the vicious circle. Only doctors at the Favorit drug treatment clinic in Rostov-on-Don can save a person from imminent death.
The development of addiction is also influenced by the fact that a person stops receiving pleasure in the usual way: from delicious food, walks with friends, a favorite activity, communication with loved ones. The only source of pleasure, euphoria and pleasure is atropine. Soon the addict begins to realize that the usual dose no longer gives the desired effect, so he gradually increases the dosage and also begins to use other pharmaceutical drugs or psychotropic substances. step by step a person loses himself as an individual and becomes one step closer to death.
Causes of bradycardia
Neurogenic bradycardia
The main role in the development of a slow heartbeat is played by a disorder of the nervous system. It can be expressed in various pathological conditions: neuroses, vagoinsular crises, bleeding in the brain, inflammatory diseases of various brain structures. Among the causes of neurogenic bradycardia are renal, hepatic, and intestinal colic. Hernias and ulcers of the gastrointestinal tract can contribute to rhythm disturbances
Ischemic bradycardia
Ischemic bradycardia is influenced by a number of influencing factors. By taking them into account, you can reduce the risk of developing coronary artery disease, and with it, bradycardia. First of all, cardiologists pay attention to biological indicators (age, gender, hereditary predisposition). Behavioral characteristics play a role, in particular, nutrition, bad habits, and an inactive lifestyle. If necessary, anatomical, metabolic and physiological characteristics are analyzed.
Extracardiac bradycardia
Extracardiac bradycardia can be a consequence of traumatic lesions, which are accompanied by severe blood loss. Severe inflammation and infectious effects are also often accompanied by a slowdown in heart rate. If the thyroid gland does not function sufficiently (hypothyroidism), then bradycardia is one of the symptoms of the development of pathology.
Vagal bradycardia
Vagal bradycardia can develop for other reasons, more related to the internal state of the body. First of all, this is the aging process, nervous system disorders, and infectious diseases. Also, tumor processes, myxedema, and excess potassium in the blood affect cardiac activity. Some drugs - 23-24 (antihypertensive and vasodilators), if taken incorrectly, can also cause rhythm disturbances.
Hyperkalemia and bradycardia
A slow heartbeat primarily occurs with hyperkalemia (excess potassium in the blood). This condition is associated with several reasons. First of all, this is a violation of the excretion of potassium from the body, which is often observed with nephropathies, systemic lupus erythematosus, adrenal and kidney failure. Hyperkalemia in combination with bradycardia can develop with increased transition of a microelement from the plasma of cells into the intercellular fluid, and from there into the blood. This often develops with extensive injuries, burns, and ischemic tissue damage. Also, rhythm disturbances can occur against the background of a lack of insulin production and with the development of intracellular acidosis.
Drug-induced bradycardia
There are drugs that, if taken incorrectly, cause a slowdown in cardiac activity. In particularly severe cases, cardiac arrest may occur. Such drugs primarily include cardiac glycosides, which most often cause drug-induced bradycardia and emergency visits for patients who have taken these drugs incorrectly. Other such medications are potassium-containing medications. They are often used to eliminate tachycardia, while forgetting that excess potassium in the body negatively affects cardiac activity.
Drug-induced bradycardia can develop while taking muscle relaxants. They are often used to relax muscles, but if used incorrectly, the heart can stop. Anti-heartburn medications are also not as safe as they initially seem. Their prolonged use or incorrectly selected dose can cause quite pronounced bradycardia. However, the medicine can be passed through breast milk, so it is extremely important for nursing mothers not to take medications for heartburn.
Phases of poisoning
Regardless of whether a person took a large dose of the drug accidentally or intentionally, he will invariably experience severe intoxication. Atropine poisoning leads to the appearance of corresponding symptoms within 10-20 minutes after consumption. A person begins to feel dry mouth and eyes, his temperature rises, and skin hyperemia occurs. There are several phases of poisoning.
Psychomotor agitation
Atropine intoxication leads to various kinds of disorders of the central nervous system, including due to dry eyes, a person’s vision decreases and deteriorates, dizziness, muscle hypertonicity, tendon reflexes, confusion, increased sensitivity to light, mydriasis, convulsions, psychosis occur. . A person addicted to a psychoactive substance begins to behave inappropriately: laugh, cry, perform strange actions, run. He may experience visual, tactile or auditory hallucinations, and mental disorders with predominant psychomotor agitation occur.
CNS depression
Disruption of the nervous system begins in a person within 7-10 hours from the moment of consuming atropine in an increased dosage. The victim feels weakness or twitching in the muscles, his thoughts are confused, he cannot formulate a sentence. The danger of the drug is that its excessive use can lead to coma.
When taking a large dose of the drug, the symptoms of depression of the nervous system are very obvious, and there may not even be psychomotor agitation. Feeling the desire to sleep, a person falls asleep, but the drug causes disruption of the heart, blood vessels and respiratory system, which can cause death in sleep. Asphyxia, respiratory arrest, heart failure, and pulmonary or cerebral edema may occur due to breathing problems.
Treatment of bradycardia. When does the heart need help?
Bradycardia is a slowing of the heart rate. Normally, an adult's heart rate is 65-80 beats per minute. In children, this figure is higher, the younger the child. A newborn's normal heart rate can be 140 beats.
Risk factors, what happens
In accordance with the generally accepted classification, there is no division of bradycardia. However, there is a conditional division that allows you to assess the severity of the violation.
Depending on the severity of the symptom, bradycardia is divided into:
- Light. It is said to occur when the heart rate is more than 50 beats/min and there is no discomfort in the patient. Treatment for bradycardia is not required.
- Moderate. The contraction frequency is in the range of 40-50 beats. In some cases, it may be a variant of the norm, for example, in athletes. Signs of oxygen starvation may occur.
- Severe bradycardia. A significant decrease in heart rate (below 40 beats/min) is accompanied by multiple disorders.
Causes
Bradycardia can be caused by a number of reasons.
Pathological causes that pose a danger are the following:
- increased tone of the parasympathetic nervous system;
- intoxication;
- hypothyroidism;
- a number of infections;
- heart diseases.
8
24/7
The appearance of bradycardia while taking medications is common and usually not dangerous. However, if this symptom occurs regularly, it is recommended to consult your doctor. Perhaps he will adjust the dosage or replace the drug.
The use of the following medications often leads to a slowdown in heart rate:
- Quinidine;
- Digitalis;
- Amisulpride;
- Adenosine;
- glycosides;
- beta blockers;
- calcium channel blockers;
- morphine
As a rule, bradycardia occurs due to an overdose of these medications.
Increased tone of the parasympathetic nervous system is also dangerous by slowing the heart rate. It can develop against the background of:
- neuroses;
- depression;
- TBI;
- increased intracranial pressure;
- cerebral hemorrhage;
- cancerous tumors in the mediastinum;
- stomach or duodenal ulcer.
Intoxication can develop not only due to medications, but also due to the effects of other substances on the body. Toxins can damage various organs and systems. This cause is determined quite simply, since in addition to bradycardia, intoxication is accompanied by many more symptoms.
Intoxication with substances such as:
- lead and lead compounds;
- organophosphorus substances;
- nicotine;
- some drugs.
Thyroid pathologies are another reason why your heart rate may slow down. A decrease in thyroid hormones leads to bradycardia, while an increase in their level leads to tachycardia.
Hypothyroidism is a hormone deficiency that occurs due to diseases of the gland itself or due to a lack of iodine.
Infectious diseases that provoke a decrease in heart rate:
- typhoid fever;
- sepsis;
- some forms of hepatitis.
It can also develop against the background of almost any infection in its protracted stage, when the body does not have the strength to fight the disease.
Cardiac pathologies are a logical reason why rhythm disturbances can be observed. The most dangerous processes in this case are sclerotization and inflammation that have spread to the conductive tissue. When this tissue is damaged, the impulse is delayed and cannot pass normally.
Symptoms
With mild bradycardia, no additional symptoms occur. Severe bradycardia significantly affects blood flow and is accompanied by the following symptoms:
- dizziness;
- fainting;
- dyspnea;
- general weakness;
- paleness of the skin;
- increased fatigue;
- chest pain.
Diagnostics
Before starting treatment for bradycardia, a diagnosis must be made. Detecting bradycardia is not difficult and can be done by a person independently by measuring the pulse on the radial or carotid artery.
However, confirmation from a specialist is still required, since pulse and heart rate do not always coincide.
8
24/7
To confirm the diagnosis the following can be used:
- auscultation;
- electrocardiography.
Auscultation is performed by a doctor during the initial examination. The procedure involves listening to tones and noises using a stethoscope. The advantage of the method is the ability to evaluate the functioning of the heart valves, which allows one to suspect certain heart diseases.
Electrocardiography is a method for studying the bioelectric impulse. The differences from the cardiogram of a healthy person will be in the longer distance between the teeth.
Treatment
Treatment of bradycardia is carried out only when it is pathological and is aimed at the reason for which it developed.
The patient should not make his own decision about taking medications, since they are not always necessary.
Drug treatment of arrhythmia during bradycardia should be carried out in the following cases:
- the presence of dizziness, fainting and symptoms indicating circulatory disorders;
- decreased blood pressure;
- frequent attacks of slow heart rate, accompanied by a feeling of discomfort;
- the presence of chronic diseases that act as a provocateur of bradycardia;
- heart rate drops below 40 beats/min.
In these cases, treatment of bradycardia is necessary, since it is important to normalize blood circulation and prevent the development of complications. Hospitalization is required only for those patients who have serious concomitant pathologies.
Most often, only drug treatment for bradycardia is used to eliminate symptoms.
Bradycardia is treated with medication using the following medications:
- Atropine. A drug from the category of anticholinergics. It prevents overexcitation of the parasympathetic nervous system. While taking it, the tone of the vagus nerve decreases and the heart rate increases. It is administered by injection subcutaneously or intravenously.
- Analogs of adrenaline. Isoprenaline, Izadrine (intravenously), Isoprenaline (orally), Izadrine (sublingual tablets). The drugs act on special receptors in the myocardium, increasing the tone of the sympathetic nervous system and stimulating the heart rate.
- Eufillin. The drug is a bronchodilator drug, but has a good effect on bradycardia. It improves the transport of oxygen to tissues and accelerates heart rate. It is administered intravenously.
In cases where bradycardia is a consequence of another disease, medications are prescribed to eliminate the underlying cause.
Treatment of bradycardia in hypertension is carried out using the following medications:
- Prazoline;
- Terazosin;
- Artesin.
Surgical intervention
Treatment methods for bradycardia are not limited to taking medications. Surgical treatment of cardiac bradycardia is performed extremely rarely - only in cases where the deviation significantly affects hemodynamics. As a rule, in the presence of congenital anomalies, the operation is performed in childhood.
Surgery is also indicated in cases where cancerous tumors affect the mediastinum area.
For persistent bradycardia leading to heart failure due to an unknown cause, implantation of a pacemaker is indicated. This is a special device that creates electrical impulses.
Forecast
If sinus bradycardia is not treated, the following consequences may develop:
- heart failure;
- thrombus formation;
- transition of bradycardia to a chronic form.
Heart failure is an extremely rare complication of bradycardia. It can occur with a strong decrease in heart rate. The pathology is accompanied by disruption of the left ventricle, in which it cannot supply a sufficient volume of blood to the tissues and maintain pressure at the required level. Against this background, the risk of ischemia and heart attack develops. It is important to control the level of physical activity, since increased load requires greater oxygen consumption by the myocardium.
The formation of blood clots occurs when heart blockades and slow heartbeat with rhythm disturbances occur. Blood is pumped slowly and a small volume of it is not pushed out of the ventricle, but stagnates. This is where clots form. The likelihood of this increases with prolonged or frequently recurring attacks.
The resulting blood clots can penetrate any vessel and lead to blockage. This increases the risk of serious complications such as heart attack and stroke. Confirmation of blood clot formation is carried out using echocardiography. It requires specific treatment for bradycardia. Surgery may also be performed to prevent congestion in the ventricle.
Chronic attacks of bradycardia are most often the result of physiological causes, so drug treatment will be ineffective.
Prevention
First of all, bad habits should be eliminated. One of the most dangerous is smoking. Constant poisoning of the body with nicotine has a negative effect on the functioning of the myocardium and the entire circulatory system.
Permitted physical activity should be discussed with your doctor.
Meals should be organized taking into account the following principles:
- limiting the consumption of fatty meat (especially pork);
- refusal of alcoholic drinks;
- control of water and salt consumption;
- inclusion of nuts and foods rich in fatty acids in the diet.
Some patients think that bradycardia is not such a terrible symptom and no measures can be taken. However, such a positive attitude is not always justified. To make sure that your life is safe, you need to contact a specialist. Only he can confirm the absence of dangerous diseases.
8
24/7
Treatment of intoxication
How to cope with poisoning? How is acute atropine intoxication treated? First of all, you need to call the Favorit RC and call the emergency drug treatment service to your home. Doctors will arrive within 30-40 years. However, quite often victims require pre-medical assistance; you can get detailed advice from professionals by calling our clinic’s hotline absolutely free. The patient will also need emergency medical care and then hospital treatment.
How to remove poison from the body without harming the health of the addicted person? First of all, doctors carry out a detoxification procedure. To cleanse the body of toxins as quickly as possible, droppers with adsorbents and a number of medications are used to speed up metabolism and normalize the patient’s general condition. In addition, depending on the degree of intoxication, the following measures are used: gastric lavage (potassium permanganate), induction of vomiting, use of laxatives and diuretics, hemosorption.
Next comes the turn of symptomatic treatment and elimination of physiological disorders in the addict’s health. The drugs are used according to indications and contraindications. In case of severe clinical picture and breathing problems, tracheal intubation and artificial ventilation are used, resuscitation measures include installation of a catheter and administration of the necessary medications intravenously.
In case of atropine poisoning, the victim must be given an antidote: Physiostigmine, Aminostigmine, Nivalin or Galantamine in an individual dosage. These drugs help to quickly get rid of the unpleasant consequences of intoxication and symptoms such as hallucinations.
Use by drug addicts
Recreational use of atropine has recently begun to increase.
Today it is quite easy to find a prescription or an illegal drug on the Internet and social networks. Pharmacy drugs are among the cheapest and most accessible, despite the ban and criminal prosecution for distribution without a doctor's prescription. Most often, people who are addicted to atropine are those who have already used or are using narcotic substances. Drug addicts can combine the drug with alcohol, other pharmaceutical drugs, tranquilizers, psychostimulants, opiates, etc. The use of several chemical substances in order to obtain a euphoric effect is called polydrug addiction.
Dual addiction is quite difficult to cure. It is worth noting that it is impossible to get rid of this kind of drug addiction on your own at home. It is necessary to contact a specialized drug treatment clinic. Our rehabilitation center in Rostov-on-Don provides assistance to all drug addicts and their loved ones, regardless of their length of use.
Systematic, regular use of atropine in high dosages leads to serious health consequences for addicts. This is not only a disruption of the central nervous system and depression of cognitive functions, and, accordingly, a person’s intellectual abilities, but also the development of heart and vascular diseases, and disruption of the respiratory system. The addict has problems with communication and socialization. Physical and mental dependence lead to the emergence and development of severe withdrawal symptoms.
Mechanism of action of atropine
The drug blocks M-receptors and nerve impulses. Atropine binds to areas of the brain instead of acetylcholine, as a result of which various abnormalities occur in the human body, including inhibition of impulses from the central nervous system and suppression of the secretion of sweat, salivary and a number of other glands. As a result, the smooth muscles of the intestines, gastrointestinal tract and bladder relax and expand. Atropine causes paralysis of accommodation and mydriasis, farsightedness, increased heart rate, bradycardia, and vasodilation.
Overdose and poisoning
Atropine, depending on the form of release, can be used orally, intravenously, in the form of eye drops, intramuscularly and subcutaneously. The therapeutic dose of the drug when taken orally is 0.25-1 mg (no more than 3 times a day). The dosage depends on the individual characteristics of the human body. For intravenous and intramuscular administration, the dose is identical. If your doctor has prescribed you drops to dilate the pupil, you should not take them in excess of the prescribed dose, a maximum of 2 drops 2 times a day. Even if a person does not intend to obtain a narcotic effect, if the dose is exceeded, an overdose can occur. In addition, atropine is found in the fruits of plants from the nightshade family, which can also easily be poisoned.
Symptoms of atropine overdose
- dilated pupils;
- lack of reaction to light;
- nausea, vomiting;
- tremor of the limbs;
- thirst, dry mouth;
- difficulty urinating;
- headache;
- dizziness;
- rapid pulse;
- accelerated heartbeat;
- high blood pressure;
- cramps, spasms;
- constipation.
Atropine overdose can occur not only when the dose is increased, but also when combined with other chemicals and toxins, including alcohol. As soon as you notice the first signs of intoxication and poisoning, you should call the Favorit RC in Rostov-on-Don. Doctors at our center have the opportunity to come to the patient’s home and carry out all the necessary resuscitation measures, as well as pre-consult relatives about emergency care.
Within 30-40 minutes, the toxic effect of atropine occurs, which can last for several days. Toxins spread throughout the body, poisoning it and accumulating in the tissues of internal organs. A pharmaceutical drug can linger in the body of an addicted person for quite a long time. This is why a person becomes lethargic, weakened, painful, irritable, and loses interest in others. The drug removes all useful substances and vitamins from the body, reducing the addict’s immunity. A person begins to have problems with teeth, hair, nails, and skin.
There are 3 degrees of atropine poisoning: mild, moderate and severe. If at the first stage a person can still cope with the symptoms on his own at home, then in the case of moderate poisoning it is worth calling an ambulance at home. If you do not contact the clinic in time, atropine will begin its harmful effects and destructive effects on the human heart, liver, kidneys, blood vessels and central nervous system. Frequent symptoms of atropine intoxication: hallucinations, psychosis, loss of coordination, abnormalities of the nervous system.
If an addict regularly uses atropine to obtain a euphoric effect, the consequences of taking it can be much sadder and more dangerous: paralysis of the respiratory muscles, coma, death. While in a coma, a person is at risk of impaired cognitive functions and intellectual abilities, and mental abnormalities. It is not difficult to calculate the lethal dose of atropine; it is 1.5 mg per 1 kg of body weight of an adult. Death from abuse and overdose occurs within 5 hours after use.
Drugs used for bradycardia and heart block
Home Medical encyclopedia Medicines Cardiovascular medicines
ATROPINE SULPHATE (Atropinisulfas)
Synonyms: Atropine, Atropine sulfate.
An alkaloid contained in various plants of the nightshade family (Solanaceae): belladonna (Atropa Belladonna L.), henbane (Hyoscyamusniger L.), various types of datura (Daturastramonium L.), etc.
Pharmachologic effect. Atropine is a non-selective M-cholinergic receptor blocker. The effects of atropine are opposite to those observed when the parasympathetic nerves (including the vagus) are excited.
Indications for use. For bradycardia (slow pulse) that develops as a result of increased tone of the vagus nerve and an overdose of beta-blockers and calcium antagonists.
Method of administration and dose. For blockade of vagal origin (caused by increased activity of the vagus nerve), 1 ml of a 0.1% solution is administered intravenously. Atropine in a similar dose is also used for blockade caused by propranolol or verapamil.
Side effect. When using atropine, care should be taken in dosage and the possibility of increased individual sensitivity of patients should be taken into account. A slight overdose can cause dry mouth, dilated pupils, impaired accommodation (impaired visual perception), tachycardia (rapid heartbeat), difficulty urinating, atony (loss of tone) of the intestines, dizziness.
Contraindications. Atropine is contraindicated in glaucoma (increased intraocular pressure).
Release form. 0.1% solution in ampoules of 1 ml.
Storage conditions. List A. In a place protected from light.
ISADRIN (Isadrinum)
Synonyms: Isoprenaline hydrochloride, Isoproterenol, Isuprel, Novodrin, Euspiran, Aleudrin, Aludrin, Antasmin, Bronchodilatin, Izodrenal, Isonorin, Isopropylarterenol, Isorenin, Neodrenal, Neoepinephrine, Norizodrine.
Pharmachologic effect. The pharmacological and therapeutic effect of isadrin is explained by its stimulating effect on beta-adrenergic receptors. The action of isadrin extends simultaneously to 6era- and beta2-adrenergic receptors, so the effect on the bronchi, cardiovascular system and other organs equipped with beta-adrenergic receptors is not selective.
During heart blocks, the effect of isadrin is associated with an improvement in conductivity due to its effect on the sympathetic innervation of the heart, with an increase in the excitability and contractile function of the myocardium (heart muscle). A similar effect is exerted by various sympathomimetic substances, including norepinephrine, adrenaline, ephedrine; however, these drugs cause increased blood pressure, angina pain (pain in the heart), increased excitability of ectopic foci (displaced rhythm sources) and other side effects, which limits the possibility of their widespread use in atrioventricular block (impaired conduction of excitation through the conduction system of the heart). Izadrin
more convenient for this purpose, since it does not increase blood pressure and is less capable of causing ventricular fibrillation (chaotic contractions of the heart muscle).
Indications for use. Isadrin is used in the treatment of patients with atrioventricular conduction disorders, to relieve atrioventricular block and prevent attacks in Adams-Stokes-Morgagni syndrome (loss of consciousness with a sharp drop in pressure due to certain heart rhythm disturbances).
Isadrin is also used in some forms of cardiogenic shock (normovolemic /without changes in circulating blood volume/, with reduced output and high peripheral resistance).
Method of administration and dose. Administered intravenously in a 5% glucose solution at a dose of 0.5-5 mcg (0.0005-0.005 mg) per minute.
Side effect. When using isadrin (especially in cardiological practice), it should be taken into account that it causes tachycardia (rapid heartbeat), can activate ectopic foci, cause extrasystoles (heart rhythm disturbances) with the risk of ventricular fibrillation. You should also consider the possibility of nausea and tremor (shaking) of the hands. dry mouth. Caution should be exercised when prescribing to patients with angina pectoris and thyrotoxicosis (thyroid disease).
Contraindications.
Release form. 0.5% and 1% solutions in bottles of 25 and 100 ml; tablets containing 0.005 g of the drug.
Storage conditions. List B. In a dry, cool place, protected from light.
Ipratropium bromide
Synonyms: Atrovent, Atrovent nasal. Arutropid, Vagos, Itrop, Normosecretol.
Pharmachologic effect. M-anticholinergic agent. Causes a pronounced and prolonged increase in heart rate. Dilates the bronchi, reduces the secretion of glands. Unlike atropine, it does not affect the central nervous system. The maximum concentration of the drug is determined in the patient’s blood plasma 2-5 hours after administration.
Indications for use. Sinus bradycardia (rare pulse), mainly caused by the influence of the vagus nerve, bradyarrhythmias (rare irregular contractions of the heart) with sino-auricular block (impaired conduction of excitation through the conduction system of the heart), atrioventricular block of the second degree according to Wenckebach (impaired conduction of excitation through the conduction system of the heart ) and bradysystolic form of atrial fibrillation (a type of heart rhythm disorder).
Method of administration and dose. The dose of the drug is selected individually. Treatment begins with a single administration of the contents of 1 ampoule of ipratropium bromide intravenously or with taking '/2-1'/2 tablets of the drug. When taken orally (by mouth), the drug is usually prescribed 1-1'/2 tablets 2-3 times a day.
Side effect. Dry mouth, loss of appetite, constipation, impaired accommodation (impaired visual perception), increased intraocular pressure, impaired urination, decreased secretion of sweat glands, extrasystole (heart rhythm disturbances).
Contraindications. Glaucoma (increased intraocular pressure), hypertrophy (increase in volume) of the prostate gland, mechanical stenosis (narrowing) in the gastrointestinal tract, tachycardia (rapid heartbeat), megacolon (enlargement of the upper part of the large intestine), first trimester of pregnancy.
Release form. Tablets of 0.01 g in a package of 50 pieces; injection solution 1 ml in ampoules in a package of 5 pieces.
ORCIPRENALINE SULPHATE (Orciprcnalinisulfas)
Synonyms: Alupent, Astmopent, Alotek, Astor, Dosalupent, Metaproterenol sulfate, Novasmazol.
Pharmachologic effect. Its chemical structure and pharmacological properties are similar to isadrin. The drug is a mixed type beta-adrenergic receptor stimulant, acting on beta- and beta-adrenergic receptors. Facilitates atrioventricular conduction (conduction of excitation through the conduction system of the heart).
Indications for use. Atrioventricular conduction disorders.
Method of administration and dose. In case of atrioventricular block (impaired conduction of excitation through the conduction system of the heart), the drug is used with caution, injecting 0.5-1 ml of a 0.05% solution slowly intravenously, or intramuscularly, or 1-2 ml subcutaneously. If necessary, administer the drug by slow intravenous infusion. For infusion, the contents of 1-2 ampoules of 10 ml of 0.05% solution (total 5-10 mg) are diluted in 250 ml of 5% glucose solution or isotonic sodium chloride solution and administered at a rate of 10-20 drops per minute.
To prevent attacks with Adams-Stokes-Morgagni syndrome (loss of consciousness with a sharp drop in pressure due to certain heart rhythm disturbances), with absolute bradyarrhythmia (very rare and irregular heartbeats) and with intoxication (poisoning) with digitalis drugs, digitalis is prescribed orally at a dose of '/2- 1 tablet (adults) 6-10 times a day, changing the dose and frequency of doses depending on the heart rhythm.
Side effect. Orciprenaline is usually better tolerated than isadrin, but its use may cause side effects similar to those with
Neniya Izadrina. When administered intravenously, a decrease in blood pressure is possible.
Contraindications. Severe atherosclerosis.
Release form. 0.05% solution in ampoules of 1 and 10 ml (0.5 and 5 mg); tablets 0.02 g.
Storage conditions. List B. In a dry place.
EPHEDRINE HYDROCHLORIDE (Ephedrinihydrochloridum)
Synonyms: Ephedrine hydrochloride, Efalon, Ephedrozan, NeoPhedrin, Sanedrin, Efetonin, etc.
An alkaloid found in various types of ephedra (EphedraL.), fam. ephedraaceae (Ephedraceae), including Ephedraequisetina (equisetum ephedra), growing in the mountainous regions of Central Asia and Western Siberia, EphedramonospermaS.AM, growing in Transbaikalia, etc.
Pharmachologic effect. Ephedrine stimulates alpha and beta adrenergic receptors.
In terms of its peripheral sympathomimetic effect, ephedrine is close to adrenaline. Causes vasoconstriction, increased blood pressure, dilation of the bronchi, inhibition of intestinal peristalsis (wave-like movements), dilation of the pupils, increased blood glucose levels. Facilitates atrioventricular conduction (conduction of excitation through the conduction system of the heart).
Indications for use. Atrioventricular conduction disorders.
Method of administration and dose. Used in cases where the use of atropine, isadrine and orciprenaline sulfate is contraindicated, at a dose of 30-50 mg every 4-6 hours, but the effect is rarely achieved. To avoid disruption of nighttime sleep, ephedrine should not be prescribed at the end of the day or before bedtime.
Side effect. The drug is usually well tolerated. Sometimes, 15-30 minutes after ingestion, slight trembling is observed, which quickly passes.
Contraindications. The drug is contraindicated in atherosclerosis, organic heart disease, hyperthyroidism (thyroid disease).
Release form. Powder; tablets 0.025 mg; tablets 0.002; 0.003 and 0.001 g; 5% solution for injection in ampoules of 1 ml; 2% and 3% solutions in 10 ml bottles.'
Storage conditions. List B. Powder - in a well-closed container, protected from light; tablets, ampoules and solutions - in a place protected from light.
| print version | This information is not a guide to self-treatment. A doctor's consultation is required. |
Treatment of atropine addiction in Rostov-on-Don
Treatment of atropine addiction, as well as addiction to any pharmaceutical drugs, takes place in a drug rehabilitation center in Rostov-on-Don. Therapy includes detoxification and symptomatic treatment, as well as rehabilitation, which stabilizes the addict’s condition and consolidates the treatment results. Doctors help patients eliminate psychological cravings for psychoactive substances through group and individual sessions. During the treatment process, various psychotherapeutic and medicinal techniques are used, as well as psychocorrection and family therapy, especially necessary for adolescents. The last step in the treatment of drug addiction is resocialization and adaptation to society.