home
/
Articles
/
How to place an IV at home for a patient with “bad” veins?
An IV is considered a simple medical procedure, but requires certain knowledge and experience. It is strictly not recommended to carry out the procedure of intravenous infusions on your own due to the high risk of complications.
To install an IV at home with the help of a nurse, you don’t need a lot of money: a specialist will do everything professionally, in compliance with the rules. True, it is not always possible to avoid difficulties during infusion, especially if the patient has inconspicuous, thin and fragile veins that are not easy to reach.
Content
- Why are IVs placed in the veins in the arms?
- What is poor venous access?
- Causes of “bad” veins in the arms
- 5 proven ways to find a vein Physical activity
- Squeezing
- Warming
- Gravity
- Fluid replacement
- Tools and accessories
Why are IVs placed in the veins in the arms?
It is no coincidence that the veins in the arms are chosen for medical procedures, since they have the most suitable structure for this. On the upper limbs there are deep and superficial vessels. The latter lie close to the surface of the skin, making it easy to draw blood from them.
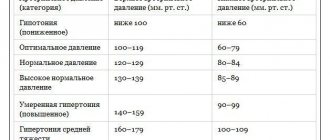
The pressure in them is only 5-10 mmHg (in the arteries in the arms it can be 139 mm), the venous wall contains a small number of muscle cells, is pliable and stretches well. In addition, the skin on the hands is much thinner than on the feet, so it can be pierced without causing severe pain to the person.
After a puncture, a small scar appears on the wall of the vein - the same as after damage to the skin in any other place. It can persist for a long time - months and even years. The integrity of damaged venous walls is never completely restored, but changes (if there are not too many of them) do not have a significant impact on the functioning of the body.
What to do if veins appear on the legs?
The answer to this question is clear and simple: contact a phlebologist. Only a doctor who treats veins can conduct a detailed examination, correctly assess the patient’s condition and prescribe treatment, the main task of which is to remove the affected veins.
The most gentle treatment option for the patient is sclerotherapy - a non-surgical method that involves injecting a special sclerosant into the lumen of the vein, which leads to the closure of the vessel. The same result is achieved by the use of radiofrequency and laser therapy; in some cases, surgical intervention is necessary. The optimal method of treatment is always chosen by the doctor depending on the initial condition of the patient.
Phlebology Center specialists often answer patients’ questions related to the fact that veins protrude on the legs. We list the most frequently asked questions here:
What is poor venous access?
The situation when a nurse cannot get into a vein is familiar to about a third of patients who have received intravenous injections or an IV at home or in a hospital setting at least once in their lives. The reason is not always the inexperience of the medical worker. Sometimes even specialists with extensive experience do not get to the right place the first time - most often this happens when venous access is difficult.
Normally, the veins should protrude slightly above the skin between the muscles and have a bluish or blue tint. But for some people, they are too thin or almost invisible, making it difficult to insert the needle. In nursing practice, there are cases when a vein is difficult not only to see, but also to palpate. Then experienced specialists use proven methods to find a vein and place an IV in the place where this is easiest to do.
Improving access to the vein
The key to a correct injection is the accessibility of the vein and its visibility. Many improve access to it incorrectly, this is due to conflicting information from dubious sources. Experienced doctors advise focusing on 5 methods.
Lots of liquid
Give the person water (at least 250 ml) one hour before you give the medicine. Why is this necessary? For two reasons:
- The amount of water in the body directly affects how quickly blood is pumped through the veins. And this speed affects how noticeable they are.
- If you are dehydrated, it is quite difficult to find a vein, especially for a layman.
The following method will help you get closer to the desired result.
Causes of “bad” veins in the arms
Inconspicuous, thin or fragile veins are a serious problem for those who perform medical procedures. There can be several reasons for this phenomenon, ranging from natural causes to taking medications and frequent injections:
- Features of the body. The pattern and location of the veins are individual for each person, therefore they are the same unique biometric characteristic as a fingerprint or iris pattern. Accordingly, “hidden” vessels may be a feature of the body.
- Genetic predisposition. The strength of venous valves is genetically determined. According to statistics, if both parents suffer from varicose veins, the probability of their children inheriting it is about 80%. The same goes for fragile or thin veins - they are often a family problem.
- Aging. Venous access worsens with age - this is due to a decrease in elastin and collagen content, as well as thinning of subcutaneous fat. The skin becomes thin, “papery”, and the veins become thin and fragile, which increases the risk of injury and bleeding.
- Excess weight. In people with a high BMI (body mass index), the veins are hidden under fat. With obesity, it is difficult to perform not only intravenous injections and drips, but also some diagnostic procedures - ultrasound, MRI.
- Frequent injections. Any injection represents an injury, and if there were too many of them, scars form in place of healthy tissue. The veins “hide” and harden, so it becomes more difficult to place an IV or give an injection.
- Regular drug administration. In addition to frequent injuries, venous access in drug addicts deteriorates due to the administration of caustic, aggressive drugs. They literally burn the venous walls, making it extremely difficult for long-time drug addicts to carry out medical procedures.
- Exposure to ultraviolet radiation. Ultraviolet rays can also destroy elastin and collagen, which is why venous access is often difficult in people who are frequently exposed to the sun.
- Taking medications. Some drugs worsen the condition of the veins and increase the risk of complications during catheterization. Corticosteroids cause atrophy of the epidermis, and anticoagulants increase the risk of bleeding.
Poor venous access may be a transient phenomenon. If a person is stressed (for example, afraid of injections) or is cold, finding a vein to place an IV can be difficult.
“The veins on my arms are very visible. Veins especially swell on the hands after physical activity. It doesn’t look very nice, even if you don’t take off your gloves! But I’m only 36 years old. Please give me some advice on what can be done about this?” Natalia, Vladivostok
Every woman wants to have beautiful, well-groomed hands. After all, you can easily tell by your hands (as well as by your face) how old you are. With age, many women begin to develop a pronounced venous pattern on their hands, especially on the back of the hands. This is explained by various physiological changes in the body. But why do veins sometimes appear on the arms of young women? What is this connected with? What is this - a disease or just a cosmetic defect? And what to do with such an “artistic” drawing?
Let's look at the main reasons why vein veins begin to appear on the hands of some women.
The first reason is the physiological characteristics of the body
- Hereditary features of skin structure
Thus, veins can be noticeable on the arms of thin people with thin skin. They shine through the thin top layer and become visible on the surface of the brush. This is often due to genetic features of the structure of the skin: if your mother has noticeable veins on her arms, then you will most likely have this feature.
- Natural skin aging process
As you know, with age, the skin becomes thinner and loses its elasticity. This is due to the fact that there are no sebaceous glands on the hands. Over the years, thinning of the subcutaneous adipose tissue is observed. That is, the fat layer in which the veins were previously hidden becomes thinner, and the veins protrude outward. If the veins do not hurt, then there is no reason to worry.
- Veins may appear on the skin in hot weather.
From the heat, blood vessels begin to dilate, blood circulates faster, and veins begin to swell.
The second reason is physical activity.
Veins on the hands can also appear from physical activity: from lifting weights, carrying heavy bags, working in the garden, cleaning the house, etc. Physical activity on the hands worsens the nutrition of the subcutaneous fat layer, because of this the veins swell and become visible on the hands.
The third reason is varicose veins or varicose veins.
As we know, venous blood circulates upward. Our hands are almost always down. If the walls of blood vessels are weak, blood circulation is disrupted, stagnation occurs, veins swell and begin to appear under the skin. As the disease progresses, swelling and pain appear along the veins. Although varicose veins on the arms are much less common than varicose veins on the legs, such cases are still known. Therefore, if the veins in your arms cause pain, you should consult a phlebologist to rule out varicose veins. As you can see, most often bulging veins on the arms of women are still a cosmetic defect, and not some kind of disease. Therefore, it is not necessary to resort to radical measures to remove veins on the arms that are very visible. But this can and must be fought!
How to remove bulging veins on the arms?
The best way is to prevent them from appearing. Therefore, starting from the age of 30, it is important not only to systematically care for your hands, not forgetting about their hydration and nutrition, but also to perform simple prevention:
- Do not wear tight, constricting clothing, so as not to impair the flow of blood through the venous vessels;
- Avoid excessive physical stress on the shoulder girdle, neither carrying nor lifting heavy objects;
- Take a contrast shower, it perfectly tones the walls of blood vessels;
- Eat more vegetables and fruits: they contain essential vitamins, and some help thin the blood.
- Perform finger exercises
These exercises can be performed anywhere - in public transport, in queues, just walking down the street, etc.
Make circular movements with your fingers, much like we do “Magpie-Crow” for little children. Spread your fingers out to the sides. Walk your fingers along the surface of the table. To improve blood circulation, perform simple hand exercises daily (read below “A set of hand exercises”). These exercises help prevent the appearance of veins or remove small veins that have already appeared on the arms. If the cause of the appearance of bulging veins is varicose veins, then phlebologists recommend wearing a compression sleeve or hand glove for therapeutic purposes. Wearing such a glove or sleeve helps stop the expansion of veins and avoid swelling. There is no need to constantly wear the product; it is advisable to use the sleeve during physical activity - during training, when working in the garden, when carrying heavy loads.
Enlarged veins spoil the appearance of your hands. Whatever this happens, love your hands, take care of them, and then no “artistic patterns” will spoil the beauty of your hands and your mood
Oksana Pustovalova, chiropractor
A set of exercises for hands:
- Cross your arms at the back of your head. Slowly turn the body in both directions. Do 20 reps.
- Stretch your arms forward, clench your fists. Unclench your palms, spreading your fingers wide. Do 20 reps.
- Squeeze your left wrist with your right palm. Raise your left hand as high as possible, while resisting with your right hand. Repeat 20 times. After this, raise your arms up and fix them in this position for 20 seconds. Repeat the exercise for the second hand.
- Raise your arms above your head, clench and unclench your fists. Do 80 reps. Put your hands down and do the same.
- Raise your arms above your head. Breathe evenly and deeply. After this, vibrate with your hands for 3 minutes. Slowly lower your arms.
These exercises help improve the condition of your hands - they become smooth, and the veins on your hands are not so visible.
How to properly place an IV: procedure algorithm
In order to administer an intravenous infusion, appropriate knowledge, experience and strict adherence to technique are required. Correct placement of a drip is not only about inserting a needle without consequences for the patient, but also about choosing a system, infusion rate, etc.
Tools and accessories
To carry out the infusion, it is necessary to prepare the medications prescribed by the doctor (check the expiration date, volume and other important indicators), as well as instruments and consumables:
- Dropper stand. It is a portable stand with hooks onto which containers with solutions are placed. Its height is 1.5-2 m, which provides sufficient pressure for insertion.
- Infusion system. Droppers differ in the diameter of needles, tubes and the speed of infusion of drugs. It is very important to decide on the size of the needle, which is inversely proportional to the number: twenty-second is the thinnest, fourteen is the thickest. It depends on the anatomical features of the patient and the characteristics of the drug.
- Related accessories. In addition to a tripod and a system for placing an IV, you will need a tourniquet (it helps to find the vein), a patch to fix the needle and cotton wool.
In addition to the prescribed medications, you need to prepare an antiseptic liquid. Most often, alcohol is used; if a person has allergies, they take alcohol-free solutions (for example, Chlorhexidine).
Preparation for the procedure
Before manipulations, be sure to wash your hands and wipe them with an antiseptic. Failure to comply with hygiene rules can lead to infection and sepsis, even if the health worker has perfect infusion technique.
- Connect the system to the container or package with the drug. To do this, you need to wipe the needle with alcohol and pierce the cork - this is not difficult, since they are made of soft rubber or other materials.
- Hang the containers on the racks and secure them well. Be sure to check that there is no air in the system - fill the tubes and drip chamber about a third with liquid. Small bubbles are usually not dangerous - they will stick to the walls of the container and will not enter the bloodstream.
If sterility is violated at one of the stages, infusion is strictly prohibited. This can lead to blood poisoning and other dangerous consequences.
Placement of the IV
Before the procedure, it is necessary to familiarize the patient with the features of its implementation. Each drug has a special effect on the body, and some sensations may frighten a person. It is important to distinguish the side effects of drugs from the alarming symptoms that develop when infusions are performed incorrectly. Pain, dizziness, nausea, weakness and other discomfort should be reported to a healthcare professional immediately. The procedure algorithm is as follows:
- the patient takes a comfortable position - it is best to do the IV while lying down, but it is also possible in a semi-sitting or sitting position;
- the arm in the biceps area is tied with a tourniquet, the needle insertion site is thoroughly disinfected;
- the needle is inserted into the darkest, well-filled vein parallel to the surface of the arm at an angle of 35-45 degrees;
- after blood appears in the catheter, it is positioned as parallel to the limb as possible and fixed with an adhesive tape;
- connect the system tube to the catheter, make sure the connection is tight, and additionally secure it with a bandage;
- The rate of supply of the solution is adjusted using a dial with a wheel - sometimes the number of drops is marked on it to make counting easier.
During the procedure, it is necessary to monitor the patient and the needle insertion site. If the fluid flows too quickly, the person may become dizzy. In such a situation, it is better to simply reduce the infusion rate by turning the wheel in the desired direction.
After completing the procedure, it is necessary to close the system, carefully remove it, apply cotton wool soaked in alcohol to the injection site and press well. You need to keep it for at least 10-15 minutes, and preferably 20-25 minutes. During this time, a blood clot will form, which will clog the wound. If you remove the cotton too quickly, drops of blood will get under the skin, resulting in a bruise or bruise. Do not rub or touch the injection site, as this can also lead to the accumulation of blood clots.
Complications from improper infusion
When carrying out the procedure, it is necessary to strictly follow all the rules - placement technique and asepsis. An incorrectly placed IV carries the risk of complications, which include:
- bruise or hematoma at the injection site;
- vessel damage;
- bumps under the skin due to the accumulation of the drug;
- unintentional introduction of a small (infiltration) or significant (extravasation) amount of solution into surrounding tissues;
- vein spasm;
- inflammation of the vein with the formation of a blood clot;
- tissue infection;
- air embolism.
Complications also include allergic reactions to the drug. They can be minor (itching and rash in the area where the solution was administered) or severe - Quincke's edema and anaphylactic shock. In any case, the patient should be left under the supervision of a doctor - sometimes minor allergic reactions lead to serious consequences.
Filler Juvederm Volbella
An excellent product for replenishing volume is the American filler Juvederm Volbella, which contains hyaluronic acid, phosphate buffer and lidocaine.
Hyaluronic acid gives an immediate hydration result after the filler is injected into the hands. It has the ability to retain moisture in cells for a long time, due to which severe dryness and irritation of the skin disappears. In this case, the task of the phosphate buffer is to regulate the amount of intracellular fluid so that it does not accumulate too much and swelling does not occur.
The Juvederm gel itself has a very delicate texture and easily fills problem areas of the skin. Lidocaine, which is part of the filler, helps get rid of painful or unpleasant sensations during injection under the skin.
After the procedure, the skin becomes more elastic, firm, its tone noticeably increases, and volume is added. The plastic consistency allows you to obtain an even skin texture and achieve noticeable rejuvenation. Accordingly, immediately after the procedure, the veins cease to be visualized.
Kuznetsova Ekaterina Olegovna
Nutritionist, gastroenterologist, cosmetologist
A pronounced rejuvenating effect, as evidenced by numerous reviews, occurs within a few hours from the moment of injection. At the same time, there is no feeling of unnaturalness; on the contrary, the gel is practically not felt under the skin. The anti-aging effect lasts for 9-18 months. After this, the gel begins to gradually dissolve and be eliminated naturally from the body.
What to do if complications develop?
The most dangerous complication of an incorrectly placed IV is an air embolism, or air bubbles entering the bloodstream. It rarely causes death - according to experts, in order to cause death, at least 200 ml of air must be injected into the vein. A small bubble simply dissolves in the cells, but sometimes it can impair the functioning of vital organs, so it is better not to take risks.
Symptoms of an air embolism depend on the size of the vessel affected and the amount of air trapped. The affected area swells, becomes painful, the skin turns blue or red, after which trophic ulcers and necrotic areas form. Tachycardia is possible, as well as manifestations from the affected organs. With pulmonary embolism, hemoptysis and pulmonary edema are observed, if the coronary or cerebral arteries are affected, heart attacks and strokes are possible with all the ensuing consequences. If signs of embolism appear, the patient should be hospitalized immediately.
Dangerous complications when intravenous infusion technique is violated include infiltration and extravasation, which can lead to unpleasant consequences. Injecting large amounts of medication past the veins can lead to severe tissue damage and necrosis. Treatment is carried out in a hospital under medical supervision.
The appearance of hematomas and bruises does not always depend on the experience or qualifications of the nurse. In some patients, the vessels are so fragile that they burst when the needle is inserted, resulting in a bruise. Such complications are not dangerous to health, but can sometimes lead to unpleasant consequences requiring medical intervention. You should consult a doctor if you have the following symptoms:
- painful sensations that increase and do not disappear for 2-3 days;
- increase in size of the bruise;
- muscle spasms;
- difficulty moving your hand;
- deterioration in general health (weakness, fever, headache);
- increased temperature at the site of the bruise.
Such signs indicate that an infection has entered the body, and sometimes the onset of necrotic processes. Normally, bruises disappear within 2-3 weeks, gradually changing color from bluish-purple to greenish and yellow. A bruise that does not go away for a long time is also a reason to consult a doctor, even if it is not accompanied by pain or malaise.
Phlebitis, or inflammation of the venous walls, usually develops after prolonged treatment with intravenous infusions, but when infected or administered caustic, irritating drugs, it can develop after several procedures. The vein area becomes dense and painful, body temperature rises to 38-39 degrees. Phlebitis is treated conservatively (anticoagulants, anti-inflammatory drugs) in combination with physiotherapy.
How to safely place an IV in case of “difficult” veins?
When inserting a needle into a person with thin, fragile, or hard-to-see veins, additional precautions must be taken. They allow you to avoid unpleasant consequences in the form of injuries, hematomas and bruises, and also make the procedure as painless as possible:
- Do not stretch the skin excessively. If the veins are pronounced enough to get to the right place, you can do without a tourniquet. Otherwise, it is better to take a soft tourniquet and not tighten it too much - this is especially true for older people, as well as patients with thin skin and fragile veins.
- Reduce the number of procedures. If possible, it is necessary to reduce the number of vein punctures - administer several drugs in one dropper or one after another. Do not forget that mixing medications yourself can lead to undesirable consequences - this issue should be discussed with your doctor.
- Use a needle with a small diameter. To administer most solutions, a needle with a minimum diameter is sufficient. Exceptions include viscous, thick preparations; extreme caution should be exercised when administering them.
- Do not press the needle too hard. If the needle is sharp enough, there is no need to press too hard. For insertion, a smooth, gentle movement with slight pressure is sufficient.
- Insert the needle parallel to the skin. This is done in order to reduce the risk of through vein puncture. The skin over the vessel should be slightly stretched and secured so that it does not slip.
- Do not rush. When placing an IV, haste can lead to unpleasant consequences - you need to act slowly and carefully.
When the needle is inserted correctly, the patient feels slight discomfort when applying a tourniquet and performing a puncture. Unpleasant sensations during the infusion of the solution, including dizziness, nausea, weakness and darkening of the eyes, indicate that the infusion is not going properly.
Other ways to make veins more visible
There are several more methods on how to pump up your arms so that all the veins are visible.
- For example, you need to drink a lot of water. This will help the muscles to be in a “puffed up” state. That is, water will not be retained in the body.
- Another way would be to increase your potassium intake. It will help remove excess fluid from the body.
- It is worth paying attention to the amount of carbohydrates consumed. If you want to become the owner of toned arms with visible veins, it is best to limit the amount of carbohydrates. They make it more difficult for fluid to drain out and the veins will be less visible. Also, reducing carbohydrates will help reduce the amount of fat in the body.
Thus, to achieve textured veins, you need to combine regular exercise with a special diet.
How can you tell if the medicine is going past the veins?
To prevent infiltration and extravasation, the patient must be closely monitored during the procedure. List of warning signs:
- unnaturally shiny, dense, stretched skin at the site of needle insertion;
- tension and the appearance of swelling (rapidly growing swelling is especially dangerous);
- change in the shade and temperature of the hand - redness, blueness, too cold skin;
- self-slowing or stopping the flow of medication;
- continuation of the infusion after applying a tourniquet to the vein;
- leakage of solution around the injection site;
- burning or discomfort in the area where the needle is located.
If such symptoms occur, stop the infusion immediately and remove the needle. The injection site must be carefully examined, and if a large amount of solution is injected past a vein (especially if it is viscous or caustic), you must immediately consult a doctor. To eliminate the consequences in such cases, the introduction of an antidote is required.
If the amount of the drug that gets into the tissue is small, you need to monitor the affected area for 2-3 days. At the first manifestations of necrosis, immediately contact a medical facility.
If a vein is damaged, it is necessary to press it for a few minutes, and then apply a dry sterile bandage; if a hematoma appears, apply a compress. If the patient's condition has not worsened, the IV can be reinserted into another vein.
Diagnosis of thrombosis
When visiting a medical facility, the doctor diagnoses the pathology and prescribes treatment. The main methods used to detect thrombosis are:
- coagulogram - blood test for clotting;
- magnetic resonance venography;
- duplex\triplex scanning of the veins of the upper extremities;
- ascending venography using a contrast agent;
- radionuclide scanning of the location of the thrombus;
- thromboelastography.
Ultrasonography
Ultrasound duplex scanning of veins is the “gold standard” for diagnosing thrombosis localized in the upper extremities. The technique allows you to quickly, highly informatively and non-invasively obtain information about the state of venous blood flow. The method is ideal for visualizing the veins of the extremities, neck, axillary and subclavian areas.
CT scan
Another popular method for diagnosing thrombosis. It is used mainly urgently, in case of suspected dangerous complication of deep vein thrombosis - pulmonary embolism. CT allows you to quickly assess the extent of the problem and select the most appropriate method of providing emergency medical care.
Where do they put an IV if the veins in the arms are bad?
If it is not possible to place a drip into a vein in the bend of the elbow, the nurse chooses another location. Inserting a needle into small vessels is strictly not recommended. It is extremely difficult to get into them, and problems subsequently arise much more often - hematomas and phlebitis are possible. The examination begins from the back of the hand, where the vessels are also quite large and well defined. A catheter is usually placed there - the bend of the elbow is not suitable for this purpose, since the device can be easily damaged when bending the arm.
Next, the veins of the forearm are examined, and a place is chosen as low as possible. The vessels that run along the outside of the forearm near the wrist are rarely used - they run close to nerves, so there is a high risk of damage. IVs are also practically not placed in the veins of the inner part of the arm below the elbow (the so-called antecubital fossa). When the solution gets into nearby tissues, compression of important anatomical structures occurs, which threatens damage to the veins and necrosis.
Droppers are placed in the veins of the legs extremely rarely - only when it is impossible to administer the drug in any other way. The vessels are more prone to inflammation and phlebitis, and the procedure is extremely painful - the skin on the lower extremities is rough, so it is much more difficult to pierce it. There are no large veins other than the central femoral ones, and the popliteal ones are inconvenient due to their location.
In the absence of other options, doctors choose the “veins of last resort” for infusions, that is, the central ones. These include:
- subclavian (under the right or left collarbone);
- internal jugular on the sides of the neck;
- femoral, which are located in the groin, are used extremely rarely due to the high risk of complications.
Such intravenous infusions are a minor surgical operation - first, catheterization is performed, after which medicinal solutions are administered. Catheterization is carried out under anesthesia and ultrasound control - some vessels are invisible to the eye, so it is impossible to determine without appropriate landmarks.
It is especially difficult to give IVs to newborns or infants. The veins in their arms are very thin, so not every experienced nurse can get into them. In addition, young children are unable to lie completely still for long periods of time, which increases the risk of injury. For such patients, IVs are often placed in the legs or veins in the head - such a procedure often shocks parents, but significantly reduces the risk of complications.
Carrying out the procedure on your own can lead to serious complications, so it is better to consult an experienced healthcare professional. To install an IV in Moscow at prices lower than in commercial clinics, you need to call a qualified nurse by calling the phone number on our website. An experienced specialist will perform the procedure quickly, painlessly and absolutely safely!
We put in an IV
As you know, a dropper is one of the most effective ways to administer medicine to a patient, so the skill of correct installation will be useful to everyone.
Initial training
The preparation is simple, but this does not negate its importance:
- Prepare your stand.
- Wash your hands. This is a mandatory step, and you need to wash your hands correctly. Wash your palms first, then the backs of your hands and the areas between your fingers.
- Prepare a kit that includes a tube and a clamp. If you are giving an IV to a child, a microset is recommended; for adults, a macroset is recommended.
- Select a needle. The rule here is: the longer the needle, the thinner it is.
- Prepare your tools.
It is recommended to put the devices in one place.
Preparing the IV
Everything is simple here: you need to take the package with the medicine and find its connection point. This is where the set is inserted. Rub this area with cotton wool and alcohol.
Then you need to connect the dropper to the bag and hang it on the stand. Often non-professionals do not notice that there are bubbles in the system. To get rid of them, you need to carry the liquid to the end of the tube.
It is important that the tube does not touch the floor. This is important because the IV is sterile and free of germs. There are always bacteria on the floor, including harmful microorganisms.
Bibliography
- Mukhina S. A., Tarnovskaya I. I. Practical guide to the subject “Fundamentals of Nursing”: textbook. - M.: Rodnik, 2005.
- www.who.int World Health Organization Publications WHO WHO/GSBI: Injection Safety and Related Procedures Toolkit.
- Savelyev N. “Injections, IVs, dressings and other medical procedures and manipulations”: - M.: AST, 2021.
- Bikkulova D.Sh. Venous access protocols are a comprehensive solution to CVC problems. //Journal Polyclinic 1(2)/2014
- Briko N.I., Bikkulova D.Sh., Brusina E.B., et al., Prevention of catheter-associated bloodstream infections and care of the central venous catheter (CVC). //Clinical recommendations. — M.: “Remedium Privolzhye”, 2021