Polycythemia vera
(IP) is a clonal myeloproliferative disease of a chronic nature with a relatively benign course, affecting hematopoietic stem cells and accompanied by the proliferation of three hematopoietic lineages. It is characterized by an increase in the number of red blood cells, an increase in the concentration of hemoglobin, blood cells (leukocytes, erythrocytes, platelets) and total blood volume.
Polycythemia vera is also known as Vaquez's disease, true, or red, erythremia. Belongs to orphan (rare) diseases. It mainly affects people over 60 years of age, more often men. In young people, the disease is less common but has a more unfavorable course.
According to ICD-11, IP is assigned code 2A20.4.
Classification
There are two known forms of this disease:
| Polycythemia vera. Occurs due to pathological changes in the blood | By diagnosis | Primary polycythemia. It develops as an independent pathology. |
| Secondary polycythemia. Occurs against the background of other diseases - tumor formation, pulmonary failure, hydronephrosis (enlargement of the renal pelvis and renal calyces). | ||
| By stage | Initial polycythemia: symptoms are virtually invisible or absent. May last for several years. | |
| Full-blown polycythemia. May affect the spleen. It has been going on for more than 10 years. | ||
| Severe polycythemia. Oncological tumors appear on various organs and malignant blood pathologies. | ||
| Relative polycythemia | Stress polycythemia. It is caused by excessive workload, unhealthy sleep and eating habits, and too strenuous work. | |
| False polycythemia. With this diagnosis, the number of blood cells is normal. | ||
Changes in working conditions
With this disease, young patients suffering from stages I and IIA erythremia in remission are considered to be able to work. Moreover, their condition should not be complicated by vascular pathologies.
For patients with polycythemia there are certain contraindications and the following working conditions are recommended:
- Stage I. Activities that require excessive physical effort or psycho-emotional stress are prohibited. Work in an unfavorable microclimate and interaction with hemotoxic substances are also contraindicated.
- Stage II. Work associated with a forced uncomfortable body position, moderate physical activity and neuropsychic stress, vibration exposure, exposure to heights, changes in temperature, pressure, etc. is not recommended.
- Stage III does not allow patients to work under normal production conditions for a healthy person.
Symptoms of polycythemia vera
Causes
Unfortunately, doctors are still unable to say with absolute certainty what exactly causes this disease. The generally accepted version is that the disease is caused by a mutation in one of the brain enzymes. For this reason, blood cells begin to divide rapidly. Hence their excessive quantity (this especially applies to red blood cells). It has been noted that predisposition to Vaquez disease may be genetic: the diagnosis of “polycythemia” is often made to close relatives.
There is also an opinion that the development of the disease can lead to:
- excessive x-ray exposure;
- previous tuberculosis or intestinal infection;
- poor working conditions - for example, frequent contact with paints and varnishes in production.
Can this disease be controlled?
With regular therapy, which protects against thrombotic complications, bleeding and infections, the life expectancy of people with PV is almost the same as that of their healthy peers. The essence of therapy is to reduce the production of blood cells and prescribe drugs that reduce the risk of thrombosis. The doctor selects the regimen, having previously calculated which risk group for thrombosis the patient belongs to.
The simplest method of treatment is the use of regular aspirin to prevent arterial thrombosis, which provokes the development of stroke and myocardial infarction. Another traditional method is conventional blood exfusion, that is, bloodletting. Periodically, 500 milliliters of blood are taken from a person two to three times a week until the hematocrit level decreases to normal.
Read also
Invisible War
Finally, there are treatment methods based on modern medicines. Patients under 70 years of age are prescribed interferon drugs, which are administered subcutaneously three times a week. Special pen syringes look like those used by people with diabetes to inject insulin. These drugs belong to the so-called cytokines - regulatory protein molecules that are normally produced by cells of the human immune system. Older people are prescribed a cytostatic drug, hydroxyurea.
Symptoms (signs)
Often this disease does not manifest itself at all. This can last for years. Sometimes it is detected during examination for a completely different disease. In this case, we can say that the patient is lucky (especially if the stage of polycythemia is not advanced).
But it also happens that the disease is accompanied by a chain of symptoms. The organs of a person suffering from Vaquez disease become excessively filled with blood. Hence a whole series of signs.
A patient with polycythemia typically:
- enlargement of veins, noticeable to the naked eye - for example, the veins in the arms look swollen;
- redness of the eyes;
- purple skin tone (visible on the face and neck);
- pressing pain in the chest, especially after lifting weights;
- sharp pain in the limbs, fingertips (when taking medications that thin the blood, the pain subsides);
- a feeling that the skin of the body is itching (the symptom occurs due to increased blood circulation and dilation of skin capillaries);
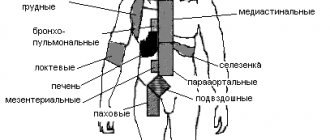
- the size of the liver and spleen is too large compared to the norm (the symptom occurs due to a strong concentration of red blood cells). The enlargement of these organs, in turn, provokes a feeling of heaviness in the abdomen. Unpleasant sensations in the left side of the abdomen are a sign of an enlarged spleen, heaviness in the right side of the abdomen is a signal of an increase in the size of the liver;
- thrombosis in large vessels, especially in the leg veins;
- thrombosis of small vessels of the intestinal mucosa, which can provoke duodenal ulcer;
- sometimes – bleeding gums;
- poor general condition of the body: high blood pressure, fatigue, migraine, tinnitus, difficulty breathing.
Please note: such obvious signs of illness as facial redness do not always appear. Diagnosis is also complicated by the fact that the symptoms of polycythemia are similar to those of other diseases. Therefore, it simply does not occur to many people to be examined for polycythemia. But it can be detected by a simple blood test.
Diagnostics
Vaquez disease is detected in modern medical laboratories.
To diagnose it, the following is carried out:
- General examination of the patient's blood. In favor of the diagnosis of “polycythemia” will be said:
- a large accumulation of red blood cells, and they can increase in size;
- increased platelet count (the higher the number, the more severe the disease);
- increased hemoglobin level;
- high hematocrit number (the ratio of red blood to plasma).
- Testing the patient's blood for biochemistry. Polycythemia will be indicated by:
- increased content of alkaline phosphatase, an enzyme responsible for phosphorus-calcium metabolism;
- accumulation of uric acid, a by-product of metabolic processes.
- Radiological diagnostics (determines the level of circulating red blood cells).
- Cytological analysis (study of bone marrow at the cellular level).
- Histological diagnosis of red bone marrow (examination of material from the ilium).
Additionally, the doctor may ask the patient to undergo an ultrasound of the internal organs. This is done to determine the size of the liver and spleen.
Medical and social examination
MSE and disability in polycythemia MSE and disability in erythremiaPOLYCYTHEMIA TRUEPolycythemia vera (erythremia, Vaquez disease) is a variant of chronic leukemia of a myeloproliferative nature involving all three lineages of myeloid hematopoiesis in the pathological process, characterized by a relatively benign course. Incidence 0.6-1.6 per 100,000 population; Mostly people over 50-60 years old are affected, men somewhat more often than women. Clinical symptoms of the disease are associated with an increase in circulating blood volume, slower blood flow, increased blood viscosity, which leads to deterioration of microcirculation and a tendency to thrombosis.
Diagnostic criteria
Category A 1. Increase in the mass of circulating red blood cells: for men - 36 ml/kg, for women 32 ml/kg. 2. Normal blood oxygen saturation (more than 92%). 3. Splenomegaly. Category B 1. Leukocytosis more than 12x10*9/l in the absence of infection or intoxication. 2. Thrombocytosis more than 400x10*9/l in the absence of bleeding. 3. Increase in neutrophil alkaline phosphatase in the absence of infection or intoxication. 4. Increasing the ability of blood serum to bind vitamin B12. The diagnosis is reliable with any 2 positive signs of category A and B or all three signs of category A.
ClassificationStage I
— initial: subjective well-being. Moderate plethora. The content of erythrocytes in men is more than 5.5x10*12/l and hemoglobin is more than 177 g/l; in women, erythrocytes - more than 5.0x10*12/l and hemoglobin - more than 157 g/l. The content of leukocytes and platelets is within normal limits. In the bone marrow there is focal hyperplasia of the myeloid lineage.
Stage IIA
- extensive (without myeloid metaplasia of the spleen): pronounced plethora, slight spleno- and hepatomegaly, arterial hypertension, vascular complications. Pancytosis, neutrophilia with band shift. Total three-line hyperplasia of the bone marrow.
Stage IIB
(with myeloid metaplasia of the spleen): severe splenohepatomegaly, urate diathesis. Pancytosis with leukocytosis above 15x10*9/l and a shift in the blood count to myelocytes, single erythrokaryocytes. Panmyelosis with focal myelofibrosis. Myeloid metaplasia of the spleen.
Stage III
(terminal, often anemic) - outcomes in myelofibrosis, acute leukemia, chronic myeloid leukemia. Anemia, thrombocytopenic, hemorrhagic syndrome, splenohepatemegaly, hyperuricemia, infectious complications. The initial and IIA stages last up to 15 years or more, stage IIB - about 3-5 years. The terminal stage lasts several months.
An example of a diagnosis:
Polycythemia, stage IIA, acute phase. Chronic coronary insufficiency, stage I. The prognosis is determined by the stage and nature of the disease.
Treatment.
Pathogenetic therapy - cytostatics (imifos, myelosan, myelobromol and others). The course dose of myelosan is about 300 mg. With maintenance therapy, remissions can last up to 5-6 years. P32 is rarely used, mainly in elderly patients. Symptomatic therapy - bloodletting in the initial stages of the disease of at least 500 ml in combination with antiplatelet agents. The number of hemoexfusions is carried out taking into account the volume of circulating blood until the hematocrit and red blood parameters are normalized.
MSE for polycythemia
Young patients in stages I and IIA, in the remission phase, who do not have vascular complications, are considered able to work. VUT: during the period of exacerbation of the disease and the occurrence of vascular and other complications. The duration of VUT is from 2 weeks to 4 months. Working capacity is restored in the remission phase, after the cessation of angina attacks, reduction and stabilization of blood pressure levels, and normalization of central hemodynamics.
Contraindicated types and working conditions
In stage I, work associated with significant physical and neuropsychic stress, in unfavorable microclimatic conditions, and contact with hematological poisons was contraindicated. In stage II, in addition, work associated with moderate physical and neuropsychic stress, forced body position, vibration, exposure to heights, changes in pressure, temperature, etc. is contraindicated. In stage III, patients cannot work in normal production conditions .
Indications for referring patients to MTU:
a) stage II polycythemia, if it is necessary to transfer the patient to work in another profession, lower qualifications, or a significant decrease in the volume of production activity; b) terminal stage polycythemia; c) the course of the disease with vascular complications leading to severe dysfunction of the cardiovascular system.
The required minimum examination when referring patients to medical examination:
a) general blood test, determination of platelet count; b) hematocrit; c) sternal puncture, coagulogram; d) ECG; e) according to indications - bicycle ergometry, study of central hemodynamics, external respiration function, fundus of the eye.
Disability is not established if the patient has: - latent, sluggish, indolent form of polycythemia without signs of progression with minor impairment of body functions. Disability of the 3rd group is established if the patient has: - polycythemia with moderate dysfunction of the blood and immune system during therapy. Disability of the 2nd group is established if the patient has: - polycythemia with severe dysfunction of the blood and immune system during therapy. Disability of the 1st group is established if the patient has: - terminal stage of the disease, with significantly pronounced dysfunction of the blood and immune system, transformation into acute leukemia. DISABILITY CRITERIA FOR POLYCYTHEMIA IN CHILDREN IN 2021 Disability is not established if the child has: - latent, sluggish, indolent form of polycythemia without signs of progression with minor impairment of body functions. Category “disabled child” is established if the patient has: - polycythemia with impaired blood and immune system function from a moderate degree or higher during therapy.
A patient can receive an official conclusion on the presence (or absence) of grounds for establishing disability only based on the results of his examination at the ITU Bureau relevant region
.
The procedure for completing documents for undergoing MSE (including the algorithm of actions in case of refusal of attending physicians to refer a patient to MSE) is described in sufficient detail in this section of the forum: Registration of disability in simple language
Source
Treatment
Once the diagnosis is made, the patient is sent to the hematology department. What tactics will the doctor choose to combat the disease? It depends on the stage of the disease.
Typically, polycythemia is treated:
- By bloodletting. This ancient method helps to quickly reduce the number of red blood cells. The level of hemoglobin in the blood also decreases. Blood is taken every week in an amount of 200 to 300 milliliters (depending on the constitution of the body and the condition of the patient). Sometimes standard bloodletting is replaced by erythrocytopheresis, a procedure consisting of three stages:
- blood sampling;
- separation of red blood from plasma;
- return of plasma to the body.
- The use of cytostatics - drugs that inhibit the process of cell division.
- Intramuscular injection of interferon, a drug that strengthens the immune system. This medication has another effect - it enhances the effect of cytostatics.
- Taking antiplatelet agents - drugs that prevent blood clots from forming (the method is not suitable for ulcers - in their case there is a risk of internal bleeding).
Indications for MSEC
A patient with erythremia is referred to undergo a medical and social expert commission (MSEC) by his attending physician, who is guided by the presence of a certain number of indications in a particular patient. These include:
- Stage II of the disease when there is a need to transfer the patient to a position of lower qualifications, another profession, or the need to reduce the volume of activities performed;
- terminal stage of erythremia;
- the course of the disease with vascular complications leading to significant dysfunction of the cardiovascular system.
Forecast
If we are talking about polycythemia vera, the doctor’s prognosis will depend on the degree of development of the disease. Unfortunately, without timely therapy, about 1/3 of patients die within 5 years from the onset of the disease. If effective treatment is carried out, there is a real chance to extend life by decades.
Please note: Vaquez disease should not be treated on your own. Firstly, it is completely useless, and secondly, precious time is wasted. Tactics for combating polycythemia should be developed by an experienced doctor who has studied the patient’s body and the severity of the disease.
Determination of disability
When conducting a commission to determine the degree of disability, medical experts are guided by the following criteria. A patient is not entitled to disability in case of a latent, indolent (sluggish) form of erythremia without symptoms of progression with unexpressed dysfunction of organs.
Group 3 is assigned to Vaquez disease with moderately manifested blood and immune dysfunctions during the treatment provided to the patient. Group 2 is provided for severe deviations in the activity of the circulatory and immune systems during the therapy.
Group 1 is assigned to the terminal stage, accompanied by significant impairments in the functioning of the circulatory and immune systems, against the background of developing acute leukemia. The category “disabled child” is provided for polycythemia with blood and immune dysfunction, starting from a moderate degree and further on the background of treatment.
Nutrition
Treatment for polycythemia requires a strict diet, as is the case with aortic aneurysm. The first and main rule: you must give up meat. Fatty meat foods rich in cholesterol do not thin the blood, but rather thicken it. This is why a patient with polycythemia should switch to a vegetarian diet as soon as possible.
The “green list” includes the following products:
- milk and its derivatives – fermented baked milk, kefir, yogurt, low-fat cottage cheese;
- tomatoes;
- bell pepper of any color;
- pumpkin;
- celery;
- cucumbers, zucchini, gherkins;
- nuts;
- sprouted grains;
- seaweed;
- beans;
- linseed oil;
- melon;
- orange, lemon, pomelo, grapefruit;
- blueberries, strawberries;
- cherry;
- ginger root (added to salads and soups).
Doctors advise paying special attention to your drinking regimen. It is recommended to drink a lot of water - at least 1.5 liters per day. However, you should try to do this in small portions - a few sips every 15-20 minutes.