Often we are faced with poor health and try to understand what is the cause of this condition. And when many laboratory and instrumental tests have already been carried out and nothing has been found, we think: “What could this be connected with? Because I really feel bad.” If there are no organ damage, it’s time to consult a neurologist. Autonomic dystonia syndrome, autonomic failure, autonomic crises are neurological diseases that we will touch on in this article.
Autonomic dystonia syndrome
Autonomic dystonia syndrome is all forms of disturbance of autonomic regulation, most often secondary manifestations of various pathologies.
There are 3 forms of SVD:
- psychovegetative – a feeling of tightness in the chest, changes in heartbeat, stomach pain, frequent vomiting, headache, dizziness, neuralgia of various locations, problems with urination, increased sweating, changes in the menstrual cycle, feeling cold;
- peripheral autonomic failure syndrome - (see autonomic failure);
- angiotrophalgic - vascular (marbling of the skin, redness, pallor, cyanosis, feeling of numbness, tingling), trophic (peeling and thinning of the skin, spots of pigmentation or depigmentation, ulcers, more often in the area of the hands and feet, brittle nails) and painful manifestations (paroxysmal prolonged pain , having a shooting, aching, burning, tingling, etc. character.
Symptoms
The symptoms of neurocirculatory dystonia are very diverse and form the basis for the classification of pathology. However, it is possible to identify a number of common features that are characteristic of most types of NDC:
- frequent mood changes;
- constant fatigue and drowsiness;
- lack of strength, weakness;
- feeling of a lump in the throat;
- increased sweating;
- weather sensitivity;
- anxiety;
- feeling of lack of air, etc.
An exacerbation of the disease can be triggered by any stressful situation: an excess of positive or negative emotions, lack of sleep, or even a simple change in time zones.
Autonomic failure
Autonomic failure is a syndrome associated with impaired innervation of internal organs, blood vessels and endo- and exocrine glands.
In most cases, it is a progressive autonomic failure. In turn, MNV includes primary violations:
- idiopathic orthostatic hypotension;
- some hereditary and acquired diseases of the nervous system (multiple system atrophy, hereditary sensory-vegetative polyneuropathy)
Secondary violations include:
- for endocrine system disorders (diabetes mellitus, thyroid disease);
- for systemic and autoimmune diseases;
- for metabolic disorders;
- with paraneoplastic syndrome;
- for infectious diseases (HIV, leprosy, herpetic infections, etc.).
Various symptoms may occur:
- from the cardiovascular system: tachycardia at rest, orthostatic fainting, arterial hypertension in the supine position;
- from the respiratory system: sleep apnea, involuntary attacks of suffocation;
- from sweating: hypo- and anhidrosis, increased sweating;
- from the gastrointestinal tract: constipation, diarrhea, nausea, vomiting, anorexia;
- from the urinary system: urinary disorders, erectile dysfunction.
Diagnosis of this disease is carried out by physical examination, checking neurological status and drug tests.
Diagnostics
In the process of diagnosing neurocirculatory dystonia, especially of the mixed type, it is important for the doctor to exclude other causes of similar symptoms. The patient will undergo a thorough examination, including:
- collecting complaints and medical history, clarifying all details of the course of the disease;
- standard examination, including assessment of the functioning of the main body systems, including both sections of the ANS;
- general blood test to exclude inflammatory manifestations;
- general urinalysis to exclude renal pathologies;
- biochemical blood test, which necessarily includes a study of glucose and cholesterol levels, hormonal status, blood clotting and markers of autoimmune processes;
- ECG, ultrasound of the heart;
- daily monitoring of ECG and blood pressure;
- functional load tests (bicycle ergometry, treadmill) to assess the heart’s response to stress and determine the “safety margin”;
- chest x-ray, spirometry if necessary (if the patient complains of shortness of breath and a feeling of lack of air);
- rheoencephalography, Doppler ultrasound of the head and neck vessels: to assess the quality of blood supply to the brain and its structures;
- MRI of the head, x-ray of the sella turcica to visualize or exclude space-occupying formations;
- electroencephalography if one or another form of epilepsy is suspected.
During the examination, the patient also consults with a therapist, neurologist and cardiologist. If necessary, doctors of other specialties are involved: psychiatrist, endocrinologist, pulmonologist, gynecologist, nephrologist, etc.
Vegetative crisis
Autonomic crisis (panic attack) is a series of clinical manifestations characteristic of emotional disorders and disorders of the autonomic nervous system, depending on the predominance of sympathetic and/or parasympathetic innervation. The obligatory presence of anxiety, a feeling of fear (even fear for one’s life), although there is no visible threat, fear of going crazy, harming loved ones or oneself.
Vegetative crises are divided into:
- hyperventilation crisis - rapid breathing, feeling of lack of air, difficulty breathing. Fear of loss of consciousness or death. There is also tension in the muscles of the forearm and hand, legs and feet. It is important to note that the attack may end in fainting
; - vagotonic crisis - rapid heartbeat, difficulty breathing, sweating, arterial hypotension, redness of the facial skin, disruption of the gastrointestinal tract, and can also result in fainting. A crisis can be provoked by being in a stuffy room, during fasting, intense exercise, or anxiety;
- mixed crises combine the above symptoms, which can appear in turn.
It is important to carry out differential diagnosis with somatic diseases: hypo-, hyperthyroidism, diabetes mellitus, pheochromocytoma, heart rhythm and conduction disorders, gastritis, peptic ulcer, epilepsy, neuroendocrine tumors.
How to help someone suffering from vegetative-vascular crises
Treatment of vegetative-vascular crises is always symptomatic. They rarely last more than five minutes. A person needs to provide a flow of fresh air, as well as peace of mind. During exacerbations, it is necessary to avoid excessive physical activity and try not to be nervous.
To prevent such crises from recurring, it is very important to establish optimal sleep, work and rest patterns. It is useful to do gymnastic exercises. It is important to stop drinking alcohol and smoking. The patient needs to establish a diet with a predominance of fresh fruits and vegetables.
Kinds
Fears can be different: fear of falling, fear of crowds, fear of open spaces. The vegetative crisis lasts within 20–40 minutes. According to severity they are divided into:
- Lungs. Lasts 10–15 minutes. Up to two symptoms are present.
- Average. Lasts from 15 minutes to 1 hour. The state of health worsens and the person may faint.
- Heavy. Lasts from 1 hour. They interfere with living fully. You will most likely need medical attention.
There are regional and systemic vascular crises. The differences are that with regional ones there is a disruption of the blood supply in a certain part of the body. The consequences of such a crisis are migraines and Raynaud's disease. Symptoms of systemic vascular crises: increased or decreased blood pressure.
Which doctor should I see and what tests should I take?
For help in treating new-onset vegetative-vascular dystonia, you should contact a neurologist. But if vegetative symptoms recur periodically, then you need to visit a therapist to undergo a comprehensive examination, since this doctor can refer the patient to the necessary specialist.
The main types of research for vascular dystonia syndrome are:
- Measuring blood pressure at different time intervals;
- Carrying out EchoCG and ECG;
- X-ray of the chest in 2 projections;
- MRI of the brain, chest and peritoneum;
- Determination of blood glucose;
- Determination of catecholamines in urine and blood.
Signs and symptoms of the disease
If a person suffers from vegetative crises, frequent attacks are characterized by certain symptoms.
Anxiety, isolation, conscious avoidance of social life and other people, fear of death, frequent mental breakdowns are clear signs of a specific disease.
A sudden release of adrenaline into the bloodstream leads to the following symptoms:
- Tremor of the limbs;
- A distinct lack of oxygen;
- Increased heart rate;
- Increased anxiety, agitated state;
- Excessive sweating, increased body temperature followed by chills;
- Sudden weakness, sudden dizziness;
- Loss of consciousness;
- Feeling of pain in the left side of the sternum;
- Strong headache.
Any panic attack is a serious stress for the body. Autonomous crises do not disappear without a trace. The person begins to fear another attack, worries and again experiences very unpleasant sensations.
Clinical manifestations
Vascular crises have specific symptoms. In people suffering from VSD, attacks often depend on individual characteristics.
Neurotic vegetative crises are characterized by the absence of stereotypical construction. Their duration may vary. They are often of a mixed nature and are associated with emotional overstrain.
In total, experts distinguish 3 variants of attacks. Their symptoms are different. The variability of symptoms is based on the pathophysiological mechanisms that underlie the development of crises.
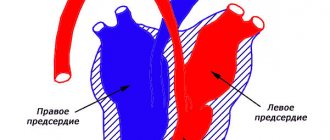
Manifestations of vegetative-vascular dysfunction are based on:
- disruption of the activity of certain departments of the ANS;
- hyperactivity of the sympathetic division of the ANS;
- hyperactivity of the parasympathetic division of the ANS.
Cardiac symptoms
An attack of VSD is characterized by:
- Arrhythmias.
- Changes in heart rate.
- Cardialgia.
Heart rates can either decrease or increase. The strong fear that arises against this background is combined with panic attacks. The person is afraid that “the heart will break” or “stop.”
Hypotensive symptoms
Attacks of vegetative vascular dystonia differ:
- A sharp decrease in blood pressure.
- Slowing down the heart rate.
- Lethargy, weakness.
- Frequent dizziness.
- Pain syndrome in the abdomen.
- Nausea.
- Pain in the chest.
Sometimes there are attacks of suffocation during VSD. Some patients experience shortness of breath.
Blood pressure readings range from 80 to 90/50 mmHg. Heart contractions slow down to 40-45 beats/60 seconds.
Hypertensive symptoms
The crisis of vegetative vascular dystonia is characterized by:
- Increased body temperature.
- Headaches.
- Increased heart rate.
- A sharp increase in systolic blood pressure.
Body temperature increases to 39 degrees. Headaches are quite painful. They often have a pulsating character. Heart contractions increase to 110-140 beats/60 sec. Systolic blood pressure rises to 140-180 mmHg.
Other symptoms
Vegetative-vascular paroxysms deserve special attention. There are crises:
- sympathetic-adrenal;
- vagoinsular;
- mixed.
In the first case, the VSD crisis is characterized by a rise in blood pressure. This condition is combined with headaches and heart pain, tachycardia, and trembling of the whole body. A person is haunted by a strong fear of imminent inevitable death.
In the second case, blood pressure decreases and an attack of suffocation occurs. There is a disorder of the gastrointestinal tract. The man sweats a lot and feels dizzy. Sometimes there are fainting spells.
In the third case, there is an alternation of these symptoms. Neurovegetative crisis is characterized by accelerated urination.
The cause of paroxysms may be a brain or skull injury.
Prevention
There are no specific preventive measures to avoid the development of the disease. But you can help the body cope with the onset of attacks faster. First of all, doctors recommend leading a healthy lifestyle. Drinking alcohol can further aggravate attacks and also increase their frequency.
During the interictal period, you will need to take folk remedies with a sedative effect. These can be tinctures of valerian, peony, motherwort. Regular visits to a psychotherapist will help build stress resistance. Various psychotherapeutic techniques help improve the patient’s mental state and help get rid of developed phobias.
With a strong desire, it is possible to cope with panic attacks. But this will require strict adherence to medical recommendations. Timely treatment is a serious step towards recovery.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Grekhov
Graduated from the Ural State Medical University with a degree in General Medicine. General practitioner
Vestibular consequences
Most clinically reported cases of vegetative crisis are not limited to a single attack. The patient remembers for a long time the sensations from the symptoms he experienced, and his further life activities are fixated on anxious anticipation. This behavior reinforces repetition, provoking behavioral restrictions, forcing a person to avoid dangerous situations.
The patient has depressive disorders, and vestibular consequences include the following symptoms:
- Frequent dizziness;
- Increased fatigue;
- Decreased activity.
Important! Competent and timely therapy leaves no room for negative symptoms of a vegetative crisis.
A vegetative crisis has a lot of unpleasant symptoms and requires immediate treatment. You should understand what a vegetative crisis is and try to maintain control over yourself when unwanted symptoms occur.
Causes
The development of autonomic neurosis is not caused by any single cause; it is usually the result of several factors:
- Traumatic brain injury with brain damage;
- Chronic fatigue, stress and depression;
- Consequences of certain infectious diseases;
- Wrong lifestyle;
- Mental and physical stress;
- Psychological trauma;
- Individual predisposition to neuroses.
Like many mental illnesses, this disorder often originates from a person’s childhood. Psychological trauma and shock experienced at an early age can develop into a serious illness after a few years. Moreover, not only people from disadvantaged families are susceptible to vegetative neurosis, but also ordinary children who lack the attention of their parents.
At an early age, monitoring the child’s psychological state is very important, since it is at this time that the foundation for adult life is laid. However, many parents, unfortunately, do not attach importance to this, accepting the child’s whims and tantrums as one of the manifestations of childhood.
When a person grows up, other factors influence his psycho-emotional state. Conflicts within the family, problems at work, social injustice - all this can cause autonomic neurosis.
Sometimes in adults, neurosis is caused by hormonal changes in the body, this is especially often observed in women during pregnancy. Also, the psychological state is affected by addiction to alcohol, drugs (and any poisoning in general), poor lifestyle or poor environment.
Treatment
In this matter, timely consultation with a doctor is of great importance. Based on the test results, comprehensive treatment is prescribed, including medication, psychotherapy and psychosocial treatment.
Important! Most often, treatment includes the use of psychotropic and sedative medications.
If an attack occurs, it is recommended to immediately take sedative herbal medicines. During pregnancy, a doctor's permission is required. If attacks are accompanied by low blood pressure, lethargy and weakness, a course of eleutherococcus and ginseng is prescribed. If you feel worse, give a Relanium tablet to chew.
Important! It is necessary to dispel the patient's fear of the existence of a life-threatening disease.
After identifying the cause of dystonia, treatment is prescribed by a doctor according to the profile of the underlying disease (allergist, psychologist, endocrinologist).
Traditional medicine recommends drinking infusions of hawthorn, motherwort, valerian, peony, and eating bananas and nuts. If necessary, electrophoresis and massage are prescribed.
But not all medications provide a long-term effect, since they temporarily block an attack without curing the psychological problem. Along with drug therapy, it is necessary to engage in psychological therapy. It is recommended to consult a psychologist who will competently diagnose and help get rid of the disease.
Complications and prognosis
In the majority of cases, an involuntary attack is not limited to one moment; for this reason, the patient creates a stable expectation of a subsequent crisis, creating a restless situation. Patients with crisis experience the following difficulties:
- Phobias – a person seeks to avoid these places and situations that may cause an attack.
- Depression - prolonged anticipation of a new attack negatively affects a single psycho-emotional background.
- Increased fatigue and decreased social activity are also considered complications of panic attacks.
The prognosis of the disease is positive if the patient does not delay the visit to the doctor, undergoes a multifaceted examination and receives additional support from a psychotherapist.
What causes severe crises
The root causes of such exacerbations are not yet fully understood. However, numerous studies and diagnostic results have made it possible to establish what may be the cause of the vegetative crisis:
- Hormonal imbalance and genetic predisposition;
- Long-term use of potent medications, stress, psycho-emotional imbalance;
- Endocrine disorders;
- Central nervous system disorders.
Often domestic violence and other social causes lead to an aggravation of a person’s condition, the first symptoms of a vegetative crisis.