Despite the fact that medicine does not stand still, much is known about diseases, their prevention and treatment, arterial hypertension occupies one of the first places among all diseases. According to statistics, at least 30% of adults on the planet suffer from hypertension. The disease requires regular monitoring and treatment, otherwise complications may arise, among them it is worth noting a hypertensive crisis.
Hypertensive crisis - symptoms and treatment, emergency care
By such an acute condition, doctors understand a sharp rise in blood pressure. Indicators can be significantly increased and amount to 240 to 120 mm of mercury. The patient feels unwell. He may experience:
- ringing appears in the ears;
- headache;
- vomiting or nausea;
- redness of the facial skin;
- legs and arms tremble;
- thirst;
- fast heart rate;
- spots in the eyes.
If such symptoms appear, emergency assistance is required. Most often, a crisis occurs in people with diseases that accompany hypertension. But sometimes it is diagnosed in those who did not have hypertension before. The following can contribute to the appearance of HA:
- menopause;
- hypertension;
- kidney diseases;
- lupus erythematosus;
- nephropathy in pregnant women,
- Itsenko-Cushing's disease;
- pheochromocytoma.
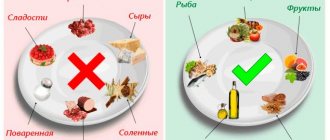
But sometimes this condition is provoked by too strong experiences, stress, tension, weather dependence, drinking alcohol, consuming large amounts of salty food. Despite the different reasons, the mechanism is the same, the regulation of vascular tone is disrupted.
It must be said that the manifestations of GC may differ and depend on the form of the disease. These include:
- water-salt;
- more dangerous – convulsive;
- neurovegetative.
Emergency care should always be prompt.
Prehospital care for sudden increases in blood pressure and hypertensive crisis
R
a sharp sudden increase in blood pressure (BP) to individually high values with minimal subjective and objective symptoms is considered as an uncomplicated hypertensive crisis (HC), and in the presence of dangerous or violent manifestations with subjective and objective signs of cerebral, cardiovascular and autonomic disorders is called complicated GK.
According to the National Scientific and Practical Society of Emergency Medical Care, over the past 3 years in the Russian Federation as a whole, the number of emergency medical services (EMS) calls for hypertensive crisis and the number of hospitalizations has increased by an average of 1.5 times. However, to date, at the prehospital stage, there is no clear algorithm for the use of drugs to provide emergency care for a sudden increase in blood pressure or blood glucose.
A sudden increase in blood pressure can be provoked by neuropsychic trauma, alcohol consumption, sharp fluctuations in atmospheric pressure, withdrawal of antihypertensive therapy, etc. In this case, two main pathogenetic mechanisms play a major role: vascular
– increase in total peripheral resistance due to an increase in vasomotor (neurohumoral influences) and basal (with sodium retention) arteriolar tone;
and cardiac
- an increase in cardiac output due to an increase in heart rate, circulating blood volume (CBV), and myocardial contractility.
Clinically, HA is manifested by subjective and objective signs. Subjective signs include headache, non-systemic dizziness, nausea and vomiting, blurred vision, cardialgia, palpitations and interruptions in cardiac function, shortness of breath; to objective - excitement or lethargy, chills, muscle tremors, increased humidity and hyperemia of the skin, low-grade fever, transient symptoms of focal disorders in the central nervous system; tachy- or bradycardia, extrasystole; clinical and ECG signs of left ventricular hypertrophy; accent and splitting of the second tone over the aorta; signs of systolic overload of the left ventricle on the ECG.
Thus, the diagnosis of GC is based on the following main criteria
: sudden onset; individually high rise in blood pressure; the presence of cerebral, cardiac and autonomic symptoms.
The tactics of providing emergency care depend on the severity of symptoms, the height and persistence of blood pressure, in particular diastolic blood pressure, as well as the cause that caused the increase in blood pressure and the nature of complications.
Depending on the characteristics of central hemodynamics, hyper- and hypokinetic GCs are distinguished (Table 1). The most common complications of GC are presented in Table 2.
The algorithm for relieving a hypertensive crisis is presented in Figure 1. When treating a sudden increase in blood pressure that is not accompanied by a violent clinical picture and the development of complications, mandatory medical intervention is required, which, however, should not be aggressive. One should remember about the possible complications of excessive antihypertensive therapy - drug collapse and a decrease in cerebral blood flow with the development of cerebral ischemia. Blood pressure should be reduced especially gradually and carefully (by no more than 20–25% of the initial value within 40 minutes) in case of vertebrobasilar insufficiency and the appearance of focal neurological symptoms. Moreover, the patient should be in a horizontal position due to the possibility of a sharper decrease in blood pressure. In the vast majority of cases, sublingual use of medications is possible to treat a sudden increase in blood pressure.
Rice. 1. Algorithm for relieving hypertensive crisis
In the absence of significant tachycardia, it is advisable to begin therapy for an uncomplicated crisis with 10–20 mg
of nifedipine
sublingually. The drug is characterized by good predictability of the therapeutic effect: in the vast majority of cases, after 5–30 minutes, a gradual decrease in systolic and diastolic blood pressure begins (by 20–25%) and the patients’ well-being improves, which allows one to avoid the uncomfortable (and sometimes dangerous) parenteral use of antihypertensive drugs for the patient funds. The duration of action of the drug is 4–5 hours, which allows you to begin the selection of planned antihypertensive therapy at this time. If there is no effect, nifedipine can be repeated after 30 minutes. Clinical observations show that the higher the level of initial blood pressure, the higher the effectiveness of the drug. Side effects of nifedipine are associated with its vasodilating effect - drowsiness, headache, dizziness, flushing of the skin of the face and neck, tachycardia. Contraindications: Tachy-Brady syndrome (as a manifestation of sick sinus syndrome); acute coronary insufficiency (acute myocardial infarction, unstable angina); severe heart failure; hemodynamically significant stenosis of the aortic mouth; hypertrophic cardiomyopathy; hypersensitivity to nifedipine. It should be taken into account that in elderly patients the effectiveness of nifedipine increases, therefore the initial dose of the drug when treating GC should be less than in young patients.
captopril sublingually.
at a dose of 25–50 mg. When taken sublingually, the hypotensive effect of captopril develops after 10 minutes and lasts for about 1 hour. Side effects of ACE inhibitors: angioedema; allergic skin reactions; impaired renal function (in patients at risk - increased levels of urea and creatinine, proteinuria, oliguria); dry cough (due to increased bradykinin levels and increased sensitivity of bronchial receptors); bronchospasm; arterial hypotension, headache, dizziness, weakness, fatigue, fainting, palpitations. Contraindications: bilateral renal artery stenosis; condition after kidney transplantation; hemodynamically significant stenosis of the aortic mouth, left atrioventricular orifice, hypertrophic cardiomyopathy. The use of ACE inhibitors is not indicated during pregnancy, including pregnancy eclampsia.
In case of hyperkinetic variant of hypertensive crisis, sublingual administration of clonidine
at a dose of 0.075 mg. The hypotensive effect develops within 15–30 minutes, the duration of action is several hours. Side effects: dry mouth, drowsiness, orthostatic reactions. Taking clonidine is contraindicated in cases of bradycardia, sick sinus syndrome, and atrioventricular block of II–III degree; its use is undesirable in acute myocardial infarction, severe encephalopathy, obliterating diseases of the vessels of the lower extremities, and depression.
If there are contraindications to the use of beta-blockers, magnesium sulfate
at a dose of 1000–2500 mg IV slowly (over 7–10 minutes or more), and if it is impossible to provide IV administration of the drug, it is permissible (as an exception) to administer the drug warm IM followed by warming the injection site. Magnesium sulfate has a vasodilator, sedative and anticonvulsant effect, reduces cerebral edema. Its use is especially indicated for GC, accompanied by the development of convulsive syndrome (in particular, with eclampsia in pregnant women), as well as with the appearance of ventricular arrhythmias against the background of increased blood pressure. The hypotensive effect develops 15–25 minutes after administration. Side effects: respiratory depression (can be eliminated by intravenous administration of 5–10 ml of 10% calcium chloride solution), bradycardia, second degree atrioventricular block. Contraindications: hypersensitivity, hypermagnesemia (renal failure, hypothyroidism), myasthenia gravis, severe bradycardia, second degree atrioventricular block.
When treating complicated HA, a rapid (within the first minutes, hours) reduction in blood pressure by 20–30% compared to the initial level is necessary. For this purpose, parenteral administration of drugs is mainly used.
HC with hypertensive encephalopathy requires rapid and careful lowering of blood pressure
, treatment and prevention of cerebral edema and convulsive syndrome.
To do this, use nifedipine
p.o. at a dose of 10–20 mg (chew).
If its effectiveness is insufficient, as well as if it is impossible to use sublingual medication (for example, with persistent vomiting), it is advisable to use magnesium sulfate
(1000–2500 mg IV slowly over 7–10 minutes) and IV administration of dibazole. Dibazol (5–10 ml of 0.5% solution) has a moderate hypotensive effect - a sharp decrease in blood pressure can in this situation worsen the patient’s condition. The hypotensive effect of dibazole is due to a decrease in cardiac output and dilation of peripheral vessels due to its antispasmodic effect; after intravenous administration, it develops within 10–15 minutes and persists for 1–2 hours. Side effects: paradoxical short-term increase in blood pressure; sometimes – increased sweating, feeling hot, dizziness, headache, nausea, allergic reactions. Contraindications: severe heart failure, hypersensitivity to the drug.
Depending on the severity of the corresponding symptoms, additional administration of 10 ml of 2.4% theophylline
IV slowly (over 5 minutes), 10 mg
diazepam
IV;
IV infusion of mannitol
at a dose of 0.5–1.5 g/kg (up to 40 g), followed by IV administration of furosemide;
Dexamethasone
(4–8 mg IV) may be used
For GC with stroke
it is necessary to stabilize blood pressure at a level exceeding 5–10 mm Hg.
the patient's usual blood pressure level. To do this, use a slow (over 7–10 minutes or more) intravenous administration of magnesium sulfate
at a dose of 1000–2500 mg (as an exception, intramuscular administration of the drug in a warm form followed by warming the injection site is acceptable).
If there is a contraindication to the use of magnesium sulfate, nifedipine
at a dose of 5–20 mg p.i. (chew), and if it is impossible to use this route of administration (for example, in coma), dibazole IV (i.m.) at a dose of 30–40 mg.
In the case of GC with acute left ventricular failure
the use of narcotic analgesics is indicated (1 ml of 1% morphine solution intravenously in fractional streams), intravenous drip administration of nitrates (nitroglycerin or isosorbide dinitrate intravenous drip at a rate of 50–100 mcg/min, not more than 200 mcg/min).
The hypotensive effect develops within 2–5 minutes from the start of the infusion. Furosemide
is administered intravenously at a dose of 60–80 mg (up to 200 mg). The hypotensive effect develops 2–3 minutes after administration and is caused at the first stage by the vasodilating properties of the drug (dilates peripheral veins, reduces preload), and only then by the diuretic effect and decrease in blood volume. Diuretics do not replace the effect of other antihypertensive drugs (since in most cases a hypertensive crisis is caused by vasoconstriction with normal or even reduced blood volume), but complement and enhance their effect. It should be remembered that the use of nitrates and diuretics is not indicated when cerebral symptoms or eclampsia develop against the background of a crisis.
In case of GC with the development of a severe attack of angina or myocardial infarction
Intravenous administration of narcotic analgesics (morphine hydrochloride intravenously in a fractional stream) and nitrates (nitroglycerin or isosorbide dinitrate subcutaneously or intravenously in a drip) is also indicated.
If anginal status, tachycardia and rhythm disturbances develop against the background of a hypertensive crisis, and in the absence of signs of heart failure, intravenous administration of beta-blockers
(propranolol) is also advisable. A necessary condition is the ability to carefully monitor blood pressure, heart rate and ECG (due to the risk of developing bradycardia, atrioventricular block, etc.).
For GC with aortic dissection
in parallel with the relief of pain with morphine or morphine with droperidol, it is necessary to reduce myocardial contractility and quickly reduce blood pressure to the optimal level (100–120 mm Hg for systolic and no more than 80 mm Hg for diastolic).
The drugs of choice are propranolol
(1 mg every 3–5 minutes until the heart rate reaches 50–60 per minute, pulse pressure decreases to less than 60 mm Hg, or until a total dose of 0.15 mg/kg is reached, or until the appearance of side effects) and
sodium nitroprusside
, in its absence -
nitrates
(nitroglycerin, isosorbide dinitrate).
Sublingual administration of nifedipine (10–20 mg p.i., chewed) is acceptable. The administration of beta-blockers should precede the administration of any drugs that can cause tachycardia; if there are contraindications to the use of beta-blockers, use verapamil
at a dose of 5–10 mg intravenously (administered over 2–3 minutes); if necessary, it is possible to re-administer 5 mg of the drug after 5–10 minutes.
In case of GC with pronounced vegetative and psycho-emotional overtones (a variant of a panic attack), parenteral administration of drugs should be avoided; propranolol (20 mg) and diazepam (5–10 mg) should be used sublingually.
In case of GC as a result of discontinuation of clonidine, beta-blockers are contraindicated. Clonidine is used
p/ya at a dose of 0.075–0.15 mg, repeated every hour (until a clinical effect is obtained or until a total dose of 0.6 mg is achieved) or intravenously (less advisable intramuscularly) at a dose of 0.15 mg.
It should be noted that to date, parenteral administration of clonidine, magnesium sulfate, as well as dibazole and droperidol is most often used for the treatment of GC at the prehospital stage. At the same time, with a sudden increase in blood pressure, in most cases, sublingual use of drugs, in particular nifedipine, is necessary and sufficient. The use of clonidine is limited by the poor predictability of the effect (regardless of the dose of the drug, in addition to collapse, it is even possible to increase blood pressure due to the initial stimulation of peripheral beta-adrenergic receptors) and the high likelihood of side effects. Intramuscular administration of magnesium sulfate is painful and uncomfortable for the patient, and is also fraught with the development of complications, the most unpleasant of which is the formation of infiltrates in the buttocks. Dibazol does not have a pronounced hypotensive effect; its use is justified only if a cerebrovascular accident is suspected. Intravenous administration of propranolol requires a certain skill from the doctor due to the possibility of serious complications. The use of diazepam and droperidol is indicated only in cases of severe agitation of patients. It should be taken into account that sedatives and hypnotics can “lubricate” the neurological clinic, making it difficult to timely diagnose complications of GC, in particular, cerebrovascular accidents. The use of drugs that have an insufficient hypotensive effect (no-shpa, papaverine, etc.) for GC is certainly not justified.
Indications for hospitalization are formulated in national recommendations for the diagnosis and treatment of arterial hypertension (All-Russian Society of Cardiologists, Section of Arterial Hypertension, 2001). Emergency hospitalization
indicated in the following cases: HA that is not relieved at the prehospital stage; GC with severe manifestations of hypertensive encephalopathy; complications requiring intensive care and constant medical supervision (stroke, subarachnoid hemorrhage, acute visual impairment, pulmonary edema).
Algorithm of actions
As you already understand, a crisis can be called a complication of hypertension. Help is provided in this case as quickly as possible. First of all, you should call an ambulance. If a person is nervous or afraid, the person must be calmed down so that the pressure does not rise even higher. It is important to ensure air flow into the room, it is necessary to unbutton clothes, it is important that breathing is controlled and as smooth as possible. An emergency medicine for blood pressure should be placed under the tongue; Captopril or Nifedipine, as well as Copoten or Corinfar, help well.
If the ambulance does not arrive, and the person has become worse, you can take the medicine again. If pain or compression appears behind the sternum, you need to take Nitroglycerin. In case of chills, it helps to surround the person with bottles, into which warm water is first poured, and wrap them up. Often, upon arrival of the medical team, it becomes clear that hospitalization is not necessary. All measures are taken on site.
Vital and essential medicines
Vital and essential drugs (VED) used in the provision of ambulance and emergency medical care
| Epinephrine 1 mg/ml 1ml | Meglumina sodium succinate 1.5% 500ml |
| Norepinephrine 2mg/ml 8ml | Sodium chloride solution complex (Potassium chloride + Calcium chloride + Sodium chloride) 400 ml |
| Dopamine 40 mg/ml 5 ml | Sodium chloride 0.9% 250 ml |
| Phenylephrine 10 mg/ml 1ml | Sodium chloride 0.9% 10ml |
| Hexoprenaline 5 µg/ml 2 ml | Lidocaine 10% 650 doses/38.0g |
| Xylometazoline 0.1% 10ml | Procaine 5 mg/ml 5ml |
| Activated carbon 250 mg | Lidocaine+ Chlorhexidine 12.5g |
| Nitroglycerin 1 mg/ml 10ml | Furosemide 10 mg/ml 2ml |
| Isosorbide dinitrate 1mg/ml 10ml | Fentanyl 50 mcg/ml 1ml |
| Isosorbide dinitrate spray 1.25 mg/dose 300 doses | Morphine 10 mg/ml 1ml |
| Magnesium sulfate 250 mg/ml 10ml | Tramadol 50mg/ml 2ml |
| Procainamide 100mg/ml 5ml | Ketorolac 30mg/ml 1ml |
| Lidocaine 20mg/ml 2ml | Paracetamol 100 mg (suppositories) |
| Amiodarone 50 mg/ml 3ml | Paracetamol 24mg/ml 100ml |
| Propranolol 10 mg | Droperidol 2.5 mg/ml 2 ml |
| Metoprolol 1mg/ml 5ml | Chlorpromazine 25 mg/ml 2ml |
| Metoprolol 25mg | Galantamine 2.5 mg/ml 1ml |
| Verapamil 2.5 mg/ml 2ml | Sodium dimercaptopropanesulfonate 50mg/ml 5ml |
| Calcium gluconate 100mg/ml 10ml | Sodium thiosulfate 300 mg/ml 10ml |
| Diphenhydramine 10 mg/ml 1ml | Naloxone 0.4 mg/ml 1ml |
| Chloropyramine 20 mg/ml 1ml | Diazepam 5 mg/ml 2ml |
| Chlorhexidine 0.05% 50ml | Digoxin 0.25 mg/ml 1ml |
| Povidone-iodine 10% 25 ml | Platyfillin 2 mg/ml 1ml |
| Hydrogen peroxide 3% 40ml | Drotaverine 20 mg/ml 2ml |
| Ethanol 70% 100ml | Caffeine 200 mg/ml 1ml |
| Atropine 1mg/ml 1ml | Heparin sodium 5000 IU/ml 1ml |
| Ipratropium bromide + Fenoterol 0.25 mg + 05 mg/ml 20 ml | Clopidogrel 75 mg |
| Budesonide 0.5 mg/ml 2ml nebula | Acetylsalicylic acid 300 mg |
| Aminophylline 24 mg/ml 10ml | Etamsylate 125 mg/ml 2ml |
| Pyridoxine 50 mg/ml 1 ml | Alteplase 50 mg |
| Clonidine 0.1 mg/ml 1ml | Glycine 100 mg |
| Moxonidine 0.4 mg | Inosine+Nicotinamide+Riboflavin+Succinic acid 100mg/ml 10ml |
| Urapidil 5mg/ml 5 ml | Metoclopramide 5mg/ml 2ml |
| Nifedipine 10 mg | Ondansetron 8mg |
| Captopril 25mg | Potassium and magnesium aspartate 250ml |
| Enalapril 10 mg | Water for injections 5ml |
| Prednisolone 30mg/ml 1ml | Sodium thiopental 1000 mg |
| Insulin lispro 100 IU/ml 3ml | Propofol 10mg/ml 20ml |
| Hydrocortisone 100 mg 2 ml | Pipecuronium bromide 4 mg |
| Oxytocin 5 IU/ml 1 ml | Thiamine 50mg/ml 1ml |
| Betamethasone 2 mg+5 mg/ml 1 ml | Ascorbic acid 50mg/ml 2ml |
| Dexamethasone 4 mg/ml 1ml | Thioctic acid 300 mg |
| Dextran 60 mg/ml 400ml | Sodium bicarbonate 5% 200ml |
| Hydroxyethyl starch 6% 250ml | Ethylmethylhydroxypyridine succinate 50mg/ml 5ml |
| Hydroxyethyl starch 10% 250ml | Carboxim 150mg/ml 1ml |
| Dextrose 10% 500ml | Flumazenil 0.1 mg/ml 5 ml |
| Dextrose 5% 250ml | Tranexamic acid 50mg/ml 5ml |
| Dextrose 40% 10ml | Haloperidol 5mg/ml 1ml |
What to do if you are alone at home?
When a person is at home himself, it is not surprising that he is at a loss. It is important to take your medicine and open the front door. After this you call an ambulance. If you lose consciousness, doctors will be able to get into the house. The arriving team usually administers Dibazol, they use diuretics, and in case of significant tachycardia, beta blockers help. This is Inderal, or Rausedil and Obzidan.
You should definitely put Nifedipine or an analogue of Corinfar under your tongue. If the GC turns out to be complicated, then further measures are taken in the hospital. Sometimes ventricular failure occurs. If coronary insufficiency develops, the patient is placed in intensive care, where they try to relieve the pain. One of the most serious complications can be called a heart attack. This pathological condition requires resuscitation. It is necessary that the person is taken to the hospital as quickly as possible. This gives a chance to save the patient and minimize complications and their risks.
Medicines for crisis
When a hypertensive crisis occurs, there is a certain standard, and specific groups of drugs are used that reduce blood pressure to normal values. You must understand that the drop in pressure must certainly be slow and usually doctors recommend that if the numbers are not too high, take another tablet of the drug that you take all the time. Too much use of Captopril and other drugs can sharply lower blood pressure to the point of fainting and collapse.
So, let's look at some groups of drugs. Anaprilin, as well as Metoprolol and Inderal, Atenolol and similar beta blockers help relieve increased heart rate and allow blood vessels to dilate. ACE inhibitors are also very important, they lower blood pressure. This group includes Enap, Enam.
Clonidine is used with great caution. It lowers blood pressure too sharply. For arrhythmia, the blockers Normodipin and Cordipine, which block calcium channels, are usually prescribed. The accumulated fluid is removed with the help of diuretics. Lasix and Furosemide are usually used. If assistance is provided on time and of high quality, then the prognosis will be quite favorable. Death can occur with developed pulmonary edema, heart failure or stroke.
To prevent such acute situations, it is important to keep your blood pressure levels under control at all times, take medications prescribed by your doctor on a regular basis, and follow the advice of your cardiologist. It is very important to move, but not to overload yourself with physical activity. It is necessary to exclude alcohol and smoking, salt, fatty foods, animal fats, which lead to atherosclerosis. If you have heart disease, high cholesterol, or diabetes, be sure to monitor your condition and take treatment. Remember that a dangerous situation can develop quickly. And if you have a crisis, you cannot always assess for yourself how dangerous it is, so call an ambulance. Doctors will examine you, assess the threats and take all necessary measures.