- Google+
Take an online test (exam) on this topic...
The PQ interval is the distance (time interval) from the beginning of the P wave to the beginning of the q wave (or the R wave, if there is no q wave - then we are talking about the PR interval). In the figure, the PQ interval is indicated by the red area - it corresponds to the time of passage of excitation through the atria and atrioventricular node to the ventricular myocardium. The PQ interval (PR) varies with age; body weight; heart rate frequency.
Normally, the PQ interval is 0.12-0.18 (up to 0.2) seconds (6-9 cells). With age, the PQ interval lengthens:
at the age of up to 14 years, the maximum PQ interval is up to 0.16 s; at the age of 14 to 17 years - 0.18 s; over the age of 17 years - 0.2 s. As the heart rate increases, the PQ interval shortens; With bradycardia, the PQ interval lengthens to 0.21-0.22 s. In the chest leads, the duration of the PQ interval may differ from the readings in the limb leads by up to 0.04 s (2 cells). To measure the PQ interval, select the lead where the P wave and the QRS complex are well defined (usually this is standard lead II). If the initial part of the P wave is isoelectric, then when measuring the PQ interval there will be an error downward from its true values. If the initial segment of the QRS complex is isoelectric, then when measuring the PQ interval there will be an error upward from its true values. Errors can be avoided if the measurement is carried out on a multichannel electrocardiograph.
The PQ interval can be divided into two parts:
P wave (green sector); PQ segment (blue sector) - from the end of the P wave to the beginning of the QRS complex.
The ratio of the duration of the P wave to the duration of the PQ segment is called the Macruse index . Normally, the Makruse index is 1.1-1.6. This index is used in the diagnosis of atrial hypertrophy.
Take an online test (exam) on this topic...
ATTENTION! The information presented on the website DIABET-GIPERTONIA.RU is for reference only. The site administration is not responsible for possible negative consequences if you take any medications or procedures without a doctor’s prescription!
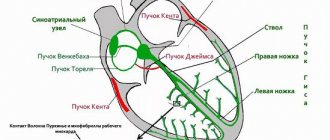
The feeling of rapid heartbeat, or tachycardia, accompanied by a very high heart rate (more than 100 per minute), can be caused by many diseases that lead to arrhythmia. Often such symptoms, together with specific changes in the electrocardiogram, are based on the anatomical features of the conduction system of the heart, which is responsible for the correct heart rhythm. The combination of such features constitutes clinical syndromes, generalized by the concept of shortening of the PQ interval.
So, shortened PQ interval syndrome is a group of electrocardiological symptoms, the basis of which is a decrease in the time it takes electrical excitation to reach the ventricles from the atria through the atrioventricular connection. This group includes Wolf-Parkinson-White syndrome (WPV syndrome), as well as Clerc-Levy-Cristesco syndrome (CLC syndrome). These syndromes can occur at any age, even in the neonatal period, regardless of gender differences.
Indications for ECG
ECG is a non-invasive and painless research method that has no contraindications. The procedure is carried out on a planned or emergency basis.
Planned electrocardiography is prescribed:
- before surgical interventions;
- during pregnancy;
- during preventive examinations of the population;
Scheduled electrocardiography is prescribed in certain cases.
Also, periodic electrocardiography must be performed for persons with health conditions or occupational hazards:
- in the presence of atherosclerotic plaques;
- hypertension;
- elevated blood cholesterol levels;
Emergency electrocardiography is performed to identify pathological processes in the heart, some of which require immediate intervention.
An emergency ECG is prescribed for:
- sharp pain localized behind the sternum or in the upper abdomen;
- sudden onset of shortness of breath;
- heart murmurs identified during initial diagnosis;
- with discomfort in the heart.
What does an electrocardiogram consist of?
To understand the elements that make up the electrocardiogram, it is necessary to delve into the processes occurring in the heart before and during its contraction.
For the heart muscle to contract, an electrical impulse must first travel through it. During the propagation of this impulse, the muscle becomes a source of electrical current, which is conducted into the surrounding tissues and onto the surface of the body.
If electrodes are placed on both sides of the heart, the potential difference that occurs during the propagation of excitation can be recorded and displayed on paper. The resulting diagram will be called an electrocardiogram.
In practice, three methods of placing electrodes, called standard leads, are used:
- In the first lead, the electrode on the left hand is positive, and on the right hand it is negative.
- In the second lead, positive electrodes are installed on the left leg and negative electrodes on the right arm.
- In the third lead, the negative electrode is located on the left arm, and the positive electrode on the right leg.
When the electrical phenomena occurring in the heart are recorded over a period of time, an image is obtained consisting of teeth, segments and intervals. The waves represent a set of positive and negative peaks and reflect the processes of changing the potential difference between the electrodes.
There are waves P, Q, R, S, T, they provide the following information:
- The P wave occurs during atrial depolarization. Depolarization is a process that precedes muscle contraction. Normally, in the second standard lead this wave is positive.
- The QRS complex consists of two negative (Q and S) and one positive (R) waves. They correspond to the process of propagation of ventricular depolarization.
- The T wave occurs when the resting potential of the cardiomyocytes (heart cells) of the ventricles returns to its original level and repolarization occurs. Normally, in the second standard lead the T wave is positive.
Segments are straight line segments connecting adjacent teeth to each other:
- The PQ segment occurs due to a delay in the impulse in the atrioventricular node; its duration can be used to judge the functioning of the conduction system of the heart.
- The ST segment corresponds to the time during which both ventricles are in a depolarized (excited) state.
The intervals consist of a tooth or several teeth and a segment:
- The value of the PQ interval is defined as the distance between the beginning of the P wave and the QRS complex. It displays the time period spent on the propagation of excitation from the atrium to the ventricles.
- The values of the QRS complexes on cardiograms are represented by the intervals from the Q wave to the S wave, and corresponds to the process of ventricular excitation.
- The QT interval refers to the distance from the starting point of the Q wave to the end of the T wave. It reflects the depolarization and repolarization of the ventricles.
Treatment
Treatment methods are conservative and surgical. Before resorting to radical measures, drug correction is carried out.
Two pharmaceutical groups are used:
- Beta blockers. Mainly Anaprilin, less often others. Allows you to stop pathological excitation in the tissues of the heart.
- Antiarrhythmic. Procainamide, Propafenone. With great care so as not to make things worse.
Attention:
Calcium antagonists and ATP agents should not be used. So as not to provoke cardiac arrest.
As part of urgent symptomatic care, doctors resort to electrocardioversion. Passing current for a fraction of a second to restore normal heart rate.
This is an emergency measure aimed at saving the patient’s life and improving well-being.
Surgery is required in extreme cases. That is, almost always, oddly enough. It is impossible to correct an organic disorder with tablets.
The method is identical - radiofrequency ablation. This is a minimally invasive intervention, it consists of introducing a special miniature emitter into the cardiac structures and destroying the abnormal conduction pathway using a bloodless method.
The procedure is painless and causes virtually no discomfort.
In the future, everything should return to normal without any additional measures. Unless the disease provokes other anatomical changes in the heart and brain.
How to decipher an ECG
Decoding the electrocardiogram includes assessment of intervals, waves and segments.
The duration of the intervals, the amplitude of the waves, their frequency and rhythm have strict normal limits, and deviation from these norms can indicate many pathologies. It is important to understand that only a doctor can diagnose a pathological change in an electrocardiogram, because the cardiogram readings can change.
The PQ interval on the ECG, the norm of which also has fairly strict values, can be differentiated according to the age categories of patients. Children's norms for this indicator, for example, are lower than those of adults. This factor is due to the peculiarities of children's physiology and the faster conduction of intracardiac excitation impulses.
ECG analysis
In the process of analyzing the electrocardiogram, the doctor receives information about the heart rate (HR), the main rhythm, the presence or absence of extraordinary contractions and disturbances in the conduction of the electrical impulse.
The patient should understand that many factors can influence the result of the electrocardiogram. Any stress factors, be it emotional overexcitation, physical activity or a cup of coffee before the examination, can significantly distort the real picture. Ideally, at the time of the examination, the patient should be well-rested and in a calm, non-excited state.
In order for the research results to be reliable, a number of rules should be followed:
- avoiding strong tea, coffee and energy drinks several hours before the examination;
- lack of physical and emotional stress;
- no excessive load on the gastrointestinal tract. If the procedure is scheduled for the morning, you should postpone a hearty breakfast. If the procedure is performed during the day, it is better not to eat a few hours before the ECG;
- do not worry directly during the examination. The ECG procedure is absolutely painless and harmless, and excessive emotional stress can affect the reliability of the results;
- Smoking and drinking alcohol are prohibited several hours before the examination;
- You should not use medications that affect the cardiovascular system.
A competent specialist, having seen deviations from the norm in ECG indicators, will make sure that all of the above rules are followed, and only after that will make a final diagnosis.
What is PQ interval
The PQ interval is the distance from the beginning of the positive P wave to the beginning of the negative Q wave (or to the positive R wave if the Q wave is not pronounced or absent). This interval reflects the process of impulse conduction from the atria to the ventricles through the atrioventricular node.
This interval reflects the time during which the electrical impulse spreads from the place where it was generated (atrium) to the ventricles, which, thanks to this “signal,” contract and push a portion of blood into the great vessels.
The atrioventricular node serves as an intermediate point through which the electrical impulse passes. Normally, it is delayed at this intermediate point in order to prevent simultaneous contraction of the atria and ventricles.
Normal PQ interval in children and adults
The PQ interval on the ECG (the norm for adults is 0.12-0.20 s) should vary strictly within a certain range. Anything that goes beyond this is pathological.
PQ interval on ECG (normal for adults and children)
However, it should be understood that the value of this parameter depends on the heart rate (the higher the heart rate, the faster the impulse propagates). Therefore, it is more correct to evaluate the nature and state of the atrioventricular connection as the ratio of the duration of the PQ interval to the duration of the entire cardiac systole (PT).
ECG in children has its own peculiarities. Differences from the electrocardiogram in adults are most pronounced at an early age; after 13-14 years, its characteristics are increasingly closer to the standard norm. The PQ interval is shorter in children, which is due to a higher heart rate compared to adults.
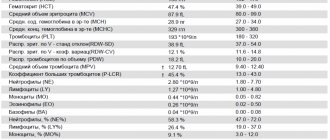
The PQ interval and heart rate values when deciphering an ECG for children are normally based on the following indicators:
| Age (years) | Heart rate (beats per minute) | Interval (s) |
| 0-1 | 120-140 | 0,09-0,12 |
| 1-2 | 110-130 | 0,10-0,12 |
| 3-4 | 90-110 | 0,11-0,13 |
| 5-7 | 80-105 | 0,12-0,14 |
| 8-11 | 75-95 | 0,12-0,14 |
| 12-15 | 70-90 | 0,12-0,16 |
Causes
Factors in the development of a shortened interval are always intrauterine. That is, the disorder or predisposition to it occurs during the mother’s pregnancy.
There are already two options here:
- The first is a spontaneous violation in the 1st trimester. When the cardiovascular system is formed. This is the main reason.
- The second is chromosomal disorders, genetic mutations (extremely rare).
Then everything depends on the case. An anatomical defect does not always manifest itself immediately after birth.
A child can live for years and seem healthy until a certain point. As long as the body copes, everything is fine. And then a trigger factor is required that will lead to dysfunction and tip the scale in the other direction.
Among them:
- Drinking alcohol, smoking, drug addiction. Cocaine, heroin, and, to a lesser extent, amphetamine are particularly dangerous in this regard.
- Constant use of caffeine.
- Insufficient sleep.
- Frequent stress, physical overload. That is, moments that provoke an increase in the synthesis of cortisol, adrenaline, and adrenal hormones.
- Using medications without a doctor's prescription. Especially anti-inflammatory drugs.
- A history of hypertension, diabetes mellitus, and endocrine disorders.
The list is incomplete. There is also an increased risk in the early years (up to 3 years), during puberty and in later life. It is necessary to carefully monitor patients from risk groups.
PQ interval pathologies
Changes in the PQ interval indicate pathologies of the cardiac conduction system. This interval can be either shortened or lengthened. In some cases, there is dissociation of the P wave from the QRS complex.
A shortening of the interval indicates a faster than normal conduction of excitation from the atria to the ventricles. This can be dangerous due to the development of tachycardia attacks.
Lengthening the interval, on the contrary, indicates difficulty in conducting excitation between the atria and ventricles. These pathologies are called atrioventricular conduction blocks. They are classified as both physiological and pathological.
Pathologies of the PQ interval are fraught with the development of tachycardia
A shortening of the interval may indicate the presence of premature ventricular excitation syndrome. This syndrome is associated with the presence of additional (abnormal) pathways through which excitation from the atria reaches the ventricles. As a result, the impulse spreads without physiological delay, faster than necessary.
There are two types of this syndrome: CLC syndrome and WPW syndrome ; they can be differentiated from each other by the characteristics of the QRS complexes. You can recognize accelerated impulse conduction on an ECG by measuring the duration of the PQ interval. Its normal values should be less than 0.11 seconds.
The PQ interval on the ECG (the norm for children is less than for adults) during diagnosis depends on the age of the patients. With this pathology, the QRS complex and the T wave remain unchanged.
The danger of this phenomenon is the possibility of developing arrhythmias (paroxysmal tachycardias). During the course of the disease without attacks of tachycardia, the patient may not realize for a long time that there are additional pathways in the heart.
An increase in the interval may occur in cases of atrioventricular blockade. There are partial (types 1 and 2) and complete (type 3) blockades. The cause of blockades can be functional or organic factors.
Functional reasons include the use of certain medications that reduce intracardiac conduction and intense exercise. Examples of organic causes are myocardial infarction, infectious diseases of the heart muscle, myocardial ischemia and heart defects.
Intense sports may cause the development of PQ interval pathologies
The PQ interval on the ECG (the norm against the background of partial blockades is violated) in the first type increases, since the conduction of excitation is slowed down, but all impulses from the atria reach the ventricles. This type of blockade is physiological and is quite often observed in young patients and athletes.
Often this type of blockade has no clinical manifestations and does not affect people’s daily lives. On the ECG, this type of blockade manifests itself as an increase in the PQ interval (duration more than 0.2 s).
If a blockade of this type is detected, it is advisable to undergo additional examination to exclude the possibility of concomitant pathologies. Treatment is not prescribed until the factors that trigger the development of the pathology are identified.
PQ interval on ECG - pathologies
In the second type of disorder, not all impulses from the atria reach the ventricles. The ECG recording clearly shows that there are no QRS complexes following some P waves. There are two variants of the manifestation of the second type of blockade: Mobitz I and Mobitz II.
Flow options
In all cases, several variants of the clinical course of the disease are described.
- Hidden or asymptomatic type. Occurs in 40% of patients. It is not necessary that pathology always moves in this way. Transformation into other forms is possible. Usually, as the disorder progresses and the condition decompensates.
- Light type. Paroxysms develop once every month or two, or less often. Lasts from 5 to 15 minutes, goes away completely without any traces, on its own.
- Moderate in severity. Episodes of varying frequency, not necessarily regular. Accompanied by a persistent increase in the number of heart contractions and poor health. Duration is 2-4 hours, sometimes longer. Independent complete regression is almost never observed; the use of drugs or the use of electrocardioversion is required to interrupt the paroxysm.
- A severe form of shortening of the PQ interval is accompanied by a pronounced disturbance: the attack continues indefinitely. Additionally, ventricular fibrillation, or atrial flutter, is detected. The probability of death is maximum; urgent hospitalization is required.
The clinical picture is almost always the same. But it is nonspecific, which does not allow doctors to say unambiguously about the origin.
Mobitz I
This type of blockade of the second type can be physiological for young people and athletes. On the ECG it appears as an increase in the PQ interval with each contraction. The interval increases until the atrial impulse is blocked (this is shown on the cardiogram as the absence of the QRS complex).
Also, as with the first type of blockade, patients may not suspect the presence of disturbances in the conduction system of the heart and may not experience any clinically manifested symptoms.
If a second-degree block of Mobitz type I is detected, a re-examination should be carried out , including 24-hour heart rate monitoring and a repeat electrocardiogram. Treatment is prescribed after identifying the cause of the blockade.
Forecast
Determining the prognosis for patients with CLC syndrome is always difficult, since it is not possible to predict in advance the occurrence of certain rhythm disturbances, the frequency and conditions of their occurrence, as well as the occurrence of their complications.
According to statistics, the life expectancy of patients with short PQ syndrome is quite high, and paroxysmal rhythm disturbances most often occur in the form of supraventricular rather than ventricular tachycardias. However, in patients with underlying cardiac pathology, the risk of sudden cardiac death remains quite high.
The prognosis for the phenomenon of shortened PQ remains favorable, and the quality and life expectancy of such patients do not suffer.
Mobitz II
This type is always pathological. The pulse travel time is constant, but the pulses are periodically blocked. This is reflected as the absence of some QRS complexes. Most often, a violation of the passage occurs on every third (3:1) or fourth (4:1) excitation. In severe cases, the blockade occurs every second contraction (2:1).
The condition of patients with this pathology can be very different. Some patients note a sharp deterioration in their condition, darkening of the eyes, coinciding with the loss of the QRS complex. A number of patients may not even be aware of the presence of these problems.
The severity of the blockade and the risk of transition to a complete blockade (third degree blockade) depends on the causes of the development of the pathology. Treatment is also prescribed based on the etiology of the disease. Blockade of the third type is characterized by complete disruption of impulse conduction. On the cardiogram, this appears as a separation between the P waves and the QRS complexes.
Cardiac activity in such patients is maintained by the rhythm generated by the ventricles. Depending on the cause of the development of third-degree blockade, treatment methods can be either medicinal or surgical (implantation of a pacemaker). If this type of block is congenital, most patients do not require a pacemaker.
Disturbances in the conduction system of the heart can cause sudden cardiac arrest and death. These disorders can be either congenital or acquired.
In the case of acquired diseases, early diagnosis and correctly prescribed treatment can affect a favorable outcome of the disease. That is why an ECG should be performed periodically to make sure that its indicators (in particular the PQ interval) are normal.
What is the difference between a syndrome and a phenomenon?
Many patients, having seen the concepts of the phenomenon or CLC syndrome in the ECG conclusion, may be puzzled which of these diagnoses is worse. The CLC phenomenon, subject to a correct lifestyle and regular monitoring by a cardiologist, does not pose a great danger to health, since the phenomenon is the presence of signs of PQ shortening on the cardiogram, but without clinical manifestations of paroxysmal tachycardia.
CLC syndrome, in turn, is an ECG criterion accompanied by paroxysmal tachycardias, most often supraventricular, and can cause sudden cardiac death (in relatively rare cases). Typically, patients with short PQ syndrome develop supraventricular tachycardia, which can be quite successfully stopped at the stage of emergency medical care.