What is leukemia in children
Statistics show that leukemia is the most common cancer pathology in childhood (30%).
Most often, blood cancer is diagnosed in children aged 2 to 5 years. Classification of blood leukemia in children
Depending on the duration of the disease, there are:
- acute leukemia (up to two years);
- chronic leukemia (more than two years).
97% of cases in children are acute. A special type of it is congenital leukemia (observed in newborns or children in the first three months of life).
According to the criterion of morphological characteristics of tumor cells, acute leukemias are conventionally divided into:
1. Lymphoblastic. They arise as a result of the uncontrolled proliferation of immature lymphocytes (lymphoblasts). There are three types:
- with small lymphoblasts (L1) – the most common type in children;
- with polymorphic large lymphoblasts (L2);
- with polymorphic large lymphoblasts with vacuolization of the cytoplasm (L3).
According to antigenic markers, acute lymphoblastic leukemias are divided into:
- B-cell (1 to 3%);
- T-cell (15 to 25%);
- O-cell (70 to 80%).
2. Non-lymphoblastic (myeloblastic). Depending on the dominance of certain blast cells, types of acute myeloblastic leukemia are distinguished:
- undifferentiated (M0) – it is not possible to isolate a specific lineage of hematopoiesis modified by the tumor,
- poorly differentiated myeloblastic (M1);
- well-differentiated myeloblastic (M2);
- promyelocytic (M3);
- myelomonoblastic (M4);
- monoblastic (M5);
- erythromyelosis (M6);
- megakaryocytic (M7);
- eosinophilic (M8).
The clinical course of acute leukemia in childhood is described in three stages:
- Acute form (from the appearance of the first symptoms to a noticeable improvement in clinical and hematological parameters as a result of therapy).
- Incomplete/complete remission. In the first case, normalization of clinical parameters and hemogram is observed, the number of immature lymphocytes in the bone marrow puncture does not exceed 20%. With complete remission, this indicator is equal to up to 5% blasts.
- Relapse of the disease. Against the background of hematological well-being, extramedullary foci of leukemic infiltration are detected in the testicles, lungs, nervous system, etc.
Leukemia is a malignant disease in which the process of hematopoiesis in the bone marrow is disrupted. As a result, a large number of immature leukocytes enter the blood, which cannot cope with their main function - protecting the body from infections. Gradually, they displace healthy blood cells and also penetrate various organs, disrupting their functioning.
Blood cancer is one of the most common cancers that occurs in both children and adults. The prognosis of the disease depends on many factors: the type of leukemia, the patient’s age, and concomitant diseases. Over the past decades, methods for effective treatment of leukemia have been developed and are constantly being improved.
Synonyms Russian
Leukemia, leukemia, blood cancer.
English synonyms
Leukemia, leucosis, bloodcancer.
Symptoms
Symptoms of myleukemia can develop acutely or gradually. They are nonspecific, depend on the type of leukemia, and in the initial stages may resemble the flu or other infectious disease.
Symptoms of leukemia are:
- frequent infectious diseases;
- fever;
- weakness, malaise;
- frequent prolonged bleeding;
- hematomas, hemorrhages on the skin and mucous membranes;
- stomach ache;
- swollen lymph nodes;
- causeless weight loss;
- headache.
General information about the disease
All blood cells - leukocytes, erythrocytes, platelets - are formed in the bone marrow - a specific hematopoietic tissue that is located in the pelvic bones, sternum, vertebrae, ribs, and long tubular bones. It contains stem cells, which give rise to all blood cells. During the process of division, lymphoid and myeloid stem cells are first formed. Lymphoblasts are formed from lymphoid stem cells, and myeloblasts are formed from myeloid stem cells, as well as precursors of erythrocytes and platelets. Leukocytes are produced from lymphoblasts and myeloblasts. Blasts differ from mature leukocytes in structure and function and must undergo a series of successive divisions during which increasingly specialized precursor cells are formed. After the last division, mature, functional blood cells are formed from the precursors. Thus, lymphocytes (a type of leukocyte) are formed from lymphoid stem cells, and erythrocytes, platelets and other types of leukocytes (neutrophils, basophils, eosinophils and monocytes) are formed from myeloid stem cells. These are mature blood cells capable of performing their specific functions: red blood cells deliver oxygen to tissues, platelets provide blood clotting, and leukocytes provide protection from infections. After completing their task, the cells die.
The entire process of division, death and maturation of blood cells is embedded in their DNA. When it is damaged, the process of growth and division of blood cells, mainly leukocytes, is disrupted. A large number of immature leukocytes enter the blood, unable to perform their function, and as a result, the body cannot cope with infections. Immature cells divide very actively, live longer, gradually displacing other blood cells - red blood cells and platelets. This leads to anemia, weakness, frequent prolonged bleeding, and hemorrhages. Immature leukocytes can also penetrate other organs, disrupting their function - the liver, spleen, lymph nodes, and brain. As a result, the patient complains of pain in the stomach and head, refuses to eat, and loses weight.
Depending on what type of leukocytes is involved in the pathological process and how quickly the disease develops, the following types of leukemia are distinguished.
- Acute lymphoblastic leukemia is a rapidly developing disease in which more than 20% of lymphoblasts appear in the blood and bone marrow. This is the most common type of leukemia and occurs in children under 6 years of age, although adults are also susceptible.
- Chronic lymphocytic leukemia progresses slowly and is characterized by an excessive amount of mature small round lymphocytes in the blood and bone marrow, which can penetrate the lymph nodes, liver, and spleen. This type of leukemia is typical for people over 55-60 years of age.
- Acute myeloblastic leukemia - with it, more than 20% of myeloblasts are found in the blood and bone marrow, which continuously divide and can penetrate other organs. Acute myeloblastic leukemia most often affects people over 60 years of age, but it also occurs in children under 15 years of age.
- Chronic myelocytic leukemia, in which the DNA of the myeloid stem cell is damaged. As a result, immature malignant cells appear in the blood and bone marrow along with normal cells. Often the disease develops unnoticed, without any symptoms. Chronic myeloid leukemia can occur at any age, but people aged 55-60 years are most susceptible to it.
Thus, in acute leukemia, a large number of immature, useless leukocytes accumulate in the bone marrow and blood, which requires immediate treatment. In chronic leukemia, the disease begins gradually; more specialized cells enter the blood and are able to perform their function for some time. They can go on for years without showing themselves.
Who is at risk?
- Smokers.
- Those exposed to radioactive radiation, including during radiation therapy and frequent x-ray examinations
- Prolonged contact with chemicals such as benzene or formaldehyde.
- Having undergone chemotherapy.
- Suffering from myelodysplastic syndrome, that is, diseases in which the bone marrow does not produce enough normal blood cells.
- People with Down syndrome.
- People whose relatives suffered from leukemia.
- Infected with T-cell virus type 1, which causes leukemia.
Diagnostics
Basic methods for diagnosing leukemia
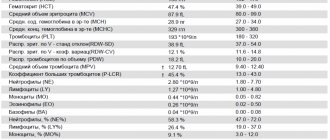
- General blood test (without leukocyte formula and ESR) with leukocyte formula - this study gives the doctor information about the quantity, ratio and degree of maturity of blood elements.
- Leukocytes. The white blood cell count in leukemia can be very high. However, there are leukopenic forms of leukemia, in which the number of leukocytes is sharply reduced due to inhibition of normal hematopoiesis and the predominance of blasts in the blood and bone marrow.
- Platelets. Usually the platelet count is low, but in some types of chronic myeloid leukemia it is elevated.
- Hemoglobin. The level of hemoglobin, which is part of red blood cells, may be reduced.
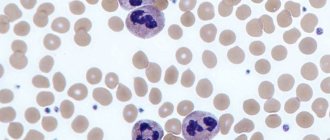
Changes in the level of leukocytes, red blood cells, platelets, the appearance of leukocytes, and the degree of their maturity allow the doctor to suspect leukemia in the patient. Similar changes in the ratio of blood cells are possible in other diseases - infections, immunodeficiency states, poisoning with toxic substances - but in these cases there are no blasts in the blood - the precursors of leukocytes. Blasts have characteristic features that are clearly visible under a microscope. If they are found in the blood, there is a high probability that the patient has one of the types of leukemia, so further examination is necessary.
- The leukocyte formula is the percentage of different types of leukocytes in the blood. Depending on the type of leukemia, different types of leukocytes predominate. For example, in chronic myeloid leukemia, the level of neutrophils usually increases, basophils and eosinophils may be increased, and their immature forms predominate. And in chronic lymphocytic leukemia, the majority of blood cells are lymphocytes.
- Bone marrow biopsy is the removal of a sample of bone marrow from the breastbone or pelvis using a fine needle and is performed after anesthesia. The presence of leukemia cells in the patient's bone marrow is then determined under a microscope.
Additionally, the doctor may prescribe:
- Spinal puncture to detect leukemia cells in the cerebrospinal fluid that bathes the spinal cord and brain. A sample of cerebrospinal fluid is taken using a thin needle, which is inserted between the 3rd and 4th lumbar vertebrae after local anesthesia.
- Chest X-ray - may show enlarged lymph nodes.
- Cytogenetic study of blood cells - in difficult cases, an analysis of the chromosomes of blood cells is carried out and thus the type of leukemia is determined.
Treatment
The treatment strategy for leukemia is determined by the type of disease, the patient’s age and his general condition. It is carried out in specialized hematology departments of hospitals. Treatment for acute leukemia should begin as early as possible, although in the case of chronic leukemia, if the disease progresses slowly and the patient is feeling well, therapy may be delayed.
There are several treatments for leukemia.
- Chemotherapy is the use of special drugs that destroy leukemia cells or prevent them from dividing.
- Radiation therapy is the destruction of leukemia cells using ionizing radiation.
- Biological therapy is the use of drugs that work similarly to specific proteins produced by the immune system to fight cancer.
- Bone marrow transplant - normal bone marrow cells are transplanted into the patient from a suitable donor. A course of chemotherapy or radiation therapy in high doses is first administered to destroy all pathological cells in the body.
The prognosis of the disease depends on the type of leukemia. With acute lymphoblastic leukemia, more than 95% of patients are cured, with acute myeloblastic leukemia - about 75%. In chronic leukemia, the prognosis is influenced by the stage of the disease at which treatment was started. This type of leukemia progresses slowly, and the average life expectancy for patients is 10-20 years.
Prevention
There is no specific prevention of leukemia. For timely diagnosis of the disease, it is necessary to undergo regular preventive medical examinations.
Recommended tests
- General blood analysis
- Leukocyte formula
- Cytological examination of punctates, scrapings of other organs and tissues
Causes of leukemia in children
It has been proven that acute leukemia is a “clonal” pathology. As a result of the mutation process occurring in the hematopoietic cell, its differentiation fails at the stage of immature forms (blasts) with their further growth (proliferation). A malignant tumor forms, replacing the bone marrow and preventing normal hematopoiesis. Blasts begin to leave the bone marrow, enter the blood and spread throughout the body. Leukemic infiltration of organs and tissues develops.
The origin of tumor cells from one mutated cell is proven by the fact that they all have identical morphological, biochemical and immunological characteristics. But what are the causes of leukemia in children and where does the mutant cell come from, scientists have not fully figured out.
It is believed that the following factors can trigger a pathological process in a child’s body:
- hereditary predisposition (if one of your relatives had leukemia, the disease may manifest itself in subsequent generations);
- genetic disorders (Down syndrome, Li-Fraumeni syndrome, neurofibromatosis, etc.);
- radioactive effects on the child’s body (man-made accidents, atomic explosions);
- increased solar insolation caused by ozone holes;
- poor environmental conditions;
- passive smoking (the child constantly inhales air containing smoking products);
- disruption of DNA structure caused by viral infections.
Causes and risk factors
The etiological factors that inevitably become the “trigger” for malignant cell mutation have not yet been precisely established. However, the risks of developing acute leukemia increase significantly if:
- radiation exposure to which a person is exposed;
- infection with certain viruses that suppress the immune system (Epstein-Barr disease, T-lymphotropic virus, etc.);
- unfavorable heredity;
- smoking tobacco;
- prolonged exposure to certain chemical compounds, including medications;
- stress, depression;
- environmental pollution.
Symptoms of leukemia in children
In most cases, the first signs of leukemia in children are veiled. The child sleeps poorly, gets tired quickly, does not want to eat, and for unknown reasons his body temperature rises. Parents mistakenly associate such symptoms with viral infections and colds. Sometimes the first sign of leukemia in children is:
- hemorrhagic syndrome (bleeding into the mucous membranes and skin);
- sudden general intoxication of the body (occurs with weakness, sweating, fever, anorexia, malnutrition, vomiting, nausea).
To recognize leukemia in a child, you should pay attention to:
- the color of the skin, mucous membranes - they become almost white, acquire a jaundiced/earthy tint (photos of patients with leukemia always show very pale children);
- condition of the mucous membranes – due to infiltration, tonsillitis, stomatitis, and gingivitis occur;
- the size of the lymph nodes - they increase, lymphadenopathy develops.
Symptoms of acute leukemia also include:
- sialadenopathy (pathological changes in the salivary glands);
- hepatosplenomegaly (simultaneous enlargement of the liver and spleen);
- hematuria (blood in the urine);
- uterine, gastrointestinal, pulmonary and nasal bleeding;
- hemorrhages into the joint cavity.
An invariable companion to acute leukemia in childhood is anemic syndrome. Its severity is determined by the degree of proliferation of blast cells in the bone marrow.
Symptoms of acute lymphoblastic leukemia can also be of a cardiac nature - arrhythmia, tachycardia, diffuse changes in the myocardium, expansion of the borders of the heart, and a decrease in ejection fraction are diagnosed.
Signs of an immunodeficiency state in leukemia are the addition of infectious and inflammatory processes to the underlying disease. Thus, death is often caused by pneumonia and sepsis.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
About relapses and prognosis after treatment
As a rule, a relapse of this particular disease, if it exists, manifests itself directly during the course of treatment or immediately after its completion. After remission has been achieved and its consolidation (consolidation) has been carried out, after five years relapses are an extremely rare occurrence. After seven years, we can safely talk about a complete recovery.
Modern treatment methods suggest a favorable prognosis for acute lymphoblastic leukemia in children in 60-80% of cases. The indicator is influenced by an adequate therapy program (including the capabilities of a specialized clinic) and the general condition of the body.
How to identify leukemia in a child - diagnosis
Suspicions of leukemia in a child usually arise from a pediatrician. Further examination and treatment of the little patient is carried out by an oncohematologist. To make a diagnosis, it is necessary to carry out basic laboratory methods:
- bone marrow examination;
- peripheral blood examination.
A blood test for leukemia in children shows:
- anemia;
- reticulocytopenia (low content of young red blood cells);
- thrombocytopenia (low platelet count);
- high ESR;
- blastemia (release of blast cells into the peripheral blood);
- leukopenia (low white blood cell count);
- complete absence of eosinophils and basophils.
A classic symptom of leukemia in children is the phenomenon of “leukemic failure,” which is characterized by the absence of intermediate forms between mature and blast cells.
Mandatory procedures in the further diagnosis of leukemia:
- Sternal puncture. The procedure is performed under local anesthesia and is aimed at assessing the state of bone marrow hematopoiesis. The patient lies on his back. A Kassirsky needle with a special safety shield that prevents damage to the mediastinal organs is inserted at the level of 2-3 ribs in the midline.
- Myelogram study. To collect diagnostic material, a puncture of the sternum is performed at the level of the 2-3 intercostal space. The doctor uses a needle with a safety lock, so damage to internal organs is excluded. If the child is under two years old, a bone marrow sample is obtained by puncturing the tibia (the puncture is made in the upper third along the inner surface).
Additionally, when diagnosing leukemia:
- immunological, cytochemical and cytogenetic studies are carried out;
- consultations with an ophthalmologist and neurologist are prescribed;
- a lumbar puncture is performed (by inserting a puncture needle into the subarachnoid space of the spinal cord, the doctor takes cerebrospinal fluid (CSF) for further study);
- X-rays of the skull and ophthalmoscopy (examination of eye structures) are performed;
- Cerebrospinal fluid is examined.
According to indications, the following is performed: ultrasound of the liver, spleen, lymph nodes, salivary glands, scrotum in boys. In order to identify metastases, the child is prescribed a computed tomography scan.
During diagnostic procedures, it is important to differentiate leukemia from whooping cough, tuberculosis, cytomegalovirus infection, infectious mononucleosis, and sepsis. Full diagnostics can be performed in any modern hematology clinic
.
Diagnostics
A patient with symptoms resembling acute leukemia is prescribed:
- blood tests - general, biochemical, coagulogram;
- removal of bone marrow from the ilium or sternum, followed by cytochemical analysis, immunophenotyping, and morphological analysis of cells;
- puncture of bone marrow and cerebrospinal fluid for cytological and histological examination;
- instrumental studies of internal organs - ultrasound, radiography, CT, MRI to assess the extent of their damage by malignant cells;
- consultations with a neurologist, otolaryngologist, ophthalmologist and other specialists.
Treatment of leukemia in children
Children diagnosed with leukemia undergo inpatient treatment in specialized oncohematological institutions. To avoid infectious complications, each child is in an isolated box, where conditions are created that are as close to sterile as possible. A lot of attention is paid to nutrition - it must be well-balanced and complete.
Treatment of leukemia involves the simultaneous use of several drugs (polychemotherapy) and is aimed at destroying the leukemic clone. Treatment regimens followed by oncologists for lymphoblastic and myeloblastic acute leukemia are different. Their difference lies in the combination of chemotherapy drugs, optimal doses and methods of drug administration.
Stage-by-stage treatment of leukemia:
- First, everything necessary is done to achieve clinical and hematological remission.
- Then the results obtained are consolidated (consolidation stage).
- Afterwards, maintenance therapy and prevention/treatment of complications are carried out.
In addition to chemotherapy, immunotherapy can be performed, the essence of which is the introduction of:
- BCG vaccine (against tuberculosis);
- leukemia cells;
- interferons;
- smallpox vaccine;
- immune lymphocytes, etc.
Among the most promising methods of treating childhood leukemia that doctors resort to today are transplantation of umbilical cord blood, bone marrow, and stem cells.
To eliminate unpleasant symptoms of the disease, the following can be done:
- transfusion of platelet and red blood cells;
- antibiotic therapy;
- hemostatic therapy;
- detoxification measures.
Forecast
Whether leukemia can be completely cured depends on:
- age at which the disease occurred;
- the stage at which it was diagnosed;
- individual characteristics of the body;
- presence of concomitant diseases;
- functioning of the immune system.
The worst prognosis is expected for children who:
- fell ill between birth and 2 years and from 10 years;
- who were diagnosed with neuroleukemia at the time of diagnosis;
- who suffer from lymphadenopathy and hepatosplenomegaly.
The earlier treatment is started, the better results can be achieved. Stable remission and complete recovery can often be achieved in patients (especially girls) who suffer from lymphoblastic leukemia type L1 from 2 to 10 years of age.
Classification of CLL
Chronic leukemia is classified by stages and risk groups.
The stage of the disease is determined based on a clinical examination and blood test results:
- Stage A - hemoglobin level more than 100 g/l, platelets more than 100 × 109/l, and less than 3 areas of lymph nodes are affected.
- Stage B - hemoglobin level more than 100 g/l, platelets more than 100 × 10 9 / l, and more than 3 areas of lymph nodes are affected.
- Stage C hemoglobin level less than 100 g/L or platelet level less than 100 × 10 9 /L.
Classification by risk groups
For this classification, an international prognostic index was developed that takes into account the following parameters:
- TP53 mutation (17p).
- IGHV mutation.
- β2-microglobulin level >3.5 mg/l.
- Stage B/C.
- Age over 65 years.
Each of these parameters is assigned a certain number of points; when summed up, the patient is assigned to one of 4 risk groups:
- 0-1 point - group with a low risk of progression.
- 2-3 points - intermediate risk of progression.
- 4-6 points - high risk of progression.
- 7-10 points - a very high risk of progression.
Diet for leukemia
There is no special diet for leukemia. Nutrition must be nutritious, since the pathological process occurring in the body leads to a weakening of the immune system. In order for the bone marrow to produce healthy blood cells, it needs large quantities of protein, carbohydrates, fats, vitamins, micro- and macroelements. Therefore, a child’s daily diet should include fruits, berries and vegetables. Freshly squeezed juices from pomegranate, carrots and beets are beneficial.
Due to anemia, you need to eat foods rich in iron. It is advisable to limit:
- fatty fish;
- fatty dairy products (can lead to metabolic disorders);
- baked goods, sweets;
- fried and smoked.
Replace pork with turkey or chicken.
The danger of leukemia - life prognosis in children
The life prognosis for children with acute leukemia, for whom adequate treatment has not been selected, is unfavorable - death occurs in 100% of cases. With the use of modern chemotherapy, the course of the disease without relapse is observed in 50-60% of children. We can talk about recovery after 6-7 years of life without relapses.
The most dangerous complication of leukemia is infiltration of the brain, nerve trunks and meninges. Signs of neuroleukemia are: nausea, headaches, dizziness, stiff neck, diplopia. Infiltration of the spinal cord substance is manifested by sensory disturbances, paraparesis of the legs, and pelvic disorders.
Causes of chronic leukemia and the possibility of its prevention
Currently, some risk factors associated with the development of chronic leukemia are known. Thus, exposure to high doses of radiation from an atomic bomb explosion or a nuclear reactor accident increases the risk of chronic myeloid leukemia, but not chronic lymphocytic leukemia.
Prolonged exposure to herbicides or pesticides among rural residents may increase the risk of chronic lymphocytic leukemia.
High-voltage transmission lines may be a risk factor for the development of leukemia.
Most people with leukemia have no known risk factors, so there is no way to prevent the disease. The exception is smoking, which increases the risk of leukemia.
Prevention of leukemia
Primary prevention of leukemia in children (that is, carried out before the disease develops) includes:
- strengthening the immune system in order to reduce the risk of contracting infectious diseases (proper nutrition, hardening, etc.);
- avoiding contact with carcinogens, sources of ionizing radiation, and potentially hazardous chemicals.
After the onset of leukemia, secondary prevention is possible. It involves undergoing regular preventive examinations in order to timely detect relapses.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Why does this disease develop?
The exact causes of leukemia in children have not been established to date; only a number of dangerous factors that can lead to the disease have been identified.
First of all, it is called a genetic factor. The disease itself is not transmitted, we are talking about the tendency of cells to mutate. It has been noticed that those who have close relatives who suffered the same pathology get sick more often. It is also worth noting the connection with some congenital diseases (for example, with Down syndrome, the risk of developing a malignant process in the blood is 15 times higher than in healthy babies).
Radiation radiation, some chemical factors, as well as endogenous problems (immunodeficiency, hormonal imbalance) can cause the development and signs of leukemia in children.