Atherosclerosis, damage to large vessels and arteries, ischemia, heart attack, angina, stroke - this is only an incomplete list of the consequences that high cholesterol leads to, not to mention poor health. In addition to drug treatment and folk remedies, nutrition plays an important role in therapy for this pathology.
You need to know how to distribute essential nutrients (BJU) among different meals, how to create a menu, which foods to exclude from it, and which, on the contrary, to focus on. As practice shows, organizing a proper diet for hypercholesterolemia is the key to recovery and reducing the risk of developing the above complications.
There is a special diet for high cholesterol, which allows you to organize nutrition so that it becomes part of the treatment program.
The essence
Brief description of the diet. Type: therapeutic, hypolipidemic. Duration: until cholesterol levels normalize or for life if hypercholesterolemia is chronic or there is a predisposition to it. Results: keeping LDL concentration in the blood within normal limits, minimizing complications. Difficulty: medium.
For high cholesterol, a diet is prescribed, which is characterized by the following features:
- constant monitoring of daily caloric intake;
- compliance with the principles of proper nutrition;
- optimal balance of all nutrients necessary for the body (BJU);
- using the characteristics of a balanced diet: taking into account climate, concomitant diseases (hypertension, Gilbert's syndrome, obesity, diabetes), age, cholesterol level, gender differences, degree of complications.
The main feature of the diet is its therapeutic effect. It is intended primarily to normalize well-being and reduce the risk of complications. Therefore, first you need to consult with a specialist (therapist, cardiologist, phlebologist) to clarify the diagnosis, and then, with the test results and doctors’ conclusions, contact a nutritionist who will help you create the right menu. Subsequently, based on it, you can develop your own version of the diet.
Reviews and results
This nutritional therapy can be considered a transition to a healthy diet and lifestyle. The diet is effective not only in terms of weight loss, but also helps normalize cholesterol levels. Within a month you can lose 4 kg, but to normalize lipid metabolism you need to follow it for at least six months.
Since this diet is balanced, you can stick to it constantly. Some discomfort is caused by a decrease in the amount of salt, simple carbohydrates and the absence of smoked and meat products. Nevertheless, these restrictions are justified and have a positive effect on health.
- “... My result is that cholesterol has normalized, although not with the help of diet alone. It was prescribed in addition to the pills. I excluded fatty and fried foods, sausages, pates, sweets and sweet pastries, I very limited sugar and jam. This diet helped me lose weight and I began to feel much better. The doctor advised me to eat like this all the time, but it’s difficult for me and sometimes I break it - I really want sausage, ham or other meat products. Occasionally I allow myself this, but I choose low-fat varieties. I think that nothing bad will happen in one or three times. The main thing is that the basic nutrition is correct. In 6 months I lost 5 kg, and it wasn’t difficult”;
- “... My weight exceeds the norm by 10 kg. It became difficult to move, and the examination revealed high cholesterol. The doctor assured that the diet was simply necessary and advised me to limit myself to it for three months. I started with losing weight and ended with an anti-cholesterol diet. Almost one replaces the other and acts in the same direction. I strictly limit myself - only boiled lean meat, fish, vegetables, berries, bran, kefir, in the morning - oatmeal with flax oil (though it is very bitter). In three months I ate as many vegetables and fruits as before in six months. The indicators are closer to normal, but we need to constantly monitor our weight and tests.”
Peculiarities
The diet takes into account the gender and age characteristics of the patient.
Gender
High cholesterol in women is associated primarily with their cravings for sweets, constant weight fluctuations (either dieting or overeating) and hormonal changes. Therefore, a lipid-lowering diet for them is based on limiting complex carbohydrates and prohibiting any fasting. In addition, it is compiled taking into account pregnancy, the postpartum period and the onset of menopause after 45-50 years. The most difficult thing is to give up cakes, ice cream, sweets, pastries, and fast food.
The advantage of this therapeutic nutrition system for women is the availability of an option for overweight. It allows you to reduce your daily caloric intake to the permitted level and keep your body weight under control without strict restrictions.
High cholesterol in men is usually diagnosed due to abdominal obesity, physical inactivity, and abuse of fatty and salty foods. Therefore, a lipid-lowering diet categorically prohibits them from drinking alcoholic drinks with high-calorie snacks, and also recommends that they simultaneously exercise, but in moderation, according to a separate program.
Age
If high cholesterol is diagnosed in a child, a lipid-lowering diet is prescribed to him with great caution and only with strict adherence to all the specialist’s recommendations. Despite the fact that for adults it involves a significant restriction of fats, in childhood this is unacceptable, as it will negatively affect the development of the nervous system. Therefore, the same dairy products should remain in the diet completely. But fast food and sweets should be limited (you shouldn’t ban them at all), finding healthy alternatives for them.
The same applies to those who were diagnosed with high cholesterol after 50 years of age. Restrictions should be approached with extreme caution, otherwise you can harm your health. The risk of diabetes also increases at this age. Therefore, you need to constantly monitor your blood glucose levels and take into account the glycemic index of foods when choosing a menu.
General principles of dietary nutrition
Each person can create an approximate menu for himself from products allowed for consumption (this is described below). But an important point of the diet is the daily consumption of complex carbohydrates (their volume should be 50–60% of the total food eaten per day).
Complex carbohydrates that take a long time to digest and provide a feeling of fullness include pasta, cereals, whole grain bread, as well as fruits and vegetables. Fruit salads and vegetable dishes cleanse blood vessels of cholesterol deposits, give them tone, and make capillaries elastic and less brittle. A third of all vegetables eaten per day should be consumed raw.
Proteins are fish, lean meats and cottage cheese. Preference is given to poultry meat with the skin removed, and it is better to stew or boil it rather than fry it. For a side dish, it is better to choose stewed vegetables or complement the meat dish with fresh vegetable salad. This way the meat is digested more efficiently.
Egg whites are cholesterol-free, so you can eat them without restricting yourself. But the yolk contains substances that help increase the levels of the substance in the blood, which is why you are allowed to eat no more than three yolks per week. Dairy products should be chosen low-fat.
Small meals are another important point in the fight against bad cholesterol. It is better to eat food more often (up to 5–6 times a day), but in small portions, than to eat 1–2 times, but in large quantities. This facilitates the work of the gastrointestinal tract, creating a feeling of constant satiety. If you feel like you have an “empty stomach,” you can drink a glass of natural yogurt or low-fat kefir.
No ads 2
Reminders
For those who are prescribed a diet against high cholesterol, the attending physician usually issues accompanying instructions. They reflect the basic principles of nutrition for this pathology. They must be followed strictly if there is a desire to recover.
Important note. The numbers in the instructions may vary, as the doctor and nutritionist adjust them depending on the individual course of the disease.
Product reminder:
- Fruits are eaten fresh every day, preferably seasonal ones. Make homemade juices from them.
- Vegetables - fresh, as well as stewed, baked, steamed and boiled. According to the season. Make homemade juices from them (without adding spices and salt).
- Legumes - 2 times a week.
- Meat - not fatty (beef, veal, turkey, chicken, rabbit) and not fried.
- Dairy products - low-fat or low-fat.
- Vegetable oil is for dressing salads; you cannot fry with it. Cold pressed. The daily norm is 2 tbsp. l.
- Salt - 5 g per day.
- Sugar - 50 g.
Nutrient Reminder:
- Complex carbohydrates - 400 g per day. Limit simple ones to a minimum. The basis is cereals.
- Proteins - 70 g. Animal to vegetable ratio: 50/50.
- Fats - 70 g. Animal to vegetable ratio: 35/65.
Nutrition reminder:
- The size of one serving is determined based on the presence/absence of excess weight and daily calorie content.
- Fractional 6 meals a day.
- Approximate diet: breakfast (7:00), lunch (10:30), lunch (14:00), afternoon snack (16:30), dinner (18:30), before bed (22:00).
- Dishes must be fresh and prepared daily.
- The daily water requirement is 1.5 liters.
First, you will have to spend some time looking at the lists of allowed and prohibited foods, the standard menu, weighing everything (kitchen scales are necessary), calculating the optimal daily caloric intake for your height and body weight, and dealing with many other issues reflected in these instructions. However, soon you will develop the necessary skills (learn to determine the serving size “by eye”, create your own version of the diet with alternative dishes, etc.) and the body will get used to such a healthy diet.
Fully or partially limited products
- High cholesterol products, sausages, canned food and all kinds of smoked meats, fatty pork, duck and goose meat, refractory animal fats, canned fish, smoked fish and caviar are completely excluded.
- Meat and fish broths.
- Products made from puff pastry or butter dough, products with cream. For obesity - sugar, sweets, jam, confiture, chocolate, ice cream.
- Fatty dairy products (cheese, cream, cottage cheese, sour cream).
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Fruits | ||||
| bananas | 1,5 | 0,2 | 21,8 | 95 |
Nuts and dried fruits | ||||
| raisin | 2,9 | 0,6 | 66,0 | 264 |
Cereals and porridges | ||||
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
Bakery products | ||||
| bagels | 16,0 | 1,0 | 70,0 | 336 |
| bagels | 16,0 | 1,0 | 70,0 | 336 |
| crackers | 11,2 | 1,4 | 72,2 | 331 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jam | 0,3 | 0,1 | 56,0 | 238 |
| candies | 4,3 | 19,8 | 67,5 | 453 |
| pastry cream | 0,2 | 26,0 | 16,5 | 300 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Cakes | ||||
| cake | 4,4 | 23,4 | 45,2 | 407 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
Dairy | ||||
| cream | 2,8 | 20,0 | 3,7 | 205 |
| sour cream 30% | 2,4 | 30,0 | 3,1 | 294 |
| sour cream 40% (fat) | 2,4 | 40,0 | 2,6 | 381 |
Cheeses and cottage cheese | ||||
| cheese | 24,1 | 29,5 | 0,3 | 363 |
| cottage cheese 18% (fat) | 14,0 | 18,0 | 2,8 | 232 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
| pork liver | 18,8 | 3,6 | 0,0 | 108 |
| pork kidneys | 13,0 | 3,1 | 0,0 | 80 |
| pork fat | 1,4 | 92,8 | 0,0 | 841 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
| beef liver | 17,4 | 3,1 | 0,0 | 98 |
| beef kidneys | 12,5 | 1,8 | 0,0 | 66 |
| beef brains | 9,5 | 9,5 | 0,0 | 124 |
| mutton | 15,6 | 16,3 | 0,0 | 209 |
Sausages | ||||
| smoked sausage | 16,2 | 44,6 | 0,0 | 466 |
| smoked sausage | 9,9 | 63,2 | 0,3 | 608 |
| sausages | 10,1 | 31,6 | 1,9 | 332 |
| sausages | 12,3 | 25,3 | 0,0 | 277 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| salted fish | 19,2 | 2,0 | 0,0 | 190 |
| Red caviar | 32,0 | 15,0 | 0,0 | 263 |
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| squid | 21,2 | 2,8 | 2,0 | 122 |
| shrimps | 22,0 | 1,0 | 0,0 | 97 |
| salmon | 19,8 | 6,3 | 0,0 | 142 |
| sturgeon | 16,4 | 10,9 | 0,0 | 163 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
| semi-finished fish products | 12,5 | 6,7 | 14,7 | 209 |
| sardine | 20,6 | 9,6 | — | 169 |
| mackerel | 18,0 | 13,2 | 0,0 | 191 |
| cod (liver in oil) | 4,2 | 65,7 | 1,2 | 613 |
| boiled oysters | 14,0 | 3,0 | — | 95 |
| fresh oysters | 14,0 | 6,0 | 0,3 | 95 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
| creamy margarine | 0,5 | 82,0 | 0,0 | 745 |
| coconut oil | 0,0 | 99,9 | 0,0 | 899 |
| palm oil | 0,0 | 99,9 | 0,0 | 899 |
| rendered beef fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
| rendered pork fat | 0,0 | 99,6 | 0,0 | 896 |
Non-alcoholic drinks | ||||
| cola | 0,0 | 0,0 | 10,4 | 42 |
| lemonade | 0,0 | 0,0 | 6,4 | 26 |
| Pepsi | 0,0 | 0,0 | 8,7 | 38 |
| sprite | 0,1 | 0,0 | 7,0 | 29 |
| * data is per 100 g of product | ||||
Product table
One of the most important points in the diet for people with high cholesterol is to strictly adhere to two lists. These are permitted and prohibited products. The first group includes those that are not just good for health and promote weight loss, but primarily have hypolipidemic properties, that is, they reduce the level of bad LDL in the blood. The second includes those that, on the contrary, increase their concentration, and also mostly refer to unhealthy foods that provoke the appearance of excess weight.
For convenience, the lists are presented in the form of a table; the products are divided into food categories, so they will be easy to find.
Recommended and prohibited products
When selecting recipes, you need to take into account their composition. Some foods are strictly prohibited for people with high cholesterol. These include spicy, salty, fried foods, and smoked foods. List of permitted and prohibited products:
| Can | It is forbidden | |
| Meat | lean poultry meat (chicken, quail); veal, beef, rabbit, horse meat. | fatty poultry meat: duck, goose, turkey; pork, lamb, lard. |
| Animal by-products | Liver, kidneys, tongue (beef) | Heart, brains, smoked meats from any offal |
| Poultry by-products | Heart, liver, stomach | Salted and smoked products |
| Sausages | Low-fat sausages, chicken ham | Pate, fatty sausages, salami, sausages |
| Fish | Trout, pike, tuna, cod | Carp, herring, salmon |
When preparing meals, only recommended products should be used. Otherwise, the amount of cholesterol may increase, continuing to clog blood vessels.
Diet options
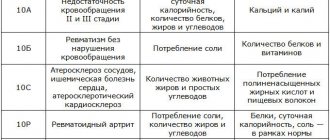
For cardiovascular diseases, a standard diet is prescribed - treatment table number 10 according to Pevzner. It is also recommended for high bad cholesterol, which is the main provocateur of the development of CVD. However, you need to keep in mind that within it there is a separate classification for more refined diagnoses. Therefore, if hypocholesterolemia is accompanied by a number of other pathologies, you need to look at this gradation.
All diet options No. 10 are similar to each other and differ only in the following points:
- 10A - low fat;
- 10B - protein-carbohydrate;
- 10C - maximum balanced;
- 10P - low carbohydrate diet;
- 10G - salt-free;
- 10I - drinking.
A more detailed description of the options for diet No. 10 is shown in the table below.
Most often, for high cholesterol, treatment table No. 10C is prescribed, which has a hypolipidemic effect. It, in turn, is divided into two more options - with obesity and without it.
Advantages and disadvantages
| pros | Minuses |
|
|
Sample menus
To lower high cholesterol, you need to focus on the sample menu for the above options for treatment table No. 10. It will help you understand the principle of preparing a diet, and in the future you can do it yourself, selecting alternatives to some dishes in accordance with your taste preferences.
Table No. 10
Prescribed for various cardiovascular diseases, which are characterized by circulatory failure. This condition is often caused by high cholesterol. Since this table is the main one, you need to know how to eat properly on it.
A sample menu for the week will help you navigate the choice of dishes and products. In some versions of diet No. 10, soups are prohibited. So, if you are not accustomed to them, they can be replaced without any damage to health with side dishes made from durum wheat cereals or pasta.
Table No. 10C
Prescribed for high cholesterol and already diagnosed atherosclerosis. Diet No. 10C reduces the level of low-density lipoproteins in the blood, cleanses blood vessels and destroys atherosclerotic plaques.
A sample menu for 3 days will allow you to correctly create your own diet. It is designed for a daily calorie content of 2000-2200 kcal, that is, with high cholesterol against the background of overweight and obesity. If there is no such problem, you should raise the bar to 2500-2700 kcal by adding permitted sweets (dried fruits, sweet fruits and berries, honey, homemade desserts) and increasing potatoes in the diet.
Table No. 10G
This diet is prescribed for hypertension, which, in turn, is a frequent accompaniment of high cholesterol. Designed to simultaneously reduce both. When compiling a diet, you can focus on an approximate menu for 3 days.
Hypocholesterol diet menu for a week (Diet)
Taking into account the permitted foods and dietary habits, it is not difficult to create a menu for the week. It is important to increase the amount of vegetables, fruits and polyunsaturated fatty acids in the diet. It is advisable to consume up to 500 g of fruits and vegetables daily.
A large amount of dietary fiber is found in oatmeal (whole), prunes, gooseberries, cranberries, figs, raspberries, dates, raisins, bran and dried apricots. You will forever have to give up sausages, liver pates, ham, fatty cheeses, sugar, sweets, cakes and cream pies, jams, preserves and sweet pastries. You can maintain HDL levels by eating flax seeds, walnuts, soy products and occasionally fatty fish.
An approximate menu for a standard hypocholesterolemic diet might look like this:
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Recipes
For breakfast. Barley porridge
If you have high cholesterol, you should eat only well-steamed cereals. Therefore, it is recommended to soak them in warm water in the evening so that they are properly boiled in the morning. Rinse 300 g of pearl barley several times, pour warm water so that it completely covers the barley. Leave overnight.
In the morning, drain the water and rinse again. Pour water into the barley in a ratio of 2 to 3. After boiling, reduce the heat to low, do not open the lid and cook the porridge for 40 minutes. Then, without opening the lid, turn off the stove and leave it to steep for 20 minutes.
At this time, boil 100 ml of 1.5% milk, chop some apples and oranges, chop 10 g of walnuts. Place the required portion of barley on a plate, pour hot milk, sprinkle with fruits and nuts. Instead of butter, it is better to use any vegetable oil, replace sugar with honey.
On the first. Buckwheat soup
Sort, rinse and fry 100 g of buckwheat in a dry frying pan. Boil by adding 1 tbsp to water. l. any cold pressed vegetable oil. In 20 minutes. Place 200 g of diced potatoes, 50 g of grated carrots, chopped onion and a little parsley root (20 g) into water. Cook for another 15 minutes. Before serving, top the soup with chopped garden herbs.
On to the second. Steamed vegetable cutlets
Grind 2 oven-baked and cooled potatoes onto a coarse grater, 3 carrots and 2 beets (medium sized) into a fine grater. Squeeze the juice from the resulting carrot and beet puree and remove it. Grind 1 onion and 4 pcs. prunes Mix all ingredients. Add 30 g of semolina flour to bind the mass. Knead thoroughly. Do not add salt. Form small cutlets. Roll them in sesame seeds. Place in a steamer. Time - 30 min.
Salad. Fish under a fur coat
Boil 150 g of potatoes, carrots and beets, 3 eggs, 200 g of any sea fish fillet (whichever you like best). Peel 2 onions, chop them and sauté for 7 minutes. over low heat. Grind the vegetables on a coarse grater, and the egg white on a fine grater. Cut the fish into small pieces.
For dressing, instead of mayonnaise, prepare a separate sauce: mix 100 g of 10% sour cream and 50 g of lemon juice. Place the ingredients on a flat and wide dish in layers: potatoes - fish - onions - coat with dressing - beets - carrots - coat with dressing - repeat all layers again. Sprinkle egg white on top and garnish with parsley leaves.
Dessert. Fruit salad
Peel, core and pit 1 red apple, 2 apricots, 100 g pineapple, 50 g orange. Prepare 50 g of pomegranate seeds and 30 g of chopped walnuts. Cut the fruits into small cubes and mix them. Place in portioned salad bowls, pour over lemon juice, sprinkle with pomegranate seeds and walnuts on top.
Bakery. Curd cookies
Store-bought baked goods are prohibited if you have high cholesterol, but homemade baked goods can be included in your diet once a week. It should be remembered that margarine and butter are strictly prohibited.
Mix 100 g of low-fat cottage cheese, 200 g of oatmeal (you can prepare it yourself by chopping regular flakes). After thoroughly kneading, add 2 tbsp. l. warm water and the same amount of vegetable oil. For a sweet taste, you can add 1 tsp. honey or 2 tbsp. l. orange zest. Form cookies, place on a baking sheet, previously greased with a small amount of vegetable oil. Bake in the oven at 180°C. Time - 10 min.
Beverages. Hot toddy
Brew large-leaf natural black tea in a ceramic teapot. In 10 minutes. pour it into a cup (200 ml). It is important that it is hot and strong. Add 50 ml of freshly squeezed lemon juice, 50 ml of vanilla syrup, a circle of lemon, a pinch of cloves and cinnamon. Mix. To cover with a lid. Drink after 5 minutes.
Cholesterol content in specific foods
To reduce cholesterol, you need to eat healthy foods, which will help reduce levels of harmful substances. But how can we determine which products contain the least amount of this compound? The table below will help with this.
| Product type (in grams) | Cholesterol content |
| By-products: | |
| Brain | 2000 milligrams |
| Kidneys | 1100–1200 milligrams |
| Liver | 400-500 milligrams |
| Meat and poultry: | |
| Pork | 110 milligrams |
| Mutton | 90–100 milligrams |
| Rabbit | 90 milligrams |
| Beef | 80–90 milligrams |
| Goose | 90 milligrams |
| Duck | 90 milligrams |
| Chicken | 70–90 milligrams |
| Turkey | 60–70 milligrams |
| Eggs: | |
| Chicken yolk, 100 grams | 1234 milligrams |
| Chicken egg, 1 pc. | 210–280 milligrams |
| Quail egg, 1 pc. | 80–90 milligrams |
| Fish and other seafood: | |
| Fish fat | 485 milligrams |
| Chum salmon | 214 milligrams |
| Carp | 90–170 milligrams |
| Shrimps | 152 milligrams |
| Red salmon | 141 milligrams |
| Squid | 85–95 milligrams |
| Coho salmon | 60 milligrams |
| Cod | 30–50 milligrams |
| Horse mackerel | 40 milligrams |
| Dairy products: | |
| Butter | 180 milligrams |
| Hard cheese | 80–120 milligrams |
| Sour cream, 30% fat | 100 milligrams |
| Adyghe cheese | 70 milligrams |
| Cream, 20% fat | 60–70 milligrams |
| Cottage cheese, 18% fat | 60 milligrams |
| Milk, 3% fat | 14.4 milligrams |
| Milk, 2% fat | 10 milligrams |
| Kefir, 1% fat | 3.2 milligrams |
You don’t need to have the knowledge of a doctor to understand which foods should be avoided according to the table, and which should be given preference. Next, we will talk about the list of prohibited foods and why it is not recommended to eat them if your blood cholesterol levels are elevated.
Individual cases
High cholesterol is considered the main cause of various cardiovascular diseases. Therefore, it is often accompanied by various health problems. In this case, you need to keep in mind what food restrictions and diets there are for diagnosed pathologies in order to be able to combine them with each other. This is quite difficult, so at first you cannot do without consulting doctors and nutritionists.
For thick blood and high cholesterol
Diagnosis: hyperviscose syndrome.
The basic rule of the diet: increase water consumption to 2 liters per day.
The basis of the diet are foods that thin the blood and at the same time reduce high cholesterol:
- tomatoes;
- fatty sea fish, kelp, fish oil;
- oils: sunflower, pumpkin, olive, nut;
- sour berries: gooseberries, currants, cranberries, viburnum, lingonberries, blueberries;
- sour fruits: all citrus fruits, kiwi;
- ginger;
- peanuts, hazelnuts;
- low-fat kefir, yogurt, ayran;
- honey;
- flax-seed.
Some foods that thicken the blood cannot be completely excluded from the diet, since many of them are beneficial for the body, but in case of such pathology it is worth limiting them (up to 1-2 times a week in small quantities):
- buckwheat;
- bananas;
- chokeberry.
But most products that thicken the blood are harmful to the body and increase bad cholesterol, so you should forget about them in case of such a disease:
- fatty meat (lamb, pork, goose, duck), lard, sausages;
- fried foods, smoked meats;
- margarine;
- whole village milk, butter, cream, sour cream;
- fast food;
- refined sugar;
- white bread, pastries, muffins;
- lemonade.
For high sugar and cholesterol
Diagnosis: diabetes mellitus.
Therapeutic diet: table No. 9.
The basic rule of the diet: for type I diabetes mellitus, create a menu based on the table of bread units; for type II diabetes mellitus - guided by the glycemic index table.
Sugar-lowering foods that you need to focus on in this diet:
- cabbage and grapefruit juices;
- the grapefruit itself;
- chicory drink;
- Jerusalem artichoke;
- herbal teas with the addition of ginseng and eleutherococcus (possibly with pharmaceutical tinctures), rose hips, St. John's wort flowers, dandelion roots, nettle leaves;
- flaxseeds (can be ground and added to porridges and cocktails);
- celery greens, asparagus, parsley;
- horseradish (not in the form of a spice, but the root, grated at home), onions (for high cholesterol, only boiled), garlic.
First of all, everything sweet is prohibited. You will have to exclude from the diet even those sweets that are allowed on the menu of treatment table No. 10.
With increased bilirubin and cholesterol
Diagnosis: Gilbert's syndrome.
Therapeutic diet: table No. 5.
The basic rule of the diet: increase water consumption to 2.5 liters per day, eliminate salt and alcohol from the diet.
The menu should focus on products that reduce elevated levels of bile pigment (bilirubin) and at the same time are useful for hypercholesterolemia. These include:
- sweet fruits: persimmons, grapes, bananas, figs, lychees, pomegranate, mango, red apples;
- low-fat dairy products;
- chicken, turkey;
- vegetable soups;
- cereal porridge;
- egg white;
- herbal teas (birch, St. John's wort, chamomile).
You need to avoid foods that increase stomach acidity:
- radishes, onions, mushrooms, sorrel;
- citrus;
- confectionery products with soda and baking powder;
- seafood;
- sweets;
- red meat;
- canned food;
- vinegar, store-bought sauces;
- coffee, alcohol.
Dietary correction of hypercholesterolemia
Among the causes of disability and mortality in the population (for men over 45 years of age and women over 65 years of age) in economically developed countries, cardiovascular diseases (CVD) continue to occupy the leading place. The development and progression of this pathology is due to the severity of atherosclerotic vascular damage, the correction of which should be the main preventive measures.
To date, more than 250 risk factors for the development of CVD have been identified, which are divided into: non-modifiable - gender, age, genetic and ethnic factors and modifiable - hyperlipidemia (HLP) (increased levels of cholesterol (HC) and low-density lipoprotein cholesterol (LDL-C), low high-density lipoprotein cholesterol (HDL-C) level), obesity, arterial hypertension (AH), nutritional disorders, smoking, low physical activity, alcohol, diabetes mellitus, impaired endothelial function, hyperhomocysteinemia, hypercoagulation, oxidative stress, inflammation, etc.
Hypercholesterolemia (HCH), together with arterial hypertension and smoking, is among the top three most powerful risk factors for CVD. A progressive and continuous relationship between mortality from coronary heart disease (CHD) and serum cholesterol concentrations is considered to be proven. According to WHO, an elevated level (more than 5.0 mmol/l) of cholesterol in the blood serum is a risk factor for premature mortality in 23% of cases and causes 12.4% of lost years of healthy life in Russian residents.
Data from epidemiological cooperative studies conducted in Moscow and St. Petersburg showed that over the age of 30 years, 55% of men and 56.9% of women have elevated levels of cholesterol. The development and progression of CVD is determined by the severity of atherosclerotic vascular damage, and the main efforts to prevent these diseases should be aimed at its correction.
The most important condition in the correction of all links in the pathogenesis of CVD, and especially lipid metabolism disorders, using diet therapy is the qualitative and quantitative correction of the fat component of the diet.
A positive correlation has been established between the level of cholesterol in the blood serum and mortality from CVD, on the one hand, and excess (more than 40% of total calories) consumption of animal fat containing saturated and trans isomers of fatty acids and cholesterol, on the other hand.
It is believed that an increase in the consumption of cholesterol in the amount of 100 mg per 1000 kcal/day helps to increase blood cholesterol by 12%. At the same time, a 1% decrease in total cholesterol in the blood serum is associated with a 2% decrease in the risk of coronary artery disease. The degree of restriction of exogenous cholesterol intake from food should be from 250 to 500 mg/day, depending on the presence and type of HLP. According to the recommendations of the National Cholesterol Education Program (NCEP), for moderate hypercholesterolemia, its amount in the diet should not exceed 300 mg/day, and for severe hypercholesterolemia, 200 mg/day. To do this, exclude foods rich in cholesterol from the diet (brains, internal organs of animals, fish caviar, butter, fatty cheeses, egg yolk, etc.).
The total fat content should be up to 30% of the calorie intake (70–80 g/day); of this amount, 8–10% should be saturated fatty acids (SFA), 10–15% — monounsaturated fatty acids (MUFA), 7–9% — polyunsaturated fatty acids (PUFAs). Sources of EFAs are fats of animal origin - fatty meat, fish, sausages, dairy products, etc.
In addition to SFAs, an increased risk of these diseases is associated with the consumption of trans isomers of fatty acids, which are formed during the hydrogenation of PUFAs during the production of margarines. Natural butter of different brands contains from 0.6 to 4.2% trans isomers of fatty acids, and margarines contain over 10%.
The main representative of MUFA is oleic acid, found in large quantities in olive oil. Olive oil forms the basis of the so-called “Mediterranean diet,” that is, the type of diet that has developed among residents of countries located on the Mediterranean coast. According to an epidemiological survey, the population of these countries has an extremely low mortality rate from cardiovascular diseases.
PUFAs, as well as MUFAs, help reduce hypercholesterolemia and the risk of thrombosis. Sources of omega-6 PUFAs (linoleic acid) are vegetable oils (sunflower, corn, cottonseed, etc.). The optimal consumption of these acids is 6–8% of the total calorie intake.
It is very important for patients with CVD to use in their diet sources of PUFAs of the omega-3 family - fatty sea fish (mackerel, sardine, herring, halibut, etc.), containing long-chain fatty acids (eicosapentaenoic and docosahexaenoic), from which prostaglandins, thromboxanes, and leukotrienes are formed , which have antiplatelet, hypotensive, anti-inflammatory, and immunocorrective effects. Based on the results of population studies, a clear inverse relationship has been established between the prevalence of cardiovascular diseases, the mortality of patients from this pathology, and the content of omega-3 PUFAs in their diet. Thus, the extremely low incidence rate among the Eskimos of Greenland, Chukotka and Japanese fishermen is associated with their consumption of large amounts of marine fish from the northern seas, which provides up to 10 g per day of omega-3 PUFAs.
A daily intake of 0.5–1.0 g of omega-3 PUFAs from fatty marine fish or purified fish oil is known to reduce the risk of CVD mortality in middle-aged people by 30–40%.
Omega-3 PUFAs (alpha-linolenic acid, from which eicosapentaenoic and docosahexaenoic acids are formed in the body) also contain vegetable oils, such as flaxseed, soybean, rapeseed, mustard, sesame, walnut, etc. The consumption of omega PUFAs is considered optimal for patients with CVD -3 in the amount of 1–2% of the total calorie intake. It is desirable that vegetable oils make up half of the fat component of the diet, since in addition to MUFAs and PUFAs, they also contain biologically active anti-atherogenic components such as phospholipids, squalene, phytosterols and phytostanols.
Phospholipids have an antioxidant, hypolipidemic effect, stabilize the solution of cholesterol in bile and reduce the absorption of cholesterol in the intestine. The optimal level of phospholipid intake (the main source of which in the diet is vegetable oils) is considered to be 5 g/day. During the refining of vegetable oils, most of the phospholipids are lost, so they can be introduced into the diet in the form of dietary supplements (BAA) to food (for example, such as Vitol).
In addition to the fatty component of the diet, protein and soy isoflavones and dietary fiber (DF) affect lipid metabolism.
Sources of vegetable protein in the diet of patients with CVD are cereals, baked goods, and legumes (especially soy protein products). The biological value of soy protein is 2 times higher than that of other plant proteins, and is close to that of animal proteins (meat and milk). Soy contains a wide range of vitamins and minerals, the presence of minor biologically active components, such as isoflavones, which determine the hypolipidemic, antioxidant, hypohomocysteinemic, hypotensive and thrombolytic effects of its processed products. According to WHO experts, daily consumption of 25 g of soy protein containing 3.4 mg of isoflavones reduces blood cholesterol levels and the risk of developing cardiovascular diseases. It is preferable to use soybean processing products with a high content of isoflavones (soy protein texture) or add isoflavones to an antiatherogenic diet as part of a dietary supplement (100–200 mg per day for 1 month).
Plant foods are also an important source of carbohydrates. Moreover, if refined carbohydrates (sugar and confectionery products containing it) cause an increase in the levels of very low density lipoproteins (VLDL) and triglycerides (TG) in the blood, then complex carbohydrates (polysaccharides), which include dietary fiber (DF), contribute to a decrease levels of TG and cholesterol of atherogenic fractions of lipoproteins in the blood serum, a decrease in blood pressure and excess body weight.
PV is a heterogeneous group of substances that for the most part are not digested or absorbed in the human gastrointestinal tract. All products of plant origin are considered sources of PV. The main representatives of PP are cellulose, hemicellulose and pectin. Adding 15 g of soluble polyphosphates (pectin, guar gum) to the daily diet reduces blood cholesterol levels by 15–21%. Wide inclusion of vegetables, fruits, and grains in the diet allows you to fully meet the body's need for dietary supplements, which is 30–50 g/day. If indicated, you can increase the consumption of PF due to their additional sources - wheat bran, chemically pure pectin, methylcellulose, etc. However, long-term consumption of PF more than 60 g per day can lead to impaired absorption of vitamins and microelements.
The issue of the effect of alcohol on the lipid profile and the possibility of its administration for the purpose of correcting lipid metabolism disorders is often discussed. If the doctor is confident that the patient will strictly follow his prescriptions in terms of drug and non-drug treatment, then he can allow the patient to take alcohol in the following doses: vodka, or cognac, or whiskey - 45–50 ml per day, red table wine or white - 150 ml per day. Of these drinks, wine is preferable because studies have shown that in countries where the population consumes mainly red wine, which contains antioxidants, mortality from CVD is lower than in countries where preference is given to spirits or beer.
It is known that excess consumption of refined carbohydrates, alcohol and animal fats increases the energy value of the diet. The calorie content of the diet and the imbalance of the body’s energy balance have a pronounced effect on the state of lipid metabolism. An increase in caloric intake is accompanied by an increase in endogenous cholesterol synthesis, an increase in the level of cholesterol, LDL cholesterol and VLDL cholesterol in the blood plasma. The amount of endogenously synthesized cholesterol increases by 20 mg for every kilogram of excess body weight (BMI). Against the background of excess caloric nutrition, the atherogenicity of animal fats and refined carbohydrates increases.
Analysis of the interdependence of various risk factors showed that HLP largely depends on the degree of BMI and reducing body weight is the primary task to reduce the content of cholesterol and TG in the blood serum, both for the purpose of prevention and treatment of IHD. The most common approach to weight loss is to prescribe a low-calorie, nutritionally balanced diet.
To reduce the caloric content of the diet and its fat content, it is very important to use the correct cooking technology. Removing fat and extractive substances from meat and fish products is achieved by preliminary boiling them, then baking or stewing. When boiling meat, poultry and fish, the fat they contain goes into the broth, while the meat loses 40%, and fish 50% of fat. For the same purposes, it is useful to use a microwave oven, grill, or Teflon-coated dishes.
The important role of some micronutrients in the regulation of lipid metabolism is also known. Iodine affects the function of the thyroid gland, has a hypocholesterolemic effect, and the ability to prevent the deposition of lipids in the vascular wall and the formation of atherosclerotic plaque. Its significant source is seafood: sea fish, shrimp, sea cucumbers, mussels, seaweed. The optimal iodine content in the diet is up to 0.5 mg per day. Consumption of seafood allows you to fully meet the increased need for iodine in patients with atherosclerosis (sea fish, shrimp, sea cucumbers, mussels, sea kale).
The importance of optimal chromium content in the diet is associated with its participation in carbohydrate and lipid metabolism. The protective role of chromium is explained by its hypoglycemic, hypocholesterolemic effect, as well as its ability to prevent the deposition of lipids in the vascular wall and the formation of atherosclerotic plaque. The main sources of chromium are baker's yeast, wholemeal rye and wheat flour, meat, legumes, pearl barley and corn grits.
Along with this, for the correction of hypercholesterolemia, it is very important to consume foods containing micronutrients that suppress oxidative stress.
Some vitamins, minerals and minor food components found in plant foods have an antioxidant effect. Sources of antioxidant vitamins include vegetable oils, nuts, seeds, legumes (vitamin E), and a variety of vegetables and fruits (vitamin C). B vitamins, along with animal products (meat, fish, liver, milk, seafood), contain legumes (soybeans, beans), wholemeal flour, buckwheat and oatmeal, millet, yeast, cauliflower, green onions, etc.
Fat-soluble vitamin A, which has an antioxidant effect, is found in products of animal origin, such as liver, butter, eggs, and chum salmon caviar; and beta-carotene (from which vitamin A is synthesized in the body) is mainly found in plant foods (red carrots, red peppers, spinach, green onions, sorrel, sea buckthorn, tomatoes, rowan).
Selenium is also a trace element with antioxidant properties. Epidemiological studies have noted an inverse correlation between the level of selenium in the blood plasma, on the one hand, and the risk of developing atherosclerosis and increased activity of lipid peroxidation (LPO), on the other hand. A decrease in selenium levels correlates with an increase in blood clotting and an increase in the synthesis of thromboxane A2 and leukotrienes. Along with this, its deficiency is accompanied by a decrease in the activity of glutathione peroxidase in platelets, erythrocytes, and arterial walls.
Of the minor food components, flavonoids, which are found in plants belonging to the families Rosaceae, legumes, buckwheat, Asteraceae, and in vegetables and fruits, have high biological activity. The antioxidant effect of flavonoid compounds is associated with their ability to scavenge free radicals and/or chelate metal ions that catalyze oxidation processes. In addition to antioxidant properties, they have capillary-strengthening, cardioprotective, antispasmodic and diuretic effects.
The hypolipidemic and antioxidant effects of squalene, contained in shark liver oil and oil obtained from amaranth seeds (Amarantus L), are also known. The nature of the biological action of squalene was studied in experiments on rats. It has been shown to have a hypocholesterolemic, immunostimulating effect, with no negative effect on biochemical parameters and the structure of internal organs.
In addition to squalene, the oil obtained from amaranth seeds also contains significant quantities of PUFAs, tocopherols, phospholipids and phytosterols. Phytosterols and phytostanols are found in soybean, coconut, rapeseed oil, coniferous seed oil, seeds, nuts, fruits, vegetables, etc. Interest in products containing plant sterols increased in the 90s of the last century. They are practically not absorbed in the gastrointestinal tract, i.e. they have only a local effect, and therefore are safer means. More than 40 varieties of plant sterols have been identified. Stanols are saturated derivatives of sterols.
In populations with a typical Western diet, the average level of plant sterols is 150–350 mg/day, and stanols are 50 mg/day. Studies conducted in recent years have found that foods with phytosterols at a dose of 2–3 g/day reduce cholesterol levels by 10%, LDL cholesterol by 14%, and in combination with a low-fat and low-cholesterol diet by 24%.
The American National Education Program provides evidence that improving an individual's diet is associated with a reduction in their risk of CVD. In the latest version of the diet to reduce the level of cholesterol in the blood plasma, recommended by the American National Education Program, there is a recommendation to introduce into daily consumption foods enriched with plant sterols and stanols (at the rate of 2 g/day).
In recent years, more than 40 clinical studies have been conducted worldwide to evaluate the effectiveness of various types of foods fortified with plant sterols and stanols. It was found that foods enriched with phytosterols at a dose of 2-3 g/day reduce cholesterol levels by 10-12%, LDL cholesterol by 14-16%, and in combination with a low-fat and low-cholesterol diet - by 24%.
A similar study found a decrease in LDL cholesterol levels by almost 16% after consuming sitostanol esters at a dose of 2 g/day in the form of mayonnaise, while no significant effect was obtained when using sitostanol at a dose of 800 mg/day. A decrease in the levels of total cholesterol and LDL cholesterol under the influence of sitostanol esters at a dose of 3 g/day was demonstrated in patients with type 2 diabetes mellitus and in children with familial hypercholesterolemia (reduction in LDL cholesterol by 15%).
In 1995, the results of a study were published within the framework of the North Karelian project, which studied the effect on the level of LDL cholesterol of short-term and long-term (1 year) introduction into the diet of patients with moderate hypercholesterolemia of a spread made on the basis of rapeseed oil containing various doses of sitostanol esters , which led to a sustained reduction in LDL cholesterol by 15%. This project demonstrated that consumption of phytostanol esters at doses ≥ 1.8 g/day is an effective, long-acting agent for reducing plasma total cholesterol and LDL cholesterol.
Reliable evidence of the effectiveness of fermented milk products enriched with plant sterols served as the basis for recommendations for the widespread use of “functional” products for non-drug correction of cholesterol and LDL cholesterol levels, first in Finland, then in other regions of Europe, as well as in North America. They began to appear in Russia.
One such product is Danacor. The effectiveness of this product was evaluated in five multicenter, double-blind, placebo-controlled studies involving more than 500 patients, conducted both in our country and abroad.
In one of the studies, 40 patients with coronary artery disease and hypertension were divided into two representative groups: the main group (18 people) and the comparison group (22 people). Patients were assigned to groups by lottery, a randomized, double-blind study. All patients received a calorie-reduced hyposodium antiatherogenic diet during the 3-week study period. Patients in the main group received the fermented milk product Danacor, 100 ml (one bottle) per day, for 3 weeks while on a diet. Patients in the comparison group received a diet containing placebo at the same dose. The comparison product (placebo) was identical in composition and nutritional value, but did not contain phytosterols.
The results of biochemical studies (table) showed that enrichment of the basic anti-atherogenic diet with a fermented dairy product containing phytosterols had an additional lipid-lowering effect and contributed to a statistically significant decrease in the level of total cholesterol (TC) from 6.29 ± 0.15 mmol/l to 5. 04 ± 0.15 mmol/l (p < 0.001), LDL cholesterol levels - from 4.16 ± 0.16 mmol/l to 3.15 ± 0.14 mmol/l (p < 0.01), decreased levels TG from 1.74 ± 0.16 mmol/l to 1.51 ± 0.12 mmol/l, VLDL cholesterol - from 0.73 ± 0.06 mmol/l to 0.64 ± 0.05 mmol/l and the value of the atherogenic coefficient - from 3.75 ± 0.25 to 3.25 ± 0.24.
In patients in the comparison group, the level of total cholesterol as a result of the course of diet therapy decreased less significantly than in the main group: from 6.25 ± 0.14 mmol/l to 5.54 ± 0.20 mmol/l (p < 0.05). Decrease in LDL cholesterol level - from 4.18 ± 0.10 mmol/l to 3.56 ± 0.17 mmol/l (p < 0.05). Serum concentrations of TG, VLDL cholesterol and the value of the atherogenic coefficient remained virtually unchanged.
Enrichment of the basic diet of patients with CVD with phytosterols also had a beneficial effect on the condition of the hepato-biliary tract. This could be judged by a noticeable decrease after the course of diet therapy in the levels of AST (from 36.6 ± 9.8 IU/l to 26.2 ± 3.00 IU/l), ALT (from 48.5 ± 14.3 IU /l to 35.4 ± 5.06 IU/l) and total bilirubin (from 15.8 ± 1.02 mmol/l to 13.4 ± 0.92 mmol/l). In patients in the comparison group, the dynamics of these indicators were somewhat less pronounced.
Reliable data were obtained between the groups of patients compared in the study as a result of treatment on the dynamics of changes in the level of total cholesterol (t = 2.35, p < 0.05), the value of the atherogenicity coefficient (t = 2.88, p < 0.01) and prothrombin activity (t = 2.23, p < 0.05).
Thus, the inclusion of phytosterols in an antiatherogenic diet has a beneficial effect on the clinical picture of CVD, does not have a negative effect on vitamin supply and enhances the lipid-lowering effect of the diet, which is manifested by a more significant decrease in the blood serum levels of total cholesterol, triglycerides, LDL cholesterol, VLDL cholesterol and the value of the coefficient atherogenicity (by 8–10%) than in patients in the comparison group. Clinical and biochemical parameters confirmed the safety of products containing sterol esters for the functional state of the liver. The results obtained indicate that these functional products can be used for the primary non-drug correction of lipid metabolism disorders.
A. V. Pogozheva , Doctor of Medical Sciences, Professor S. A. Derbeneva , Candidate of Medical Sciences, State Research Institute of Nutrition of the Russian Academy of Medical Sciences, Moscow
For questions regarding literature, please contact the editor.
Indications for use
Nutritionists, together with specialized cardiologists, as well as endocrinologists, have developed a standard hypocholesterol diet, which must be used in the event of the development of such serious pathologies in the body:
- Pathology of the blood flow system - atherosclerosis;
- Ischemia of the cardiac organ;
- High blood pressure index - hypertension;
- Hypercholesterolemia;
- Dyslipidemia of a genetic nature;
- Disruption of the endocrine organs - diabetes mellitus;
- Pathologies of the cardiac organ;
- Diseases of the blood flow and hematopoiesis system.
The index of lipoprotein increase is influenced by the following provoking factors:
- Excess weight - obesity;
- Genetic hereditary predisposition;
- Alcoholism;
- Nicotine addiction;
- High blood pressure index;
- High blood glucose index;
- Physical inactivity;
- Constantly interrupting a person in a stressful situation;
- Poor nutrition;
- Taking certain medications.
A hypocholesterolemic diet should not be used during pregnancy for a woman, as well as during the period of feeding a baby with breast milk.
Children are also prohibited from using an anti-cholesterol diet.
How to make your diet as healthy as possible?
In order for the diet to be as healthy as possible, it is necessary to take a variety of foods every day that will help reduce the cholesterol index and not cause a feeling of constant hunger:
- Using soy in cooking , you can achieve the maximum speed of reducing lipids in the body, because soy products speed up the absorption and processing of food;
- With a hypocholesterolemic diet, eat several nuts constantly throughout the day . This will make it possible to satisfy hunger, and vegetable protein helps reduce cholesterol. Nuts also contain sterol, vitamin E, vegetable fat and fiber, which has a beneficial effect on the condition of the entire body;
- Barley and oatmeal provide the necessary intake of beta-glucans , which prevents low molecular weight cholesterol from entering the blood;
- Fresh vegetables , as well as fruits and garden herbs, provide the body with fiber and help remove harmful cholesterol from the body;
- Vegetable oils strengthen the inner membrane of the choroid, which prevents damage.
In addition to adjusting your diet, you also need to change your usual lifestyle and get rid of bad habits. By giving up nicotine addiction and alcohol use, you can also reduce your cholesterol index, and in combination with a hypocholesterolemic diet, achieve good results.
Also, do not forget about physical activity on the body; daily exercise and walking can speed up the process of reducing the level of lipoproteins in the blood plasma.
What is it used for?
Cholesterol in the human body is a very important building element for all cell membranes.
If fat-containing alcohol does not exceed standard values, then the lipid process in the body occurs normally, and a person should not go on a cholesterol-lowering diet.
You just need to adhere to the basic rules of a healthy diet and eat less foods containing natural animal fat.
If the total cholesterol level is higher than the standard level of 5.5 mmol per liter of blood, then you should think about it, because there is an excess of lipoprotein molecules in the blood. This excess cholesterol affects the heart organ as well as the blood flow system of the human body.
If you do not use a hypocholesterolemic diet in the fight against a high cholesterol index in the blood, then this is fraught with the development of such pathologies in the body that are dangerous due to their complications and consequences:
- Atherosclerosis;
- Phlebeurysm;
- Thrombosis of large diameter arteries;
- Trophic ulcer;
- Stagnation of blood in the pulmonary artery and organs;
- Failure of the heart organ;
- Improper functioning of the heart valve apparatus;
- Cardiac arrhythmia;
- Arterial aneurysm.
To avoid the development of these pathologies and their transition to a complicated form of heart attacks or strokes, a hypocholesterolemic diet has been developed.